Abstract
Background
Urticarial dermatitis, which is characterised by persistent wheals with eczematous papules and plaques, is frequently misdiagnosed and difficult to treat. Patients commonly experience intolerable pruritus which may greatly affect their quality of life.
Objective
The objective of this study is to characterize the clinical patterns of pruritus in patients with urticarial dermatitis and to determine the effectiveness of cyclosporine treatment.
Methods
This prospective study included 50 histopathologically confirmed patients with urticarial dermatitis. A face-to-face structured questionnaire was given to all patients, and they were treated with low-dose cyclosporine (1~3 mg/kg/d) for at least 2 weeks.
Results
The majority of patients (80.0%) had moderate to severe pruritus. Most patients experienced exacerbation of the itch in the evening (74.0%), with the extremities (upper, 86.0%; lower, 94.0%) being the most commonly involved sites. Due to severe pruritus, patients complained about reduced social contact, quality of life and difficulties in falling asleep et al. Cyclosporine significantly reduced the mean itch score and extent of erythema, and improved interference with daily activities and sleep.
Clinical features of urticarial dermatitis consist of heavily itchy erythematous papules and plaques resembling urticaria with or without eczematous features. Up until now, the detrimental effects on the quality of life of subjects with urticarial dermatitis were not well understood and there is no study about the characteristics of itch. Although the optimal treatment for urticarial dermatitis remains to be solved, there have been several reports about various therapeutic trials using topical or systemic steroids, antihistamines, dapsone, mycophenolate mofetil or phototherapy in the literature123. Therefore, this study aimed to investigate the characteristics of itch and to evaluate the therapeutic effects of low-dose cyclosporine for urticarial dermatitis.
In total, 50 patients (aged ≥18 years) consistent with the diagnosis of urticarial dermatitis and who showed unsatisfactory therapeutic response to systemic steroid or antihistamines at local clinic were prospectively enrolled at the dermatologic clinic of Pusan National University Hospital between January 2012 and April 2013. Urticarial dermatitis was defined by the strict criteria of previously published studies12. Requirements for a diagnosis of urticarial dermatitis included both clinical and histopathologic characteristics which were outlined by Kossard et al.2 in 2006. Clinical criteria were both eczematous and urticarial lesions lasting longer than 24 hours. Histologic criteria were as follow: dermal inflammation with eosinophils limited to the papillary dermis with minimal spongiosis (Fig. 1). Detailed medical history recording, histopathologic examination, direct immunofluorescence and blood analysis were carried out to confirm the diagnosis. Differential diagnoses (e.g., eczema, urticaria, urticarial vasculitis, herpes gestationis or dermatitis herpetiformis, etc.) were ruled out by patients' medical history, physical exam, histopathologic findings or laboratory evaluation at their first visit. Written informed consent was obtained from all subjects after explaining the nature of the study, which was conducted according to the ethical standards of the Bioethical Committee of Pusan National University Yangsan Hospital (IRB no. 05-2015-075) and it was also performed in accordance with the Declaration of Helsinki.
To characterize the itch profile, a face-to-face structured questionnaire concerning pruritus (location, cutaneous lesions other than wheals, intensity, frequency, and diurnal variation) was conducted. The questionnaire also included the affective descriptors and consequent events resulting from the itch itself with the purpose of evaluating the quality of life matters and social activities. Respondents expressed their agreement with each statement by checking the corresponding boxes.
All patients received low-dose cyclosporine (1~3 mg/kg/d) for at least 2 weeks. If patient reports a marked improvement in symptoms in response to cyclosporine, we adjusted the dose of medication to 1 mg/kg/d. Otherwise, if there wasn't any apparent improvement, authors instructed patients to take the same dose of cyclosporine. The use of topical corticosteroids and antihistamines was prohibited for all patients who were enrolled throughout the study. At every visit, the intensity of pruritus, extent of erythema and interference with daily activities and sleep were evaluated. The evaluation of pruritus intensity and interference with daily activities and sleep (over the last 24 hours) were classified and evaluated with a 4-point scale as 0=none, 1=mild, 2=moderate, and 3=severe. The extent of erythema as a measure of clinical response to cyclosporine was defined as the percentage of area covered by erythematous lesions at every visit and it was divided into a 4-point scale as 0=≤30%, 1=31%~50%, 2=51%~75%, and 3=>75%. Any patient with adverse effects were recorded at each clinical visit. Cyclosporine was discontinued when patients experienced a complete clearance of clinical signs and symptoms and followed-up for 2 months more after stopping medication of cyclosporine.
A total of biopsy-proven 50 patients completed the clinical assessments including the questionnaire. The mean age±standard deviation of the respondents was 52.5±17.7 years. Among the respondents, 17 were men (34.0%) and 33 were women (66.0%). Thirty-five patients had no known comorbidities, whereas 6 and 3 patients had a history of hypertension and diabetes, respectively.
Among the 50 patients with urticarial dermatitis, 40 patients (80.0%) complained of an itch considered moderate to severe, and 46 patients (92.0%) reported often or always experiencing an itching sensation. Most patients experienced exacerbation of the itch in the evening (74.0%), with the extremities (upper, 86.0%; lower, 94.0%) being the most commonly involved sites. Additional characteristics of pruritus in our patients are listed in Table 1. The affective descriptors and consequent events were analysed in Table 2. More than half of the patients reported having experienced reduced social contact, quality of life and daily activities due to pruritus. Difficulties in falling asleep and frequently waking were often observed. However, patients with urticarial dermatitis seldom need sleeping pill and lose their appetite.
The mean duration of treatment with cyclosporine was 4.3±2.7 weeks. The mean dose of cyclosporine was 2.96 mg/kg/d for the first 2 weeks, and 1.63 mg/kg/d and 1.04 mg/kg/d for 2 to 4 weeks and 4 to 6 weeks, respectively. The mean intensity score of pruritus was significantly reduced after 4 and 6 weeks of treatment (p=0.002, and <0.0001, respectively) compared with that of baseline. The interference with sleep was also significantly decreased at weeks 4, and 6 (p=0.020 and 0.012, respectively). Furthermore, erythema extent and interference with daily activities were reduced with statistical significance (p<0.0001 and p=0.005, respectively) after 2 weeks of cyclosporine therapy (Fig. 2, Table 3).
Only 6.0% (n=3) of all patients reported adverse events including general weakness, irregular menstruation and nausea during the treatment. However, none of the adverse events was severe enough to stop using cyclosporine.
All patients were available for follow-up telephone surveys 8 to 10 weeks after discontinuation of cyclosporin. Three patients had continued to take cyclosporin for 4 weeks and did not notice any relapse of symptoms or signs of the disease, whereas 2 patients who took medication only for 2 weeks experienced relapse within 10 weeks. Forty eight out of 50 patients remained free of the disease for at least 8 weeks after the discontinuation of cyclosporine.
From 50 patients with histopathologically proven urticarial dermatitis, we performed the study to highlight the clinical characteristics of pruritus in patients with urticarial dermatitis and also accessed the efficacy of cyclosporine. Urticarial dermatitis is a novel clinical and histological term used to describe patients showing a specific, evident dermal hypersensitivity reaction pattern123. In 2006, Kossard et al.2 defined urticarial dermatitis as a subset of dermal hypersensitivity reactions with clinically relevant characteristics compared with alternative, differential diagnoses. Skin biopsy is often required to differentiate these disorders and histopathological findings of urticarial dermatitis commonly show minimal epidermal spongiosis and perivascular inflammation of lymphohistiocytes and a few eosinophils, without evidence of vasculitis45. With regard to the cutaneous findings, most patients of urticarial dermatitis had urticarial component which could last for days, whereas the true urticarial wheals usually resolve in less than 24 hours1. In the current study, we included only subjects who presented with clinically typical lesions of urticarial dermatitis, as confirmed by histopathological analyses.
Recently, Hannon et al.1 reported that the most commonly involved sites in urticarial dermatitis were the trunk (90%) and lower extremities (82%). Conversely, in the present study, we found that the upper (86%) and lower extremities (94%) were more commonly involved than the trunk (80%). This can be a new and helpful diagnostic clue when we encounter the patients who have cutaneous lesions only on extremities.
Among 50 urticarial dermatitis patients, 40 (80%) responded that they experienced itch intensity as moderate or severe. Further 45 (90%) of 50 patients felt itch often or always during the day. These findings implicate that dermatologists who are dealing with itch symptom in patients with urticarial dermatitis need prudent approach.
It has been established that pruritus associated with common dermatologic diseases typically intensifies at night6. In the present study, 18% of patients with urticarial dermatitis experienced itch right after getting up in the morning, and 28% of subjects experienced worsening of the itch in the afternoon. However, similar to that in other dermatological diseases45678, the period during which most patients (74%) experienced pruritus was found to be in the evening. Thus, the mechanisms of itch in urticarial dermatitis might be similar to those of typical nocturnal itch, which involves temporal regulation of the immunoglobulin E/mast cell-mediated intrinsic clockwork or mediators of circadian rhythm7. However, the mechanisms behind itching sensation specifically in the morning or afternoon are not well understood.
Patient-based outcomes associated with itch are critical for clinical dermatologists to evaluate, and yet, the impact of the itch itself on these outcomes is poorly understood. Our results suggest that patients with urticarial dermatitis perceive negative sequelae not only from the cutaneous lesions, but also from the pruritus, with pruritus reportedly causing scratching and reduced social contact and daily activities in the majority of patients. Moreover, 40% of patients also reported having difficulties falling asleep as a result of the itch. However, our results showed that once the patients were asleep, they did not easily awaken due to itching. A total of 86% of patients did not require sleeping pills, and 50% of patients did not experience change in behaviour toward others due to their urticarial dermatitis.
In terms of refractory itch, we measured and clarified the characteristics of itch and quality of life in urticarial dermatitis using the Leuven itch scale8. Although there are some reports regarding the clinical characteristics of urticarial dermatitis in the dermatologic literature, no clinical study focusing on the characteristics of the itch associated with this condition has been conducted.
Urticarial dermatitis has been known to represent a therapeutic challenge using conventional treatments such as systemic steroid or antihistamines9. As urticarial dermatitis involves cutaneous lesions reminiscent of both urticaria and eczema, we hypothesised that treatment with cyclosporine might be effective910. As the main target of cyclosporine is the helper T cells, we speculated that the depletion of lymphocytes and macrophages in epidermis and dermis, and inhibition of histamine release from the mast cells might have contributed to the improvement of symptoms in urticarial dermatitis111. The therapeutic efficacy of cyclosporine in the current study was evaluated objectively by examination of the erythematous lesion, and subjectively by the evaluation of symptoms such as itch intensity and interference with daily activities and sleep. The intensity of pruritus and interferences with sleep were significantly decreased after 4 weeks treatment with cyclosporine compared with that at baseline. However, the extent of erythema and interference of daily activities were more rapidly improved at week 2 with statistical significance. From these results, we speculated that cutaneous lesions including erythema might mainly have influenced daily activity for patients.
There are several limitations in the study. First, this study lacked a control group, and secondly, the subject sample size was relatively small.
In present study, adverse events during treatment with cyclosporine included irregular menstrual period, nausea, and general weakness in 3 patients only. These adverse events were all transient and did not interrupt the study design.
In conclusion, to the best of our knowledge, this is the first prospective study designed to identify the characteristics of itch and therapeutic efficacy of cyclosporine for urticarial dermatitis12. Based on our findings, we recommend a low-dose cyclosporine as a useful treatment option for urticarial dermatitis.
Figures and Tables
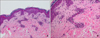 | Fig. 1Histological examination of a skin biopsy specimen from patient 3 showed minimal epidermal spongiosis and superficial perivascular infiltration of lymphocytes and eosinophils in upper dermis (H&E; A: ×100, B: ×400). |
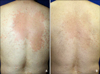 | Fig. 2(A) Representative image of erythematous wheals and papules on the back were observed at the first visit. (B) After treatment with low-dose cyclosporine for 2 weeks, only mild post-inflammatory hyper pigmentation left remained, with resolution of pruritus is observed. |
Table 1
Characteristics of itch at baseline in patients with urticarial dermatitis (n=50)

Table 2
Affective descriptors and consequent events associated with pruritus in patients with urticarial dermatitis (n=50)
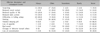
Table 3
Therapeutic efficacy of cyclosporine on urticarial dermatitis

References
1. Hannon GR, Wetter DA, Gibson LE. Urticarial dermatitis: clinical features, diagnostic evaluation, and etiologic associations in a series of 146 patients at Mayo Clinic (2006~2012). J Am Acad Dermatol. 2014; 70:263–268.

2. Kossard S, Hamann I, Wilkinson B. Defining urticarial dermatitis: a subset of dermal hypersensitivity reaction pattern. Arch Dermatol. 2006; 142:29–34.
3. Lee JS, Loh TH, Seow SC, Tan SH. Prolonged urticaria with purpura: the spectrum of clinical and histopathologic features in a prospective series of 22 patients exhibiting the clinical features of urticarial vasculitis. J Am Acad Dermatol. 2007; 56:994–1005.

4. Peroni A, Colato C, Zanoni G, Girolomoni G. Urticarial lesions: if not urticaria, what else? The differential diagnosis of urticaria: part II. Systemic diseases. J Am Acad Dermatol. 2010; 62:557–570.

5. Kazmierowski JA, Chusid MJ, Parrillo JE, Fauci AS, Wolff SM. Dermatologic manifestations of the hypereosinophilic syndrome. Arch Dermatol. 1978; 114:531–535.

6. Erturk IE, Arican O, Omurlu IK, Sut N. Effect of the pruritus on the quality of life: a preliminary study. Ann Dermatol. 2012; 24:406–412.

7. Patel T, Ishiuji Y, Yosipovitch G. Nocturnal itch: why do we itch at night? Acta Derm Venereol. 2007; 87:295–298.

8. Haest C, Casaer MP, Daems A, De Vos B, Vermeersch E, Morren MA, et al. Measurement of itching: validation of the Leuven Itch Scale. Burns. 2011; 37:939–950.

9. Chaptini C, Sidhu S. Mycophenolate mofetil as a treatment for urticarial dermatitis. Australas J Dermatol. 2014; 55:275–278.

10. Asero R. Oral cyclophosphamide in a case of cyclosporin and steroid-resistant chronic urticaria showing autoreactivity on autologous serum skin testing. Clin Exp Dermatol. 2005; 30:582–583.

11. Tedeschi A, Airaghi L, Lorini M, Asero R. Chronic urticaria: a role for newer immunomodulatory drugs? Am J Clin Dermatol. 2003; 4:297–305.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download