Abstract
Objective
To estimate the prevalence of tinea capitis among primary school students, in Fayoum, Egypt with identification of etiological agents in both public and private primary schools.
Methods
A cross-sectional study was conducted in twelve primary schools. The students were selected from different grades with a total number of 12,128 students. Hair and scalp were clinically examined for any lesions that may suspect tinea capitis and mycological samples were collected for direct microscopy and culture.
Results
The prevalence of tinea capitis in the study group was 0.4% and higher in public than private schools (73.5% versus 26.5% respectively). Boys were more affected than girls with boy to girls' ratio 5:1. Intrafamily history of infection was present in 40.8% of tested group while 51% showed low social standard profile. Mycological culture revealed that Microsporum canis was the predominant isolated organism followed by M. audouinii (52% and 36% respectively).
Tinea capitis is a mycosis caused by dermatophytes that invade the keratinized tissues, including the corneous layer of the skin, nails, and hair1. Tinea capitis in particular remains a prevalent health problem among school-aged children under tropical conditions2. School environment usually makes children more vulnerable to cross-transmission of communicable skin diseases3.
The prevalence of tinea capitis and the predominance of its etiological agents differ according to the geographical distribution4. It has decreased in developed countries, while a high prevalence in developing countries was reported1. In some urban areas in North America, Central and South America, tinea capitis is widespread and it is still very common in parts of Africa and India. Degreef5 sought that the frequency is increasing again in the last decade, probably due to emigration, immigration, and the ease of international travelling. Its prevalence is closely related to socioeconomic status, life style, living conditions, large family size, poor hygienic conditions and close contact. It is generally spread through direct transmission via contact with an infected person or indirect transmission by sharing facilities, including contaminated hair-brushes, combs, towels or other personal items and backs of seats which is common between family members in low socio-economic areas or by direct physical contact with an infected person. The spores are long lived and can infect another individual months later6.
Although hair and scalp disorders generally are not associated with significant physical morbidity, the psychological impact of visible scalp problems may be very high, and changes in the appearance of skin and hair affect self-esteem and confidence in social settings7.
This study aimed to estimate the prevalence of tinea capitis among primary school students, in Fayoum city, Egypt and explore the predisposing factors with identification of etiological agents in both public and private primary schools.
The study was a cross-sectional descriptive study, conducted in twelve primary schools at Fayoum city which represents Upper Egypt during the academic year of 2013~2014.
The sample was purposive sampling. Fayoum was chosen because it has an urban and rural community with variable socioeconomic status. The schools were selected according to their geographical distribution to cover the whole district and from public and private schools with different socioeconomic levels (12 primary schools in Fayoum district 6 public and 6 private schools). All the students in the selected schools were enrolled in the study from different grades with a total of 12,128 students. A structured questionnaire was formed including socioeconomic data as age, sex, number of family members, the level of education and occupation of the parents, to determine the social standard of a family. A score system was used as described previously8 and according to the sum of the parents' score values, the social standard can be classified into three levels: low level, if the sum is <8, intermediate level if the sum ranged between 8~18, and high level if the sum ranged between 19~28. The students were asked about the level of living conditions, bed, towel and comb sharing, similar family affection, presence of pets in home, history of the lesion and treatment taken. Information about the disease and instruction about the simplest ways to guard against this infection was given to the students.
A suitable place with good illumination was prepared in each school with the cooperation of the schools' principals to conduct the clinical examination. Hair and scalp were clinically examined with the help of Wood's light for any lesions that may be suspect to be affected with tinea capitis. Dermoscope was used for detection of variable clinical features of the disease (comma shaped, corkscrew and broken hair). All the school classes from the 1st to the 6th grade were examined with the help of a school nurse for reassurance of the students.
Sample collection: Affected areas were scraped with a blunt scalpel and affected broken hair was plucked and sufficient amount of samples were transported in a folded square of paper to laboratory at Department of Medical Microbiology and Immunology, Faculty of Medicine, Fayoum University.
Scalp scales and broken off hair stumps containing the root section are mounted in a 10%~20% potassium hydroxide gently heated and viewed under the light microscope. Positive microscopy (endothrix or ectothrix) was reported. Culture was performed for all samples irrespective to the results of microscopic examination. Samples were cultured in Screw capped bottles containing Sabouraud dextrose agar with chloramphenicol and cycloheximide (Oxoid, Ltd.) to suppresses the growth of bacteria and environmental contaminant fungi, incubated at 28℃ for 2~6 weeks, examined periodically for evidences of growth of dermatophytes. Identification was carried out using conventional methods; cultures were examined for morphology, texture and color of growth from top and reverse sides and microscopic examination of stained Lactophenol cotton blue film were performed for identification of macroconidia, microconidia, pectinate bodies and other structures needed for identification of different species9.
Data were collected, coded and analyzed using SPSS software ver. 18.0 under Windows 7 (IBM Co., Armonk, NY, USA), and a simple descriptive analysis in the form of percentage distribution, means were done.
This study was reviewed and approved by the Faculty of Medicine, Fayoum University, Research Ethical Committee with protocol approval number (9/2013). The official approval was obtained from the Directorate of Health and Education, Directors of the schools and students' parents. The study was conducted after explaining the aim of the study and confidentiality was expressed to the students. Verbal consents were taken from class teacher and students before examination. All students had the right not to participate in the study. The method of examination was explained to students and school nurse. Treatment was prescribed when indicated and method of use was explained.
The total number of study group screened for tinea capitis was 12,128 students; 49.8% in public schools (n=6,037) and 50.2% in private schools (n=6,091) were enrolled in the study. Among them 65.6% (n=7,960) were boys and 34.4% (n=4,168) were girls. The age of the students ranged from 5.5 years old to 12 years old with the mean age was 8.4±1.8 years.
Based on clinical examination, 49 students (0.4%) were suspected to have tinea capitis with no significant difference between public and private schools (Table 1). A total boy to girls' ratio was 5:1.
As regarded the education of parents, a high significant correlation was detected between illiteracy and tinea capitis (p=0.000); nearly half of students affected with tinea capitis had illiterate parents or received only primary education (n=23, 46.9%) versus 17.3% for non-affected children (n=2,059), while 20.4% (n=10) and 32.6% (n=16) was secondary or higher education respectively versus 42.5% (n=5,129) and 40.2% (n=4,855) respectively for non-affected children. Most predisposing factors that facilitate infection as living in a crowded environment, sharing of bed, towels, comb, intrafamily history of tinea capitis and low social standard were significantly higher in all affected children than others (p<0.05). But when comparing affected children with non-affected others in public schools we found that the only significance detected was with intrafamily history while those of private schools showed more significance regarding predisposing factors as summarized in Table 2.
As regarded the number of the lesion, 53.1% (n=26) of the lesions were single lesion; 42.9% (n=21) were multiple lesions and 4.1% had two lesions (n=2). The type of the lesions was mainly scaly 81.6% (n=40), scaly and black dot in 16.3% (n=8) and black dot in 2% (n=1). The shape of the lesion appeared to be rounded in 57.1% (n=28), oval in 28.6% (n=14), rounded and oval in 10.2% (n=5), and irregular in 4.1% (n=2) (Fig. 1).
Twenty-nine dermatophyte isolates were recovered by mycological cultures from 25 samples (51.0%) and the remaining 24 samples (49.0%) gave negative results. Microsporum canis was the predominant isolate followed by M. audouinii; M. canis was recovered as a single isolate from 10 samples (40.0%) and in association with Trichophyton violaceum in 3 samples (12.0%) (total, 52.0%) (Fig. 2). The relation of isolated organisms and clinical types is illustrated in Table 3. Ectothrix was detected in 15/25 of hair samples (60.0%) while endothrix was detected in 2/25 of samples (8.0%). The number of positive culture in public schools was 76.0% (n=19) and 24.0% in private schools (n=6). Although M. canis was the highest among the isolated dermatophytes, correlation of mycological type and animal contact was not significant (p>0.05).
Tinea capitis is a public health problem worldwide especially in developing countries10. Information about the prevalence of tinea capitis in Egypt is limited. It was reported that the high occurrence of tinea capitis is linked to children less than 10 years of age4. Our study aimed to estimate the prevalence of tinea capitis among primary students, in Fayoum city, Egypt. Fayoum was chosen because it has rural and urban areas and some of the Fayoum villages were with poor sanitary water supply making regular washing of hair difficult.
Our results revealed that the prevalence rate of tinea capitis was 0.4%. This result was nearly to that of Triviño-Duran et al.11 who examined 1,305 school children, aged 3~15 years, from 21 schools located in the inner city of Barcelona and found that the infection rate was 0.23%, distributed among the schools. Our results are much lower than that reported in older studies from Egypt; in Alexandria, the prevalence among primary school children was 7.5%12 and in Ismaelia, Azab et al.13 reported the prevalence was 92.9%. The limited number in Azab et al.'s study13 (only 56 children) may explain the wide discrepancies found.
The current study revealed insignificant difference between public and private schools as regarded incidence of tinea capitis. Boys to girls ratio was 5:1 which may be due to most of the girls' hair in this region was covered by scarfs at a young age, starting at the age of seven in some schools leading to some sort of protection against catching the infection from other infected students and girls also apply a regular vegetable oils over the scalp which reported to have antifungal properties against dermatophytes1415. This result is in agreement with previous study screened 4,601 children with an average age 10.7±0.16 years, and found that boys with tinea capitis were much higher than girls (63.7% versus 36.3% respectively)10.
As regarded the predisposing factors related to socioeconomic status; low socioeconomic profile was detected in 51% and 95.9% of them sharing bed and towels. This is in agreement with Fathi and al-Samarai16 who demonstrated that the prevalence rate of tinea capitis was higher in children with low socioeconomic profile with a male to female ratio that was 2:1.
Many reports suggested that animal contact is a strong predisposing factor for tinea capitis17. More than half (51%) of the positive cases in the current study were in contact with animals but without significant association. Much lower percentage was reported in El-Khalawany et al.'s study (17.2%)17. These results may be due to that M. canis ; the most isolated dermatophyte in this study; is mostly associated with cat and dogs contact and our study included all animals that covered M. canis-related animal. Also family history is high in patient group suggesting human to human transmission.
The type of the lesions was mainly scaly (81.6%) which is in accordance with that reported by El-Khalawany et al.17 in Egypt as scaly scalp was the most clinically presented type (37.9%).
Positive cultures were obtained only in 51% of cases which could be explained by regular application of fungistatic oils by most tested children. The results of Chapman et al.18 go hand in hand with ours; they conducted a study for 15 years and found that, from 1,220 patients suffering of signs and symptoms of tinea capitis, only 39% yield positive culture.
M. canis was responsible for most cases in this study followed by M. audouinii (52% and 36% respectively). Earlier studies in Egypt reported that T. violaceum was the most common isolated organism and in some studies was the only isolated dermatophyte causing tinea capitis (Table 4)121317192021. It seems that there is an epidemiological change regarding the etiological agent in our region. This result is confirmed by another study targeting Palestinian patients and found that M. canis is replacing T. violaceum as an etiology of tinea capitis22. Razzaq Adel et al.23 in Kuwait, found that M. canis was the predominant dermatophyte isolated in 62.5% of tinea capitis cases, followed by T. violaceum in 19.3% and T. tonsurans in 13.1%. While Abanmi et al.24 in Saudi Arabia, reported that the prevalence of tinea capitis is 22% and the principal causative agent is M. canis.
In Europe, M. canis remains the commonest agent for tinea capitis overall. The highest incidence was reported in the Mediterranean region in addition to more distant countries as Hungary, Austria, Poland and Germany25. In conclusion, there is an epidemiological change regarding the etiological agent in our region. M. canis is replacing T. violaceum as an etiology for tinea capitis in Egypt with much lower frequency than reported previously.
Figures and Tables
Fig. 1
The different types detected of the tinea capitis lesions. (A) Scaly type. (B) Black dot type. (C) Scaly & black dot type.

Fig. 2
Isolated dermatophytes. (A) Microsporum canis on Sabouraud dextrose agar (SDA). (B) M. audouinii on SDA. (C) Microscopic picture showing macroconidia of M. canis. (D) Microscopic picture showing pectinate bodies of M. audouinii.

Table 1
The incidence of tinea capitis in public and private schools

Table 2
Frequency of predisposing factors and social standards among children with and without tinea capitis in public and private schools

Table 3
Isolated dermatophytes in relation to clinical types
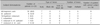
Table 4
Changes of dermatophytes species causing tinea capitis in Egypt (from 1965 to 2012)

| Year | Area | Number of patients | Isolated dermatophytes | % |
|---|---|---|---|---|
| 1965~196719 | Cairo | 250 | Trichophyton violaceum | 53.3 |
| T. schoenleini | 26.7 | |||
| Microsporum canis | 18.8 | |||
| 198321 | Rural village | 230 | T. violaceum | 100 |
| 200012 | Alexandria | 38 | T. violaceum | 100 |
| 2010~201113 | Ismailia | 52 | T. violaceum | 40.3 |
| M. canis | 30.8 | |||
| M. gypseum | 17.3 | |||
| 2002~201217 | Multicenter study: Cairo Alexandria, Tanta | 58 | T. violaceum | 56.9 |
| M. audouinii | 19.0 | |||
| M. canis | 15.5 | |||
| T. schoenleini | 8.6 |
References
1. Pérez-González M, Torres-Rodríguez JM, Martínez-Roig A, Segura S, Griera G, Triviño L, et al. Prevalence of tinea pedis, tinea unguium of toenails and tinea capitis in school children from Barcelona. Rev Iberoam Micol. 2009; 26:228–232.

2. Ghannoum M, Isham N, Hajjeh R, Cano M, Al-Hasawi F, Yearick D, et al. Tinea capitis in Cleveland: survey of elementary school students. J Am Acad Dermatol. 2003; 48:189–193.

3. Andrews MD, Burns M. Common tinea infections in children. Am Fam Physician. 2008; 77:1415–1420.
4. Sidat MM, Correia D, Buene TP. Tinea capitis among children at one suburban primary school in the city of Maputo, Mozambique. Rev Soc Bras Med Trop. 2007; 40:473–475.

5. Degreef H. Clinical forms of dermatophytosis (ringworm infection). Mycopathologia. 2008; 166:257–265.

6. Bassiri-Jahromi S, Khaksari AA. Epidemiological survey of dermatophytosis in Tehran, Iran, from 2000 to 2005. Indian J Dermatol Venereol Leprol. 2009; 75:142–147.

8. Park JE, Park K. Textbook of preventive and social medicine. 7th ed. Jabalpur: Banarsidas Bhanot;1979. p. 81.
9. Rippon JW. Dermatophytosis and dermatomycoses. Medical mycology-The pathogenic fungi and the pathogenic actinomycetes. 3rd ed. Philadelphia: WB Saunders;1988. p. 169–275.
10. Kechia FA, Kouoto EA, Nkoa T, Nweze EI, Fokoua DC, Fosso S, et al. Epidemiology of tinea capitis among school-age children in Meiganga, Cameroon. J Mycol Med. 2014; 24:129–134.

11. Triviño-Duran L, Torres-Rodriguez JM, Martinez-Roig A, Cortina C, Belver V, Perez-Gonzalez M, et al. Prevalence of tinea capitis and tinea pedis in Barcelona schoolchildren. Pediatr Infect Dis J. 2005; 24:137–141.

12. Omar AA. Ringworm of the scalp in primary-school children in Alexandria: infection and carriage. East Mediterr Health J. 2000; 6:961–967.

13. Azab MM, Mahmoud NF, Abd Allah S, Hosny AM, Shehata AS, Mohamed RW. Dermatophytes isolated from clinical samples of children suffering from tinea capitis in Ismailia, Egypt. Aust J Basic Appl Sci. 2012; 6:38–42.
14. Vijayakumar R, Muthukumar C, Kumar T, Saravanamuthu R. Characterization of Malassezia furfur and its control by using plant extracts. Indian J Dermatol. 2006; 51:145–148.

15. Geweely NSI. Antifungal activity of ozonized olive oil (Oleozone). Int J Agri Biol. 2006; 8:670–675.
16. Fathi HI, al-Samarai AG. Prevalence of tinea capitis among schoolchildren in Iraq. East Mediterr Health J. 2000; 6:128–137.

17. El-Khalawany M, Shaaban D, Hassan H, Abdalsalam F, Eassa B, Abdel Kader A, et al. A multicenter clinicomycological study evaluating the spectrum of adult tinea capitis in Egypt. Acta Dermatovenerol Alp Pannonica Adriat. 2013; 22:77–82.
18. Chapman JC, Daniel CR 3rd, Daniel JG, Daniel MP, Sullivan S, Howell D, et al. Tinea capitis caused by dermatophytes: a 15-year retrospective study from a Mississippi Dermatology Clinic. Cutis. 2011; 88:230–233.
20. Taha M, Amer M, Salem A, el Harras M. The perfect state of Trichophyton violaceum. Int J Dermatol. 1994; 33:493–495.
21. Othman T, Vacher C. Tinea of the scalp in Egypt. Bull Soc Pathol Exot Filiales. 1983; 76:126–128.
22. Ali-Shtayeh MS, Yaish S, Jamous RM, Arda H, Husein EI. Updating the epidemiology of dermatophyte infections in Palestine with special reference to concomitant dermatophytosis. J Mycol Med. 2015; 25:116–122.

23. Razzaq Adel AA, Sultan AO, Basmiah AM, Aftab A, Nabel N. Prevalence of tinea capitis in southern Kuwait. Mycoses. 2007; 50:317–320.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download