Abstract
Nodular tuberculid (NT) was originally described by Jordaan et al. in 2000 in 4 patients from South Africa. It appeared as nodules on the legs; the pathologic changes were situated in the deep dermis and adjacent subcutaneous fat. A 34-year-old woman visited our hospital with subcutaneous skin-colored or slightly erythematous round to oval nodules. Skin biopsies revealed granulomatous inflammation at the dermo-subcutaneous junction with vasculitis. Chest X-ray, tuberculosus (TB)-polymerase chain reaction and TB culture of the skin specimen were normal. A QuantiFERON®-TB Gold test (QUIAGEN, Germany) was positive, which suggested a diagnosis of latent TB infection. The patient was treated with anti-TB medication and her condition has not recurred. Herein, we report a case of a patient with latent TB diagnosed by a positive QuantiFERON®-TB Gold test whose skin lesions had the clinical and histopathologic features of NT.
Tuberculosis (TB) remains one of the world's most important communicable diseases. The number of TB cases is slowly declining year by year, but in 2013, according to a report published in 2014, an estimated 9.0 million people developed TB and 1.5 million died from the disease1. The prevalence and mortality of TB in Korea are 146 per 100,000 and 5.4 per 100,000, respectively, which represent the greatest prevalence and mortality among OECD countries2.
Cutaneous TB incidence parallels that of pulmonary TB. The cutaneous lesions of Mycobacterium tuberculosis (MTB) infection have a variety of manifestations. Tuberculids are recurrent skin or mucous membrane lesions in which tuberculous bacillus is absent; they are caused by hypersensitivity to MTB that spreads hematogenously from distant extracutaneous foci. Nodular tuberculid (NT) was identified as a form of tuberculid by Jordaan et al.3 in 2000. NT presents as red to bluish nodules without ulceration. Its main pathologic feature is granulomatous inflammation at the dermo-subcutaneous junction.
To diagnose TB infection in cases with tuberculids, tuberculin skin tests, TB-polymerase chain reaction (PCR), QuantiFERON®-TB Gold test (QUIAGEN, Duesseldorf, Germany), and T SPOT-TB tests are used. The Quanti-FERON®-TB Gold test can diagnose latent TB infection. MTB antigen stimulates T cells, which produce interferon-γ (INF-γ), and the QuantiFERON®-TB Gold test measures the amount of INF-γ. The QuantiFERON®-TB Gold test does not have a booster effect, and is less influenced by the effects of previous bacille Clmette-Guerin (BCG) vaccination, resulting in a lower false negative rate than other tuberculin tests.
We experienced a rare case of female patient with NT, in whom latent TB infection was confirmed by a QuantiFERON®-TB Gold test.
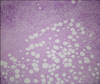
A 34-year-old woman had 7-month history of recurrent skin eruption on both lower extremities and the buttocks. The lesions consisted of multiple tender subcutaneous skin-colored or slightly erythematous round to oval nodules. The lesions did not show any ulcerations or scars (Fig. 1). The patient had no history of trauma, insect bites, or topical use of drugs or cosmetics. Skin biopsy showed dermal necrosis and remarkable fat necrosis with lobular panniculitis. Vasculitis was present in the small- to medium-sized vessels. Diffuse infiltration of foamy histiocytes and mixed cell inflammation were also observed. The pathologic changes were mainly confined to the dermo-subcutaneous junction (Fig. 2, 3, 4). Diastase-treated periodic acid-Schiff (PAS) stain was negative and Ziehl-Neelsen stain failed to reveal acid-fast bacilli. Acid fast bacilli (AFB) culture and TB-PCR of skin tissue samples were negative for MTB. Her husband had a history of incomplete treatment for pulmonary TB, but the patient did not have a history of TB or associated symptoms such as chills, fever, cough, or night sweats. On physical examination, there were no enlarged lymph nodes. Also, findings on a chest radiograph were normal. Her hemoglobin level was 10.8 g/dl, C-reactive protein was 1.36 mg/dl, and erythrocyte sedimentation rate was 46 mm/hr; other laboratory findings were within normal limits. However, a QuantiFERON®-TB Gold test was positive, so a diagnosis of latent TB infection was made. The clinical and pathologic findings of our case are in accordance with tuberculid. We confirmed the diagnosis of NT. The patient was treated with isoniazid (300 mg/day), ethambutol (800 mg/day), and rifampicin (600 mg/day). All skin lesions had disappeared 3 months after anti-TB treatment and she has experienced no recurrence.
Cutaneous lesions associated with MTB infection occur because of direct inoculation of the skin from an exogenous source, autoinoculation, or hematogenous spread. Tuberculids are cutaneous hypersensitivity reactions to MTB from distant extracutaneous foci of infection resulting from hematogenous spread. Tuberculids are recurrent skin or mucous membrane lesions in which tuberculous bacillus is absent. The pathogenesis of tuberculids is the consequence of heightened T-cell-mediated immunity to MTB antigens from an extracutaneous focus in a patient with a moderate or high degree of immunity against MTB.
The characteristics of tuberculids consist of a positive tuberculin test, internal tuberculous involvement, absence of bacillus on mycobacterial cultures or stains of skin specimens, response to anti-TB medications, and specificity in the context of TB4. Although acid-fast stain or culture of the skin lesion is negative, PCR can demonstrate MTB DNA in the biopsy lesion5. Papulonecrotic tuberculid (PNT), erythema induratum of Bazin (EIB), and lichen scrofulosorum (LS) are included in this “tuberculids” group, classically6.
PNT is a symmetric eruption of red papules. The papules of PNT show necrosis and become crusted. The skin lesions of PNT sometimes show spontaneous healing, associated with scars. PNT usually occurs in the acral areas and extensor surfaces of the extremities, buttocks, and lower trunk367. The histopathology of PNT shows leukocytoclastic and lymphohistiocytic vasculitis with wedge-shaped necrosis in the papillary dermis. Necrosis of the papillary dermis extends into the epidermis, but caseous necrosis is absent3.
EIB is a nodular subcutaneous eruption. The lesions of EIB are characterized by tender, recurrent, erythematous, ulcerating skin eruption on the lower extremities, and are most often found in young women. When EIB heals, it leaves an atrophic scar. The histologic features of EIB include diffuse involvement of subcutaneous fat, vasculitis of small vessels, extensive necrosis, and granulomatous inflammation3.
LS is characterized by uncommon lichenoid eruption that is caused by hematogenous spread of mycobacteria in an individual sensitive to MTB6. The lesions of LS are often found on the trunk, mostly in children and adolescents. Asymptomatic, flat-topped yellowish or pink, firm, follicular small lichenoid papules occur in groups, sometimes with scales. Skin eruptions of LS resolve spontaneously without scarring. The histopathologic features of LS can be summarized by lymphohistiocytic to granulomatous inflammation in the upper dermis. Superficial tuberculoid granulomas can be seen around the hair follicles, or can be independent of the adnexa67.
NT is a newly defined type of tuberculid, which was first described in 4 patients from South Africa by Jordaan et al.3 in 2000. A second report of NT involved a female patient with human immunodeficiency virus7. Another, 6th, report of NT was published that involved a male patient with asymptomatic active pulmonary TB48 (Table 1).
Morphologically, the skin lesions of NT are characterized by red to bluish nodules without ulceration. They are usually found in the lower extremities, and measure around 1 cm or larger. NT is found at the dermo-hypodermal junction, not in the papillary dermis, as in PNT, or in the subcutaneous fat, as in EIB. NT has pathological features that are somewhere between those of superficial EIB and deep PNT or LS. Granulomatous inflammation, vasculitis, and necrosis at the junction of the dermis and hypodermis are present.
Our patient had nodular skin eruptions on the lower extremities without redness or ulceration. Histopathologic findings showed granulomatous inflammation at the dermo-hypodermal junction. Chest X-ray and TB-PCR were normal, but QuantiFERON®-TB Gold test was positive, so we identified this as a case of NT. In Korea, there have been several reported cases of tuberculids, including PNT, EIB, LS, and PNT with erythema nodosum, and one case of atypical cutaneous tuberculid in an immunocompromised patient9101112131415. In the latter case, the patient had tuberculous lymphadenitis and multiple discrete, 2~5 mm sized asymptomatic, erythematous to flesh-colored papules on the legs9. To the best of our knowledge, there is no previous report of NT.
A tuberculin skin test is frequently used to diagnose latent TB infection. The results can be affected by immune system or nutritional status, or concomitant corticosteroid use, which can interfere with the interpretation of the results. Moreover, the test is influenced by previous BCG vaccination, so it can be misinterpreted in South Korea where children are routinely given BCG vaccination owing to the high prevalence of TB infection16.
The QuantiFERON®-TB Gold test is an in vitro diagnostic test that measures the amount of INF-γ released when an antigen is used to stimulate the T cells of a patient who is sensitized to MTB. Early-secreted antigenic 6-kDa protein and culture filtrate protein 10 are used as antigens. These antigens are produced from genes located within the “region of difference 1 (RD1)” locus of the genome of MTB, which does not exist in BCG or non-tuberculous mycobacterium1718. The QuantiFERON®-TB Gold is thus a good option for identifying latent TB infection when patients have received a BCG vaccination or are immuno-compromised.
The diagnosis of NT can be delayed because the clinical and histopathologic characteristics of NT are subtler than those of other tuberculids. NT should be included in the classification of cutaneous TB because diagnostic delay may lead to progression of associated TB. We experienced a case of NT in a patient with latent TB, who showed normal findings on chest X-ray and negative findings on TB-PCR. The QuantiFERON®-TB Gold test was positive and the patient's skin lesions showed successful resolution following administration of anti-TB medications. Herein, we report the 7th case of NT in the world and the first in South Korea.
Figures and Tables
Fig. 3
Dense inflammatory cell infiltration around the vessels. Multinucleated giant cells, eosinophils, lymphocytes, foamy histiocytes, and neutrophils are evident (H&E, ×200).
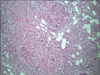
Table 1
Summary of previously reported nodular tuberculid cases including this case

ACKNOWLEDGMENT
The present research was conducted by the research fund of Dankook University in 2014.
References
1. World Health Organization. Global tuberculosis report. World Health Organization;2014. Available from: http://apps.who.int/iris/bitstream/10665/137094/1/9789241564809_eng.pdf.
2. World Health Organization. Global tuberculosis report 2013. World Health Organization;2013. Available from: http://apps.who.int/iris/bitstream/10665/91355/1/9789241564656_eng.pdf.
3. Jordaan HF, Schneider JW, Abdulla EA. Nodular tuberculid: a report of four patients. Pediatr Dermatol. 2000; 17:183–188.

4. Asiniwasis R, Dutil MT, Walsh S. Molluscum-like papules as a presentation of early papulonecrotic tuberculid in association with nodular tuberculid in a male with asymptomatic active pulmonary tuberculosis. J Cutan Med Surg. 2015; 19:159–162.

5. Schneider JW, Jordaan HF, Geiger DH, Victor T, Van Helden PD, Rossouw DJ. Erythema induratum of Bazin. A clinicopathological study of 20 cases and detection of Mycobacterium tuberculosis DNA in skin lesions by polymerase chain reaction. Am J Dermatopathol. 1995; 17:350–356.

6. Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw-Hill;2012. p. 2225–2240.
7. Friedman PC, Husain S, Grossman ME. Nodular tuberculid in a patient with HIV. J Am Acad Dermatol. 2005; 53:2 Suppl 1. S154–S156.

8. Kumar B, Parsad D. Is ‘nodular tuberculid’ a distinct entity. Pediatr Dermatol. 2001; 18:164–167.

9. Lee JY, Shin SJ, Yoo CS, Kim CW, Kim SS. A case of atypical cutaneous tuberculid in an immunocompromised patient. Korean J Dermatol. 2013; 51:705–708.
10. Lee JI, Park HJ, Lee JY, Cho BK. A case of lichen scrofulosorum developing after BCG vaccination. Korean J Dermatol. 2009; 47:309–312.
11. Choi SJ, Won CH, Chang S, Lee MW, Choi JH, Moon KC. Lichen scrofulosorum occurring in association with tuberculous salpingitis. Korean J Dermatol. 2012; 50:358–361.
12. Oh ST, Lee HJ, Youn DH, Kim JW. A case of papulonecrotic tuberculid combined with erythema induratum. Korean J Dermatol. 1999; 37:1703–1705.
13. Yim JH, Koh BK, Kim JW. A case of papular tuberculid and BCGitis after BCG vaccination. Korean J Dermatol. 2005; 43:830–833.
14. Han TY, Kim JY, Kwak HW, Choi JC, Shin JW, Kim JY, et al. A case of tuberculous lymphadenitis accompanying papulonecrotic tuberculid. Tuberc Respir Dis. 2007; 62:536–539.

15. Lee HJ, Park CJ, Yi JY, Kim TY, Kim CW. A case of papulonecrotic tuberculid combined with erythema nodosum. Ann Dermatol. 1995; 7:278–281.

16. Kim G, Jeong YI, Huh JW, Kim EJ, Joh OJ. Interferon-gamma release assay in a patient with tuberculosis verrucosa cutis. Ann Dermatol. 2015; 27:109–110.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download