Abstract
Background
Demodicosis is a parasitic skin disease caused by Demodex mites, and the determination of mite density per square centimeter is important to diagnose demodicosis. Standardized skin surface biopsy (SSSB) and direct microscopic examination (DME) are commonly used to determine Demodex mites density (Dd). However, no study has previously compared these two methods with respect to clinical types and distribution patterns of demodicosis.
Objective
The aim of this study was to compare the value of SSSB and DME findings in reference to the clinical types and distribution patterns of demodicosis.
Methods
The medical records of 35 patients diagnosed with demodicosis between December 2011 and June 2015 were retrospectively reviewed. Demodicosis was classified according to four clinical types (pityriasis folliculorum, rosacea type, acne type, and perioral type) and three distribution patterns (diffuse pattern, U-zone pattern, and T-zone pattern). Two samples, one for SSSB and one for DME, were obtained from a lesion of each patient.
Results
In all patients, mean Dd and the proportion with a high Dd (>5D/cm2) by DME (14.5±3.3, 80.0%, respectively) were higher than by SSSB (5.5±1.3, 37.1%, respectively; p<0.01, p=0.02, respectively). In terms of clinical types, for rosacea type, mean Dd and proportion with a high Dd by DME (12.4±3.5, 84.6%, respectively) were significantly greater than those determined by SSSB (3.6±1.2, 23.1%; p=0.04, p=0.04, respectively). In terms of distribution pattern, for the diffuse pattern, mean Dd and the proportion with a high Dd by DME (17.5±3.7, 100%, respectively) were significantly higher than those determined by SSSB (6.0±2.7, 26.7%; p<0.01, p<0.01, respectively).
Demodicosis is a parasitic skin disease caused by Demodex folliculorum and/or Demodex brevis. D. folliculorum resides in hair follicles, and D. brevis in the infundibulum of sebaceous glands. These mites both routinely inhabit human skin with a prevalence of up to 100%, and are considered to be pathogenic when present in excessive numbers123 or when they penetrate dermis45.
Demodex has various clinical manifestations, that is, papulopustular rosacea26789, pityriasis folliculorum310, granulomatous rosacea41112, perioral dermatitis-like demodicosis13, blepharitis141516, and pustular folliculitis1718.
Demodex mite densities can be measured in different ways and the presence of >5 mites per cm2 is required for a diagnosis of demodicosis. Two methods are commonly used to determine Demodex mite densities–a standardized skin surface biopsy (SSSB) and direct microscopic examination (DME). A recent study found SSSB is more effective than DME for detecting Demodex19, but no study has previously compared the two methods with respect to the clinical types and distribution patterns of demodicosis. Accordingly, the aim of this study was to compare measures of Demodex mite densities obtained using SSSB and DME in terms of their relations with clinical types and distribution patterns.
Thirty-five patients with demodicosis attending the Department of Dermatology, Gachon University Gil Medical Center, Gachon University School of Medicine, Incheon, Korea, between December 2011 and June 2015, were retrospectively studied. Institutional review board approval was obtained from the institutional review committee of the Gachon University Gil Medical Center (IRB no. GAIRB-2015-288).
Demodex has various clinical features, and in the present study, demodicosis was classified into four clinical types based on the literature and clinical experience, as follows: (1) Pityriasis folliculorum is observed as erythema of the face with follicular plugging and discreet fine, whitish scale2021; (2) rosacea type consists of papulopustules involving the face in patients with or without pre-existing inflammatory dermatoses, such as, rosacea2122; (3) acne type is described as localized follicular pustules without scale clinically mimicking acne vulgaris18; and (4) perioral type is described as papulopustules involving the perioral area with or without pre-existing inflammatory dermatoses23.
We also classified demodicosis into three distribution patterns: (1) the diffuse pattern exhibits lesions evenly distributed over the entire face; (2) the U-zone pattern has lesions mainly on the cheeks, jawline, and chin; and (3) the T-zone pattern has lesions dominantly distributed on the forehead, nose, and the central portion of the chin.
SSSB and DME were used to measure Demodex mites density (Dd). For SSSB, a standard area of 1 cm2 was drawn on a slide with a waterproof pen. A drop of cyanoacrylic adhesive was then placed on the other side of the slide and the adhesive-bearing surface was applied to the skin for one minute. After allowing the adhesive to dry, the slide was removed gently with surface skin, clarified with one to two drops of immersion oil, and covered with a cover slip. For DME, a 1 cm2 sized affected skin area was squeezed using a comedo extractor. The sample obtained was transferred to a 10% potassium hydroxide drop and covered with a cover slip. Samples obtained using both methods were studied under an optical microscope (×40, ×100).
The collected data were analyzed by using SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA). Results for qualitative variables are expressed as numbers and percentages, and for quantitative variables as means and standard deviations and standard error. Data normality was evaluated using the Kolmogorov-Smirnov test. Fischer's exact test was used for intergroup comparisons of qualitative data, and the Mann-Whitney test and the Kruskal-Wallis test were used for intergroup comparisons of quantitative data. McNemar's test and Wilcoxon's signed rank test were used determine the significances of differences between DME and SSSB results. For all statistical tests, significance was accepted for p-values<0.05.
Demodicosis was more prevalent in women (28, 80.0%) than in men (7, 20.0%). Overall mean patient age was 43.5 years and ranged from 19 to 60 years. Most of the 35 patients (88.6%) were aged between 31 and 60 years (Table 1). The most common clinical type was pityriasis folliculorum 20 (57.1%), followed by rosacea type 13 (37.1%), perioral type 1 (2.9%), and acne type 1 (2.9%). The prevalence distribution patterns were: diffuse 15 (42.9%), U-zone 13 (37.1%), and T-zone 7 (20.0%).
Mean ages of patients with pityriais folliculorum or rosacea type were 42.8 years (range, 19~60 years) and 46.5 years (range, 25~57 years), respectively, and ages were not significant different (p=0.3; Table 2). No significant differences were observed between the ages of patients with one of the three distribution patterns: U-zone pattern (mean=42.8 years; range, 19~58 years), T-zone pattern (mean=45.0 years; range, 25~60 years), and diffuse pattern (mean=43.3 years; range, 25~58 years; p=0.9).
In the 35 patients, DME identified >5D/cm2 mites in 28 patients (80.0%) and SSSB in 13 patients (37.1%; p=0.02). Mean Dd by DME (14.5±3.3) was greater than mean Dd by SSSB (5.5±1.3), and this difference was statistically significant (p<0.01; Table 3).
Of the patients diagnosed with pityriasis folliculorum or rosacea type, mean Dd values by DME (16.8±5.3 and 12.4±3.5, respectively) were higher than for SSSB (6.8±2.1 and 3.6±1.2, respectively), but the difference was statistically significant only for rosacea type (p=0.1, p=0.04, respectively). The numbers of patients with pityriasis folliculorum or rosacea type diagnosed by DME (15 and 11 patients, respectively) were greater than numbers diagnosed by SSSB (9 and 3 patients, respectively), and again the difference was significant only for rosacea type (p=0.2, p=0.04, respectively).
In terms of distribution patterns, mean Dd values were higher for DME than for SSSB, but the difference was significant only for the diffuse pattern: 17.5±3.7 by DME and 6.0±2.7 by SSSB for the diffuse pattern (p<0.01), 9.5±3.0 by DME and 3.4±1.1 by SSSB for the U-zone pattern (p=0.1), and 17.0±13.9 by DME and 8.1±1.7 by SSSB for the T-zone pattern (p=0.6). With the exception of the T-zone pattern, the number of cases with a Dd of >5D/cm2 was greater for DME. However, the difference was significant only for the diffuse pattern: 15 by DME and 4 by SSSB for the diffuse pattern (p<0.01), 10 by DME and 3 by SSSB for U-zone pattern (p=0.1), and 2 by DME and 6 by SSSB for the T-zone pattern (p=0.2).
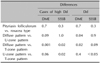
Comparing pityriasis folliculorum with rosacea type, no significant difference was observed between mean Dd values of the proportions with a high Dd (p=0.3, p=0.3, respectively; Table 4). In terms of distribution patterns, the mean Dd by DME for the diffuse pattern was significantly than mean Dd values for the U-zone and T-zone patterns (p=0.04, p=0.02, respectively), and the proportion with a high Dd by DME was significantly higher for the diffuse pattern than for the T-zone pattern (p=0.001). Mean Dd by SSSB was significantly higher for the T-zone pattern than for the U-zone pattern (p<0.05), and the proportion with a high Dd by SSSB was significantly greater for the T-zone pattern than for the U-zone pattern (p=0.02) or the diffuse pattern (p=0.02).
Demodicosis is a skin disease of pilosebaceous units caused by the human Demodex mites D. folliculorum and/or D. brevis3. D. folliculorum and D. brevis are obligatory parasites of the pilosebaceous units in human skin18. D. folliculorum is usually found in the infundibular portion of hair follicles, whereas D. brevis thrives in sebaceous ducts, Meibomian glands, and in the deeper parts of hair follicles.
The pathogenesis of human demodicosis is largely unknown. It is supposed to be pathogenic role when follicles become heavily infested or mites penetrate dermal tissue 12345. It is considered that Demodex proliferation is related to age, sebum production, hypervascularized ground, hygiene, immune status, and genetic factors.
Demodex mites are found on the skins of demodicosis affected and healthy individuals, and thus, diagnosis requires the presence of compatible clinical manifestations and a high Dd (>5/cm2). Various methods have been used to detect Demodex mites, for example, SSSB, skin biopsy, hair epilation, DME, cellophane tape, and reflectance confocal microscopy. Sampling methods can influence Demodex infestation results. Of these methods, SSSB and DME are commonly used because they are convenient and allow mite densities to be easily measured.
SSSB is non-invasive and also enables analysis of an important part of the D. folliculorum biotope in a reproducible manner25. However, some limitations of SSSB have been reported in the literature2526. In particular, it is conducted on the superficial portions of the horny layer and follicles, but does not include entire follicles. Furthermore, false-negative or suboptimal results can occur in patients with elongated and hyperkeratotic follicles or seborrheic skin due to poor adherence of mites to slides25. Quality of sampling is dependent on the preconditioned status of skin, for example, whether or not skin is cleaned with ether20. This process is usually repeated twice to avoid false-negative results. However, a second SBBB at same sites would probably induce bleeding in patients with thin skin27.
DME requires samples from follicular papules or pustules by squeezing, and is more invasive and painful than SSSB. Thus, DME can be dependent on examiner's skill and patient compliance. However, it allows the collection of superficial portions of follicles, and also samples sebaceous glands, deeper portions of hair follicles, and intact papules and pustules. Hence, SSSB can detect only D. folliculorum, whereas DME can detect both D. folliculorum and D. brevis.
According to Aşkin and Seçkin19, mean Dd by DME in patients with a diagnosis of demodicosis was lower than that obtained by SSSB, and the proportion of patients with a high Dd by DME was comparatively low. However, our data show DME (80.0%) was more sensitive than SSSB (37.1%) for all 35 patients and for patients of the rosacea type (84.6% by DME and 23.1% by SSSB) and patients with a diffuse pattern (100% by DME and 26.7% by SSSB).
In contrast to previous study19, we consider DME is probably better at detecting mites than SSSB. First, DME is not influenced by skin types like hyperkeratotic follicles or seborrheic skin, because it obtains samples by squeezing. Second, SSSB can detect mites at small follicular scales, ruptured papules or pustules, but hard to detect mites at intact papules and pustules. However, DME can detect mites regardless of skin lesions. Third, SSSB can fail to detect mites in sebaceous glands and in the deeper parts of hair follicles where D. brevis resides. DME allows examination of deeper skin regions, which increases opportunity for D. brevis detection.
For the rosacea type, DME was significantly more sensitive than SSSB. We believe this difference between DME and SSSB in rosacea type is probably due to the lower detection rate of SSSB. Forton et al.20 supposed that older age and the consequential decline of immune response in pityriasis folliculorum leads to a larger proliferation of the mite, and the more severe immune response in rosacea type resists the mite proliferation. However, in the present study, ages between the two clinical types were not significantly different.
We believe two possible reasons, which differ from those suggested by Forton et al.20, for this result. The first is that pityriasis folliculorum is usually caused by the more superficially living D. folliculorum, whereas rosacea type is commonly associated with the deep living D. brevis24. The second is that measurements are usually performed using severe lesions. When dermatologists examine Demodex, measurements at usually made using severe follicular scale, papules, or pustules regardless of clinical types. The size of papules and pustules depends on depth of infiltration28, and thus, the severe papules or pustules are probably more related to the proliferation of Demodex, which penetrates deeply into hair follicles or dermis. This means that the test on severe lesion in patients with suspected rosacea type may affect mites detection by SSSB. Therefore, SSSB, which analyzes only superficial skin, has a lower detection rate for rosacea type than pityriasis folliculorum.
Interestingly, SSSB was significantly more sensitive for the T-zone pattern than other distribution patterns. One possible explanation is that increased sebum secretion and dilated follicles in lesions of the T-zone result in the proliferation of D. folliculorum. Demodex infestation is related to sebum secretion29, and sebum secretion levels are positively correlated with follicular dilation30. The forehead and nose regions secrete more sebum than other facial regions and follicles are more dilated31. Aylesworth and Vance32 revealed follicular dilation is not associated with D. brevis proliferation, but that it does affect D. folliculorum survival. They also found higher prevalences of D. folliculorum infestation in the forehead and nose region than on the cheeks and chin region. This finding concurs with those of Akilov et al.24, who concluded D. folliculorum is more likely to cause demodicosis in the facial T-zone. These results indicated that the development of sebum secretion and the dilation of follicle in the T-zone are attributable to the proliferation of D. folliculorum, and that this increases the detection rate of SSSB.
This study has several limitations. In particular, it was conducted using a retrospective design based on medical records, and D. folliculorum and D. brevis were not differentiated. Another limitation of this study was the small sample size ant it was probably responsible for some of our non-significant results. And because of the limited number of patients with acne type or perioral type, statistically analysis was not performed.
Finally, we propose that DME is the more appropriate method for measuring Demodex densities, especially in patients with diffuse distribution pattern and or suspected of having rosacea type. Further controlled comparative studies on a large number of cases, possibly prospective, are needed in order to confirm the results of the present study.
Figures and Tables
Table 1
Numbers of cases according to clinical parameters (n=35)

Table 2
Comparisons of ages by clinical types and distribution patterns
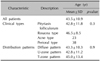
Table 3
Comparisons of DME and SSSB results by clinical types and distribution patterns
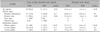
Table 4
Comparision of DME and SSSB between clinical types and between distribution patterns
References
2. Bonnar E, Eustace P, Powell FC. The Demodex mite population in rosacea. J Am Acad Dermatol. 1993; 28:443–448.

3. Ayres S Jr, Ayres S 3rd. Demodectic eruptions (demodicidosis) in the human. 30 years' experience with 2 commonly unrecognized entities: pityriasis folliculorum (Demodex) and acne rosacea (Demodex type). Arch Dermatol. 1961; 83:816–827.
5. Hoekzema R, Hulsebosch HJ, Bos JD. Demodicidosis or rosacea: what did we treat? Br J Dermatol. 1995; 133:294–299.

6. Forton F, Seys B. Density of Demodex folliculorum in rosacea: a case-control study using standardized skin-surface biopsy. Br J Dermatol. 1993; 128:650–659.

7. Abd-El-Al AM, Bayoumy AM, Abou Salem EA. A study on Demodex folliculorum in rosacea. J Egypt Soc Parasitol. 1997; 27:183–195.
8. Erbağci Z, Ozgöztaşi O. The significance of Demodex folliculorum density in rosacea. Int J Dermatol. 1998; 37:421–425.
9. el-Shazly AM, Ghaneum BM, Morsy TA, Aaty HE. The pathogenesis of Demodex folliculorum (hair follicular mites) in females with and without rosacea. J Egypt Soc Parasitol. 2001; 31:867–875.
10. Ayres S Jr, Mihan R. Rosacea-like demodicidosis involving the eyelids. A case report. Arch Dermatol. 1967; 95:63–66.

11. Grosshans EM, Kremer M, Maleville J. Demodex folliculorum and the histogenesis of granulomatous rosacea. Hautarzt. 1974; 25:166–177.
12. Pena GP, Andrade Filho JS. Is demodex really non-pathogenic? Rev Inst Med Trop Sao Paulo. 2000; 42:171–173.

13. Dolenc-Voljc M, Pohar M, Lunder T. Density of Demodex folliculorum in perioral dermatitis. Acta Derm Venereol. 2005; 85:211–215.

14. Norn MS. Demodex folliculorum. Incidence, regional distribution, pathogenicity. Dan Med Bull. 1971; 18:14–17.
16. Clifford CW, Fulk GW. Association of diabetes, lash loss, and Staphylococcus aureus with infestation of eyelids by Demodex folliculorum (Acari: Demodicidae). J Med Entomol. 1990; 27:467–470.

17. Karincaoglu Y, Bayram N, Aycan O, Esrefoglu M. The clinical importance of demodex folliculorum presenting with nonspecific facial signs and symptoms. J Dermatol. 2004; 31:618–626.

18. Purcell SM, Hayes TJ, Dixon SL. Pustular folliculitis associated with Demodex folliculorum. J Am Acad Dermatol. 1986; 15:1159–1162.

19. Aşkin U, Seçkin D. Comparison of the two techniques for measurement of the density of Demodex folliculorum: standardized skin surface biopsy and direct microscopic examination. Br J Dermatol. 2010; 162:1124–1126.
20. Forton F, Germaux MA, Brasseur T, De Liever A, Laporte M, Mathys C, et al. Demodicosis and rosacea: epidemiology and significance in daily dermatologic practice. J Am Acad Dermatol. 2005; 52:74–87.

21. Chen W, Plewig G. Human demodicosis: revisit and a proposed classification. Br J Dermatol. 2014; 170:1219–1225.

22. Kim MS, Kim BS, Koh WS, Lee SS, Seo SL, Chun DK, et al. Rosacea: clinical study of 67 cases. Ann Dermatol. 2001; 13:39–43.
23. Hsu CK, Hsu MM, Lee JY. Demodicosis: a clinicopathological study. J Am Acad Dermatol. 2009; 60:453–462.

24. Akilov OE, Butov YS, Mumcuoglu KY. A clinico-pathological approach to the classification of human demodicosis. J Dtsch Dermatol Ges. 2005; 3:607–614.

25. Forton F, Song M. Limitations of standardized skin surface biopsy in measurement of the density of Demodex folliculorum. A case report. Br J Dermatol. 1998; 139:697–700.

26. Forton F. Standardized skin surface biopsy: method to estimate the Demodex folliculorum density, not to study the Demodex folliculorum prevalence. J Eur Acad Dermatol Venereol. 2007; 21:1301–1302. author reply 1302.

27. Forton F, Seys B, Marchal JL, Song AM. Demodex folliculorum and topical treatment: acaricidal action evaluated by standardized skin surface biopsy. Br J Dermatol. 1998; 138:461–466.

28. Forton FM. Papulopustular rosacea, skin immunity and Demodex: pityriasis folliculorum as a missing link. J Eur Acad Dermatol Venereol. 2012; 26:19–28.

29. Zhao YE, Peng Y, Wang XL, Wu LP, Wang M, Yan HL, et al. Facial dermatosis associated with Demodex: a case-control study. J Zhejiang Univ Sci B. 2011; 12:1008–1015.

30. Kim BY, Choi JW, Park KC, Youn SW. Sebum, acne, skin elasticity, and gender difference-which is the major influencing factor for facial pores? Skin Res Technol. 2013; 19:e45–e53.
31. Jung HJ, Suh HY, Shim JH, Li K, Ahn JY, Park MY, et al. Analysis of the distribution of pores and factors affecting facial pores. Korean J Dermatol. 2014; 52:851–857.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download