Abstract
Background
It has been suggested digital mucous cysts (DMCs) are associated with osteoarthritis and osteophytes in the elderly, and usually have a communicating pedicle with the joint. Surgical excision is a standard therapy with a high cure rate.
Objective
The purpose of this prospective study is to evaluate the features of DMCs via clinical, radiological and pathological examination and the efficacy of surgical excision of DMCs.
Methods
Between 2010 and 2014, 24 Korean patients were treated with the resection of the cyst and the pedicle. Preoperative X-ray and ultrasonography were performed to detect the presence of the osteophyte and the connection to the joint space. Postoperative patients' satisfaction score was assessed by the visual analogue scale (0~10).
Digital mucous cyst (DMC) was titled “synovial lesion of the skin” by Hyde in 1883, and has other names such as synovial cyst, periungual ganglia, mucinous pseudocyst, and myxoid cyst1.
The etiology and pathogenesis of DMCs are unclear. However, two possible types of DMCs have been suggested. One is caused by the herniation of tendon sheaths or synovial linings and is associated with degenerative joint diseases and osteophytes in the elderly23. The other type is caused by overproduction of mucin by fibroblasts4. The connections between the cysts and the joints were controversial1, but were investigated by means of dye injections into the joint and the definite communication has been identified in the surgical fields45.
Several therapies have been performed. They include aspiration of cystic contents6, cryosurgery7, CO2 laser therapy89, and surgical excision34. Excision is considered as a standard therapy of DMCs because of its high cure rate.
Until now, there have been only few reports about DMCs in the dermatological literatures. Most were investigated by orthopedic surgeons. So we began to study the features of DMCs including osteophytes and leakage from joint via clinical, radiological and pathological examination, and the efficacy of surgical excision in the dermatological fields.
Between 2010 and 2014, 24 Korean patients with DMCs were included in our study. The diagnosis of DMCs was based on the clinical assessment and histopathological results.
The clinical features of DMCs were evaluated by our protocol. Patients' age, duration, location, size of cysts, symptoms, associated nail findings and previous treatments were investigated. Preoperative X-ray and ultrasonography were performed to detect the presence of the osteophyte and the connection to the joint space. Histologic types of DMCs were classified into the myxomatous type, which was a subepidermal cystic space and the ganglion type, which was a cyst deeply seated, surrounded by a fibrous stroma with a pedicle in most instances.
The surgical treatments of DMCs were performed via “H” or “U” shaped incision over the distal interphalangeal (DIP) joint (Fig. 1). The cystic lesion was identified and a meticulous dissected along with the compressed stroma and a pedicle. After ligating the pedicle with 6-0 Vicryl (Ethicon, Sommerville, NJ, USA), the dissected portion was excised and lightly electrocoagulated. Osteophytes, if existed, were removed if existed with a rongeur after the extensor tendon was carefully raised. If the cyst had ruptured previously or the pedicle was not identified, the site was curetted with light electrocoagulation and allowed to heal by secondary intention. The skin incision was closed with 5-0 nylon and the wound was dressed with antimicrobial ointment under a firm bandage. The sutures were removed in 10 to 14 days.
The characteristics of 24 patients, 21 men and 3 women, are summarized in Table 1. The age of the patients ranged from 53 to 82 years (mean: 66.8 years) and the duration of DMCs was between 2 months and 10 years (mean: 20.7 months). The DMCs involved fingers or thumbs in 19 patients and toes in 5. While 5 DMCs occurred near the nail fold, 19 DMCs were near the joint. Seven patients presented with nail deformities such as longitudinal groove or umbilication. Of 24 patients, 10 had multiple aspirations, 2 had undergone previous cryosurgery and 1 had been treated with sclerotic agent.
Preoperative X-ray was checked in 19 patients. Of these, osteophytes were found in 3 cases (15.8%; Fig. 2). In ultrasonographic findings of 22 patients, there were prominent flow signals between the cyst and the joint space in 3 cases (13.6%; Fig. 3). Histopathologic examination revealed 11cases of myxomatous type and 13 cases of ganglion type.
During surgery, pedicles were ligated in most patients except for those with DMCs near the nail fold (Case no. 1, 2, 8, 14, 24) and on the small joint of toe (Case no. 11, 12, 19).
Recurrences were observed in 4 cases during at least 1 year follow-up period, and recurrence rate was 16.7%. Of 4 cases, 2 were fingers (2/19, 10.5%) and 2 were toes (2/5, 40.0%). And 1 case was located near the nail fold and 3 were near the joint (Table 2).
Postoperative complications were few. Mild pain, transient joint stiffness and swelling were observed.
Mean score of patients' satisfaction for surgery by means of VAS was 8.3 in 20 patients who gave answers.
DMCs, the most common soft tissue tumor in the hand, occurs between second to fourth decades and affects women more than men. Patients often complain of annoying mass that with gelatinous discharge upon squeezing or minor trauma. DMCs occurs as solitary, round to oval, skin colored cystic nodular lesion on the digits of the hand12310.
DMCs are commonly associated with degenerative changes of DIP joints including osteoarthritis. It has been pointed out that DMCs originate from the area of the arthritic spurs and almost all of the patients had evidence of osteophytes noted on X-ray311, and removing the spurs may improve treatment outcome1213. However, in our study, osteophytes were found in only 3 patients (15.8%) despite the fact that all of our patients were over 50 years of age. In addition, Lawrence14 reported that osteophyte removal is not essential for treatment success as opposed to the statement made by Brown et al.15 Thus, the relationship between DMCs and osteophytes needs further evaluations.
It has been suggested that there are two histologic types in DMCs, the myxomatous type and the ganglion type. The former is located near the nail fold and the latter is located near the joint101116. The current study shows that the location of DMCs and the histologic types did not always match. Whereas 11 out of 13 cases of the ganglion type were located near the joint, only 2 out of 11 cases of the myxomatous type were located near the nail fold. Therefore, differentiating the two histologic types by clinical location only was difficult, and may not be essential because the surgical technique and postoperative recurrence rate of the two types were not significantly different in our series.
De Berker and Lawrence45 reported that there is a connection between DMCs and the joint and demonstrated this connection in more than 80% of the patients by injecting the methylene blue into joint during surgery. Because, this methylene blue-guided surgery is difficult and time-consuming, we planned preoperative ultrasonographic examination to evaluate the communication. The communication between DMCs and the joint was found in 3 cases (13.8%), which led to the conclusion that preoperative ultrasonographic examination was not helpful in detecting the leakage site. Lawrence14 had adopted a flap technique where precise leak point identification is not required, thus reducing the potential postoperative morbidity and operation time. Eke et al.17 suggested proximal nail fold flap dissection for DMCs from a 7-year experience and hypothesized that the flap initiates dermal scarring which is thought to interrupt any connections between the joint and the cyst. According to Zook3, there is no reason to remove the cyst, as it is a compressive-type lining and obliterates when decompressed. Regardless of connection, a meticulous dissection along with excision and pedicle ligation was enough for therapeutic success in our experience. In addition, we used electrocoagulation on the stump of pedicle and surrounding stromal tissue after cyst removal, which may promote fibrosis, resulting in closure of the leak.
Recurrence occurred in 4 cases (16.7%), 2 on the fingers and 2 on the toes, and recurrence rate was higher on the toes (40.0%) than on the fingers (10.5%), which was similar to the results of previous studies514. In one recurred case, where communication was observed in ultrasonographic examination, reoperation was done after 6 months but failed again. The reason for this is not clear, but may be due to differences in joint fluid pressure in the toe depending on position14.
There were no long-term, serious complications such as infection, joint limitation, and nail dystrophy in our study. Mild pain, transient joint stiffness or swelling were observed, but disappeared gradually without treatment.
The limitation of our study comes from the relatively small number of DMC patients in the dermatologic fields.
In conclusion, the pathogenic relationship between DMCs and osteophytes needs to be further clarified, since the incidence of osteophytes noted on X-ray was much lower than the previous reports in our study. Preoperative ultrasonographic examination is not useful in detecting the communication between DMCs and the joint. A meticulous surgical technique including a pedicle ligation and electrocoagulation rather than identification of leakage site seems to be more important for DMC treatment.
Figures and Tables
Fig. 1
The surgical treatments of digital mucous cysts. (A) Before surgery, (B) dissected cyst, (C) pedicle (arrow), (D) after surgery.

Fig. 3
On the ultrasonographic finding, there was a prominent flow signal between the cyst and the joint space (Case no. 4).
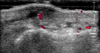
Table 1
Characteristics of patients

Table 2
Summary of the results

References
1. Miller PK, Roenigk RK, Amadio PC. Focal mucinosis (myxoid cyst). Surgical therapy. J Dermatol Surg Oncol. 1992; 18:716–719.

2. Salasche SJ. Myxoid cysts of the proximal nail fold: a surgical approach. J Dermatol Surg Oncol. 1984; 10:35–39.

3. Zook EG. Ganglions of the distal interphalangeal joint. In : Krull EA, Zook EG, Baran R, Haneke E, editors. Nail surgery: a text and atlas. New York: Lippincott Williams & Wilkins;2001. p. 209–212.
5. De Berker D, Lawrence C. Ganglion of the distal interphalangeal joint (myxoid cyst): therapy by identification and repair of the leak of joint fluid. Arch Dermatol. 2001; 137:607–610.
6. Epstein E. A simple technique for managing digital mucous cysts. Arch Dermatol. 1979; 115:1315–1316.

7. Minami S, Nakagawa N, Ito T, Sadanobu N, Lin Y, Natsuaki M, et al. A simple and effective technique for the cryotherapy of digital mucous cysts. Dermatol Surg. 2007; 33:1280–1282.

8. Huerter CJ, Wheeland RG, Bailin PL, Ratz JL. Treatment of digital myxoid cysts with carbon dioxide laser vaporization. J Dermatol Surg Oncol. 1987; 13:723–727.

9. Kim JH, Park JH, Jee H, Oh SH. Successful treatment of recurrent digital mucoid cysts using a 1,444-nm neodymium-doped yttrium aluminum garnet laser. Dermatol Surg. 2011; 37:1528–1530.

10. Hur J, Kim YS, Yeo KY, Kim JS, Yu HJ. A case of herpetiform appearance of digital mucous cysts. Ann Dermatol. 2010; 22:194–195.

11. Lin YC, Wu YH, Scher RK. Nail changes and association of osteoarthritis in digital myxoid cyst. Dermatol Surg. 2008; 34:364–369.

12. Mani-Sundaram D. Surgical correction of mucous cysts of the nail unit. Dermatol Surg. 2001; 27:267–268.

13. Lee HJ, Kim PT, Jeon IH, Kyung HS, Ra IH, Kim TK. Osteophyte excision without cyst excision for a mucous cyst of the finger. J Hand Surg Eur Vol. 2014; 39:258–261.

14. Lawrence C. Skin excision and osteophyte removal is not required in the surgical treatment of digital myxoid cysts. Arch Dermatol. 2005; 141:1560–1564.

15. Brown RE, Zook EG, Russell RC, Kucan JO, Smoot EC. Fingernail deformities secondary to ganglions of the distal interphalangeal joint (mucous cysts). Plast Reconstr Surg. 1991; 87:718–725.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download