Abstract
Background
An epidermal cyst is a common keratin-filled epithelial-lined cyst. The treatment of choice for epidermal cysts is surgical excision. If the cyst becomes ruptured, incision and drainage with oral antibiotic therapy or intralesional steroid injection are required.
Objective
To analyze the dermoscopic features that can differentiate between ruptured and unruptured epidermal cysts.
Methods
The clinical and dermoscopic features of the pathologically confirmed epidermal cysts of two subgroups of 38 patients, 20 with unruptured cysts and 18 with ruptured cysts, were reviewed.
Results
With regard to the dermoscopic features, an ivory- white background color and punctum were commonly found in both groups (p>0.05). The unruptured-cyst group showed higher frequencies of pore sign (p<0.05), blue-white veil (p>0.05), no vascular structure, and arborizing telangiectasia (p<0.05), but the ruptured-cyst group usually had red lacunae (p>0.05) and peripheral linear branched vessels (with an erythematous rim) (p<0.05).
An epidermal cyst can generally be diagnosed based on clinical and physical findings, but a biopsy is required for differential diagnosis with other subcutaneous nodules, and for determining the best treatment modality12. The typical treatment is to remove the cyst after incision, but if the cyst is ruptured and inflamed, or if secondary infection exists, intralesional steroid injection or antibiotic therapy after incision and drainage is required. Choosing a treatment is not easy in some cases; however, because it is difficult to determine if the epidermal cyst is ruptured with the naked eye1. As Asians has darker skin phototypes, it can be more difficult to detect inflammation with the naked eye in Asians than whites. Further, as biopsy takes time and is invasive, a simple, quick, and non-invasive diagnosis method that would be helpful for the differential diagnosis of subcutaneous nodules and for the differentiation of ruptured from unruptured epidermal cysts is required. Dermoscopy is useful for observing a punctum characteristically appearing in an epidermal cyst, and can increase the accuracy of diagnosis of epidermal cysts. No study has been done; however, with regard to the difference in the dermoscopic findings between ruptured and unruptured epidermal cysts. As such, this study was conducted to evaluate the usefulness of dermoscopy in differentiating ruptured from unruptured epidermal cysts in patients with epidermal cysts confirmed via biopsy.
This study was conducted targeting the 38 patients who visited the Department of Dermatology of Kosin University Gospel Hospital due to subcutaneous nodules within the period from September 2011 to June 2013, and who were diagnosed to have epidermal cysts based on the results of the biopsy that was performed after an ultrasound scan.
The total of 38 patients was divided into a group of 20 patients with unruptured epidermal cysts and 18 patients with ruptured epidermal cysts according to histologic findings. Ruptured epidermal cyst is defined as which shows partial or total loss of epithelial wall, exposure of keratinous material to surrounding tissue, or granulomatous inflammation on histologic findings. To compare the two groups, the patients' clinical features were obtained from their medical records and clinical images, and their dermoscopic findings were reviewed.
Based on the patients' medical records and clinical images, ages, genders, duration, location, diameter, redness, symptoms (pain, tenderness, and local heat) were searched and reviewed for comparison.
After lesions were observed via polarized dermoscopy (DermLite DL3, 10× magnification; 3Gen, LLC, Dana Point, CA, USA), the images of the lesions were taken with a digital camera (Sony Cybershot DSC-W290, 3 optical zoom; Sony Corporation, Tokyo, Japan) connectable to dermoscopy. The ivory-white background color, punctum, pore sign, red lacunae, blue-white veil, and vascular pattern of the cysts were observed via dermoscopy.
For the statistical analysis, SPSS Statistics ver. 17.0 for Windows (SPSS Inc., Chicago, IL, USA) was used, and to compare the differences in the dermoscopic findings between the unruptured- and ruptured-cyst groups, chi-square test and Fisher's exact test were performed. All statistically processed results were determined to be significant at p<0.05.
The mean age was 45 years (18~75 years) in the unruptured-cyst group and 43.1 years (19~71 years) in the ruptured-cyst group. The mean age of all the patients was 44.1 years. The male-to-female ratio was 10:10 cases (1:1) in the unruptured cyst group and 7:11 cases (about 1:1.6) in the ruptured-cyst group. For all the patients, the male-to-female ratio was 1:1.2.
The mean duration of the disease was 20.9 months in the unruptured-cyst group and 17.7 months in the ruptured-cyst group. For all the patients, it was 19.4 months. Lesions most commonly developed on the face (25.0%), trunk (30.0%), and neck (20.0%) in the unruptured-cyst group. Similarly, in the ruptured-cyst group, the face, trunk, and neck were the sites where lesions most commonly developed. The mean long diameters of the epidermal cysts were 10.95 mm in unruptured-cyst group and 12 mm in ruptured-cyst group. And redness was observed in 20.0% of unruptured-cyst group and 61.1% of ruptured-cyst group. With regard to redness, the difference between the two groups was significant (p<0.05).
With regard to the symptoms, in the unruptured-cyst group, asymptomatic cases were the most common (80.0%), and a few cases were accompanied by tenderness (10.0%) or pain (10.0%). As for the ruptured-cyst group, pain was the most common symptom (66.7%), and a few cases were asymptomatic (22.2%) or were accompanied by local heat (22.2%) or tenderness (11.1%). With regard to pain and local heat, the difference between the two groups was significant (p<0.05).
The ivory-white background color commonly appeared in 83.3% and 70% of the patients in the unruptured- and ruptured-cyst groups, respectively. Punctum was found in 45.0% and 38.9% of the patients in the unruptured- and ruptured-cyst groups, respectively, showing similar frequencies. The pore sign was observed in 45.0% and 11.1% of the patients in the unruptured- and ruptured-cyst groups, respectively. Red lacunae were observed more commonly in the ruptured-cyst group (55.6%) than in the unruptured-cyst group (15.0%). The blue-white veil was observed in 20.0% of the patients in the unruptured-cyst group and was not observed in any of the patients in the ruptured-cyst group. For the vascular pattern, in the unruptured-cyst group, arborizing telangiectasia (Fig. 2B) was observed in 20.0% of the patients, peripheral linear branched vessels (with an erythematousrim) (Fig. 1B) were found in 10.0% of the patients, and no vascular structure was found in the rest of the patients (70.0%). As for the ruptured-cyst group, peripheral linear branched vessels (with an erythematous rim) were found in 77.8% of the patients, and no vascular structure was found in the rest of the patients (22.2%). With regard to peripheral linear branched vessels (with an erythematous rim), the difference between the two groups was significant (p<0.001).
An epidermal cyst is a common keratin-filled epithelial-lined cyst3. The duration of the disease varied from 28.8 to 48.9 months in the previous studies published in Korea45. It has been known that the longer the duration of disease is, the higher the likelihood of damage in the cystic wall, which results in further destruction6. In the Korean literature, however, the duration of the disease was even shorter in the group with a destroyed cystic wall57. It is believed that this was because the patients visited the hospital earlier due to the inflammatory response that occurred after the destruction of the cystic wall57. In this study, the mean duration of the disease was 19.4 months, which was slightly shorter than that in the other studies that had been published in Korea. The result that the mean duration of the disease was shorter in the ruptured-cyst group than in the unruptured-cyst group, however, coincided with the results of the previous studies in the country.
Epidermal cysts not accompanied by inflammation are mostly asymptomatic, but if inflammation is present or if the cysts are too large and are pressing the surrounding tissues, or if they are ruptured and extend to the surrounding soft tissues, an inflammation response may occur, accompanied by redness, severe pain, and local heat. Due to repeated trauma or expansion of the cysts, rupture is promoted, and the destruction of the cystic wall occurs at the part with the weakest resistance. Therefore, the site and size of cysts are known to determine whether or not the cystic wall would be destroyed89. In this study, cysts most frequently occurred on the face, trunk, and neck in both groups. The mean size of the cysts was larger in the ruptured-cyst group than in the unruptured-cyst group, showing that the size of the cyst determines whether or not the cystic wall would be destroyed. And cutaneous manifestations such as redness, pain, and local heat were observed in higher rate in ruptured-cyst group than in unruptured-cyst group.
Dermoscopy is a non-invasive test without time and spatial limitations, and since recently, polarized dermoscopy has also been used with a cross-polarized lens, which, compared to the conventional non-polarized dermoscopy, allows deeper structures such as blood vessels and collagen to be seen. Thus, its importance is more emphasized, especially in screening tests of malignant tumors, including melanoma or basal cell carcinoma, for which the diagnoses of the type of vascular structures and the relevant colors are particularly important1011. This study was carried out from the same point of view, and by observing all the lesions using polarized dermoscopy, the vascular structure of the lesions and the relevant colors were effectively observed.
In this study, the ivory-white background color and punctum appeared as common dermoscopic findings in both the unruptured- and ruptured-cyst groups. The white structure is known to be a dermoscopic clue implying a tumor originating from the hair follicle, and is thought to be a finding histologically appearing corresponding to the keratin mass12. Punctum is a plugged pilosebaceous unit and is a characteristic finding in epidermal cysts. Regarding the prevalence of punctum, in the study conducted by Chandrasekaran et al.13, it was found in 15 of the 34 patients with an epidermal cyst (42.1%) with the naked eye. Through dermoscopy, deeper structures such as blood vessels and collagen of the skin can be observed on an enlarged scale, which is helpful for identifying small punctum, which cannot be recognized with the naked eye. Therefore, when dermoscopy is used, punctum was thought to be observed at a higher rate. In this study, however, through dermoscopy, it was observed in 16 of the 38 patients with an unruptured or a ruptured cyst, or in 42.1% of the patients, which exactly coincides with the previous study's result. This result might be associated with the small sample size in both studies, and further studies targeting a larger number of patients would be required in the future.
The pore sign is known to be a dermoscopic finding that is useful in diagnosing epidermal cysts. The area where the pore sign appears is filled with keratin and has a white, yellow, brown, black, or other color. Also, this area appears in the form of a roughly circular orifice. When the cyst is small or not mature enough, it is difficult to find14. In this study, the pore sign was more commonly observed in the unruptured-cyst group (45.0%) than in the ruptured-cyst group (11.1%). It can be assumed that it was not easy to recognize the pore sign in the ruptured-cyst group because the keratin was discharged to the outside of the cystic wall after the rupture of the cyst. In addition, the pore could not maintain a complete form, unlike in the unruptured cyst, and a vascular structure developed.
Ruptured epidermal cysts may contain red blood cell components due to bleeding, which may appear as red lacunae in dermoscopy. In this study, it was observed in 15.0% of the patients in the unruptured-cyst group and in 55.6% of the patients in the ruptured-cyst group. Park and Ko15 reported that a histological finding of hypergranulosis was observed in about 17% of epidermal cysts, and more common in unruptured epidermal cysts. The dermoscopic finding of a blue-white veil is known to reflect the histological finding of hypergranulosis1617. In this study, a blue-white veil was found in 20.0% of the patients in the unruptured-cyst group and was not found in any of the patients in the ruptured-cyst group.
In the vascular pattern observed via dermoscopy, the vascular structure was not observed in most of the patients in the unruptured-cyst group, and a vascular structure of the peripheral linear branched vessels (with an erythematous rim) was found in 77.8% of the patients in the ruptured-cyst group. This is thought to have been caused by the proliferation of the vessels after the rupture of the cyst. In 20.0% of the patients in the unruptured-cyst group, arborizing telangiectasia was found in the central or peripheral portion, while in the ruptured-cyst group, it was not observed. This finding is thought to be a result of the congestion of the blood flow by pressing the surrounding tissues due to the mass effect caused by the increase in the size of the epidermal cyst. In the ruptured epidermal cysts, blood congestion occurs relatively less frequently because the mass effect shown in the unruptured epidermal cysts is reduced after the rupture, which might be the reason that arborizing telangiectasia does not appear.
In this study, the usefulness of dermoscopy in determining if the cyst in a patient clinically suspected of having an epidermal cyst is ruptured was confirmed. In particular, considering the inflammatory response and the proliferation of microvessels following the rupture of the cyst, dermoscopy can be helpful in determining if the epidermal cyst is ruptured because the vascular pattern can be observed via dermoscopy. In this study targeting patients with a histologically confirmed unruptured or ruptured epidermal cyst, dermoscopy was performed and findings were obtained from each group. By statistical analysis, the significance of the difference in dermoscopic findings such as vascular patterns between the two groups was confirmed. Based on the results of this study, it is believed that dermoscopy would be helpful in identifying the best treatment method to be employed by determining if epidermal cysts are ruptured.
Figures and Tables
Fig. 1
Ruptured epidermal cyst. (A) Erythematous 2×2 cm subcutaneous nodule. (B) Dermoscopic view showing peripheral linear branched vessels with an erythematous rim (arrowheads) against an ivory-white background. (C) Microscopic view showing a cystic lesion with dense inflammation surrounding the ruptured cyst (patient 5 in the ruptured-cyst group).
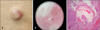
Fig. 2
Unruptured epidermal cyst. (A) Well-demarcated bluish 2×2 cm subcutaneous nodule. (B) Dermoscopic view showing a arborizing telangiectasia consisting of vessels with different diameter and several branches. (C) Microscopic view showing prominent dilated vessels with congestion of blood flow between the epidermis and cystic wall (patient 9 in the unruptured-cyst group).

Fig. 3
Schematic representation of dermoscopic pattern in patient with unruptured cyst and ruptured cyst.

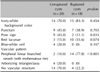
Table 1
Clinical features of the unruptured and ruptured epidermal cysts

Table 2
Dermoscopic features of the unruptured and ruptured epidermal cysts
References
1. Thomas VD, Snavely NR, Lee KK, Swanson NA. Benign epithelial tumors, hamartomas, and hyperplasias. Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw Hill;2012. p. 1332–1334.
2. Kirkham N. Tumors and cysts of the epidermis. Elder DE, Elenitsas R, Johnson BL, Murphy GF, Xu X. Lever's histopathology of the skin. 10th ed. Philadelphia: Lippincott Williams & Wilkins;2009. p. 800–802.
3. Lee SY, Moon KC. A clinical and histopathologic study of epidermal cysts. Ann Dermatol. 1994; 6:157–161.

4. Chung J, Lee BJ, Ahn SK, Song DH, Lee WS, Kim SC. A clinical and histopathologic study of epidermal cysts. Korean J Dermatol. 1993; 31:517–522.
5. Kim SK, Kwon H, Lee SY, Lee JS, Whang KU, Park YL, et al. A clinical and histopathological study of epidermal cysts in the province of Chungcheongnam-do. Korean J Dermatol. 2009; 47:516–523.
6. McGavran MH, Binnington B. Keratinous cysts of the skin. Identification and differentiation of pilar cysts from epidermal cysts. Arch Dermatol. 1966; 94:499–508.

7. Cho HM, Kim SN. A clinical and histopathological study of 324 cases of epidermal cyst. Korean J Dermatol. 2007; 45:242–248.
8. Lee HS, Joo KB, Song HT, Kim YS, Park DW, Park CK, et al. Relationship between sonographic and pathologic findings in epidermal inclusion cysts. J Clin Ultrasound. 2001; 29:374–383.

9. Jin W, Ryu KN, Kim GY, Kim HC, Lee JH, Park JS. Sonographic findings of ruptured epidermal inclusion cysts in superficial soft tissue: emphasis on shapes, pericystic changes, and pericystic vascularity. J Ultrasound Med. 2008; 27:171–176. quiz 177-178.

10. Benvenuto-Andrade C, Dusza SW, Agero AL, Scope A, Rajadhyaksha M, Halpern AC, et al. Differences between polarized light dermoscopy and immersion contact dermoscopy for the evaluation of skin lesions. Arch Dermatol. 2007; 143:329–338.

11. Pan Y, Gareau DS, Scope A, Rajadhyaksha M, Mullani NA, Marghoob AA. Polarized and nonpolarized dermoscopy: the explanation for the observed differences. Arch Dermatol. 2008; 144:828–829.
12. Lallas A, Moscarella E, Argenziano G, Longo C, Apalla Z, Ferrara G, et al. Dermoscopy of uncommon skin tumours. Australas J Dermatol. 2014; 55:53–62.

13. Chandrasekaran V, Parkash S, Raghuveer CV. Epidermal cysts-a clinicopathological and biochemical study. Postgrad Med J. 1980; 56:823–827.
14. Ghigliotti G, Cinotti E, Parodi A. Usefulness of dermoscopy for the diagnosis of epidermal cyst: the ‘pore’ sign. Clin Exp Dermatol. 2014; 39:649–650.

15. Park JS, Ko DK. A histopathologic study of epidermoid cysts in Korea: comparison between ruptured and unruptured epidermal cyst. Int J Clin Exp Pathol. 2013; 6:242–248.
16. Pizzichetta MA, Canzonieri V, Soyer PH, Rubegni P, Talamini R, Massone C. Negative pigment network and shiny white streaks: a dermoscopic-pathological correlation study. Am J Dermatopathol. 2014; 36:433–438.
17. Soyer HP, Argenziano G, Chimenti S, Ruocco V. Dermoscopy of pigmented skin lesions (Part XMLLink_XYZ). Eur J Dermatol. 2001; 11:483–498.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download