Abstract
Background
Sublingual immunotherapy (SLIT) with house dust mites (HDM) preparation has recently been proven to be beneficial for treating allergic rhinitis and asthma. However, there has been no report regarding the efficacy and safety of SLIT in Korean patients with atopic dermatitis (AD).
Methods
A total of 34 patients with AD and immunoglobulin E (IgE)-proven HDM sensitization (Class ≥3) were recruited. Eczema area and severity index (EASI) score, total serum IgE level, specific IgE assays to Dermatophagoides pteronyssinus, D. farinae, and adverse effects were recorded during follow-up. "Responder" was defined as a patient with ≥30% improvement in EASI score after SLIT.
Results
Twenty-three patients continued SLIT for 12 months or more, whereas 3 patients (8.8%) dropped out because of exacerbation of dermatitis, and 8 patients (23.5%) were lost to follow-up. The average duration of SLIT treatment was 22.4 months (range, 12~32 months). EASI scores reduced significantly after 6 months of treatment (p<0.05) compared with those at baseline. A total of 18 patients were determined to be responders to SLIT after 6 months. Total and specific IgE serum levels did not significantly reduce after SLIT. No patients experienced serious adverse events, with the exception of two patients who developed transient lip and tongue swelling.
Atopic dermatitis (AD) is a common chronic inflammatory skin disease that is triggered by specific allergens, such as house dust mites (HDM). Allergen-specific immunotherapy has recently been reported to be an effective treatment for AD12. Allergen-specific immunotherapy is classified into two treatment modalities according to the method of allergen administration: subcutaneous immunotherapy (SCIT) and sublingual immunotherapy (SLIT)3. Compared to SCIT, SLIT has not been well validated, and there are conflicting data regarding the use of SLIT for treating AD2. However, a few recent reports have shown that SLIT is a viable alternative to the classic injection route45. To date, no study has assessed the efficacy and safety of SLIT for AD patients in Korea. Therefore, we aimed to investigate the efficacy and safety of SLIT in Korean patients with AD.
This was an open-label, non-controlled, non-randomized pilot trial in Pusan National University Hospital from July 2011 to September 2014. The study was approved by the institutional review board of Pusan National University Hospital (No. E-2015039), and all the patients were given informed consent. A total of 34 patients with a diagnosis of AD (by Hanifin and Rajka criteria) who presented with positive results to the specific immunoglobulin (Ig)E testing (ImmunoCAP®; Phadia, Uppsala, Sweden) to Dermatophagoides pteronyssinus (DP) and D. farinae (DF) (Class ≥3) were included in this study. Patients were excluded for having uncontrolled or severe asthma, having significant co-morbid disease such as cardiovascular disability, and using beta-blockers. Patients with AD were classified in two groups according to the number of sensitized allergens: mono-sensitized patients (sensitized to only DP and DF) and poly-sensitized patients (simultaneously sensitized to HDM and other allergens proven by a multiple allergen simultaneous test immunoblot assay (Polycheck Allergy®; Biocheck GmbH, Münster, Germany). AD patients who presented with mild to moderate severity (eczema area and severity index [EASI] score ≤20) after cyclosporine induction therapy (3~4 mg/kg for 2~4 weeks) were included.
Patients with AD received SLIT (DP and DF mix extracts, 200 standardized treatment units/dose, SLIT one®; ALK-abello, Hørsholm, Denmark) for at least 12 months. The daily dose was a volume of 0.2 ml per single-dose container. Drops were held under the tongue for 2 minutes and were then swallowed. Patients were prohibited to drink or eat any foods for 5 minutes after swallowing the drops.
The clinical efficacy of SLIT was evaluated by changes in EASI score. Responders were defined as patients with ≥30% improvement of EASI scores after SLIT. Levels of total serum IgE and specific IgE to DP and DF were measured at baseline and after 12 months of SLIT. Clinical response and adverse effects were checked after 1, 3, 6, 9, and 12 months of treatment. Topical tacrolimus 0.1% ointment/pimecrolimus 1% cream and oral antihistamines were allowed during SLIT. Short-term therapy with oral cyclosporine (3~4 mg/kg) was permitted in the case of worsening pruritus, itching, edema, or oozing.
Only patients who received SLIT over 12 months were included in the analysis. Statistical analyses were performed using PASW Statistics ver. 18.0 (IBM Co., Armonk, NY, USA), and a p-value of <0.05 was considered to indicate statistically significant differences. The Mann-Whitney test was used to test changes in EASI scores, total IgE serum levels, and specific anti-HDM IgE serum levels.
The demographics of all patients are summarized in Table 1. Twenty-three patients continued SLIT for 12 months or more, whereas 3 patients (8.8%) dropped out because of exacerbation of dermatitis, and 8 patients (23.5%) were lost to follow-up. Thirteen of the patients were male, and 10 were female (mean age, 20.6 years). The average duration of SLIT was 22.4 months (range, 12~32 months). Compared with baseline scores, there was a significant reduction of EASI scores after 6 months (p<0.05; Fig. 1). This presented a 51.6% reduction in EASI scores. A total of 18 (78.3%) patients were considered responders to SLIT after 6 months (Fig. 2).
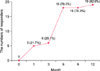
In contrast, there were no significant differences in age, gender, disease duration, severity, total IgE level, and positivity to DP/DF between responders and non-responders after 12 months (p>0.05) (data not shown). Total and specific IgE serum levels did not show significant reduction (p>0.05; Fig. 3, 4). The reduction in EASI scores between the mono-sensitized and poly-sensitized groups was not significantly different (p>0.05; Fig. 5). During the treatment, no patients experienced serious adverse events, with the exception of two patients who suffered from transient lip and tongue swelling. The above minor adverse effects disappeared spontaneously without treatment.
AD is a T-cell-mediated chronic inflammatory skin disease associated with cutaneous hyperreactivity to environmental antigens, such as HDM6. The mechanism of action underlying SLIT with DF extract is hyposensitization to the allergen. SLIT leads to decreased numbers of specific T cells, increased production of interleukin-10, and enhanced protection from DF-induced skin inflammation7.
The indication of SLIT in allergic rhinitis and asthma is well-established in adults and children, regardless of the allergen considered8. However, there have been few studies investigating the use of SLIT for AD. Recently, a few studies34910 have reported that SLIT resulted in clinically significant improvements in those with AD compared to those in healthy individuals (Table 2). Our study demonstrated a significant reduction of EASI scores, which supports the results of these previous reports. Cadario et al.4 reported that 51 patients (51/86, 59.3%) responded to SLIT after 12 months. In our study, the responder/non-responder ratio was higher than that in a previous report4. We think that the reason for this high ratio of responders in our study may be partially because we allowed patients to use topical treatment and rescue medication for AD exacerbations. However, despite these biases in our study, SLIT showed favorable results for treating patients with AD.
There is no gold standard serological or laboratory test for assessing the severity of AD. However, several studies of specific immunotherapy for AD reported changes in levels of IgE, IgG4, and cytokines in the blood11. While Cadario et al.4 presented that total and specific IgE values decreased significantly after SLIT, other researchers512 reported no significant difference in IgE values. Our study showed that the levels of total and allergen-specific IgE remained unchanged during treatment. Serum IgE levels are thought to correlate with the severity of AD, but additional studies are still needed to identify the influence of specific immunotherapy on IgE levels.
Criteria for the selection of SLIT indicate that mono-sensitized patients are ideal candidates13. However, our results demonstrated that the reduction in EASI scores between the mono-sensitized and poly-sensitized groups were not significantly different. Moreover, SLIT with mixed DP and DF extract showed a similar effect on poly-sensitized patients with AD in our study. As the sample size of the current study was relatively small, and there have been few clinical trials of SLIT in poly-sensitized AD patients, more clinical studies are necessary to determine the efficacy of SLIT in mono- and poly-sensitized patients with AD.
SLIT is known to have a better safety profile than SCIT, and no fatality has been reported in clinical trials1415. Local side effects, such as itching or mild edema in the mouth and/or throat, have been frequently reported. Only two patients developed transient lip and tongue swelling in this study, and these adverse effects resolved when the treatment was temporarily stopped. Moreover, we did not observe any serious systemic reactions or anaphylaxis. Three dropped out patients experienced an exacerbation of AD from the result. Rather than stopping cyclosporine, we assume that SLIT itself may have influenced on exacerbation as it was mostly identified after every re-administration of SLIT.
In conclusion, our study shows that SLIT with HDM extracts is effective and tolerable in Korean patients with AD, as shown by the significant overall reduction of EASI scores. Additional controlled long-term trials with larger patient populations are required to reinforce these current results in Korea.
Figures and Tables
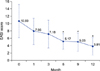 | Fig. 1Changes in eczema area and severity index (EASI) scores during sublingual immunotherapy (n=23). *Statistical analysis was performed using using Mann-Whitney test showing significant difference (p<0.05). |
 | Fig. 3Changes of total immunoglobulin E (IgE) serum levels during sublingual immunotherapy (SLIT) (n=23). *Statistical analysis was performed using Mann-Whitney test. |
 | Fig. 4Changes of specific anti-house dust mite immunoglobulin E serum levels during sublingual immunotherapy (SLIT) (n=23). *Statistical analysis was performed using Mann-Whitney test. DP: Dermatophagoides pteronyssinus, DF: D. farinae. |
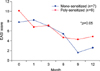 | Fig. 5Changes of specific anti-house dust mite immunoglobulin E serum levels during sublingual immunotherapy. *The differences of reduction in eczema area and severity index (EASI) score between monosensitized and polysensitized group was analyzed statistically by using Mann-Whitney test. Mono-sensitized patients: sensitized to only Dermatophagoides pteronyssinus and D. farinae. Poly-sensitized patients: simultaneously sensitized to house dust mite and other allergens proven by multiple allergen simultaneous test (Grade ≥3). |
Table 1
Demographics and baseline characteristics (n=23)

Table 2
Efficacy of specific sublingual immunotherapy for AD in previous studies

| Study, year | Total number of patients | Age (range, yr) | Types of allergen used | Duration of treatment (mo) | Results |
|---|---|---|---|---|---|
| Cadario et al.4 (2007) | 86 | 3~60 | HDM | 12 | A total of 51 patients (51/86, 59.3%) had a significant improvement defined by a SCORAD reduction of >30%. |
| Pajno et al.10 (2007) | 56 | 5~16 | HDM | 18 | A significant improvement of SCORAD from baseline was seen only in the active group. |
| Qin et al.3 (2014) | 107 | 18~46 | DF | 12 | A total efficacy rate of 77.78% (35 of 45) was significantly higher than 53.85% (21 of 39) in the control group. |
| Di Rienzo et al.9 (2014) | 27 | 5~18 | HDM | 18 | A significant improvement of SCORAD from baseline was seen only in the treated group. |
| Present study | 34 | 9~38 | HDM | 12 | A total of 19 patients (19/23, 82.6%) had a significant improvement defined by a EASI score reduction of >30%. |
References
1. Pajno GB. Sublingual immunotherapy: the optimism and the issues. J Allergy Clin Immunol. 2007; 119:796–801.
2. Bae JM, Choi YY, Park CO, Chung KY, Lee KH. Efficacy of allergen-specific immunotherapy for atopic dermatitis: a systematic review and meta-analysis of randomized controlled trials. J Allergy Clin Immunol. 2013; 132:110–117.

3. Qin YE, Mao JR, Sang YC, Li WX. Clinical efficacy and compliance of sublingual immunotherapy with Dermatophagoides farinae drops in patients with atopic dermatitis. Int J Dermatol. 2014; 53:650–655.

4. Cadario G, Galluccio AG, Pezza M, Appino A, Milani M, Pecora S, et al. Sublingual immunotherapy efficacy in patients with atopic dermatitis and house dust mites sensitivity: a prospective pilot study. Curr Med Res Opin. 2007; 23:2503–2506.

5. Silny W, Czarnecka-Operacz M. Specific immunotherapy in the treatment of patients with atopic dermatitis--results of double blind placebo controlled study. Pol Merkur Lekarski. 2006; 21:558–565.
6. Bieber T. Atopic dermatitis. N Engl J Med. 2008; 358:1483–1494.
7. Vanbervliet B, Tourdot S, Mascarell L, Rouzaire P, Vocanson M, Rozières A, et al. SLIT prevents the development of eczema in percutaneous allergen-sensitized mice. J Invest Dermatol. 2012; 132:244–246.

8. Passalacqua G, Compalati E, Canonica GW. Sublingual immunotherapy: clinical indications in the WAO-SLIT position paper. World Allergy Organ J. 2010; 3:216–219.

9. Di Rienzo V, Cadario G, Grieco T, Galluccio AG, Caffarelli C, Liotta G, et al. Sublingual immunotherapy in mite-sensitized children with atopic dermatitis: a randomized, open, parallel-group study. Ann Allergy Asthma Immunol. 2014; 113:671–673.e1.

10. Pajno GB, Caminiti L, Vita D, Barberio G, Salzano G, Lombardo F, et al. Sublingual immunotherapy in mite-sensitized children with atopic dermatitis: a randomized, double-blind, placebo-controlled study. J Allergy Clin Immunol. 2007; 120:164–170.

11. Novak N. Allergen specific immunotherapy for atopic dermatitis. Curr Opin Allergy Clin Immunol. 2007; 7:542–546.

12. Werfel T, Breuer K, Ruéff F, Przybilla B, Worm M, Grewe M, et al. Usefulness of specific immunotherapy in patients with atopic dermatitis and allergic sensitization to house dust mites: a multi-centre, randomized, dose-response study. Allergy. 2006; 61:202–205.

13. Canonica GW, Bousquet J, Casale T, Lockey RF, Baena-Cagnani CE, Pawankar R, et al. Sub-lingual immunotherapy: world allergy organization position paper 2009. World Allergy Organ J. 2009; 2:233–281.
14. Cox LS, Larenas Linnemann D, Nolte H, Weldon D, Finegold I, Nelson HS. Sublingual immunotherapy: a comprehensive review. J Allergy Clin Immunol. 2006; 117:1021–1035.

15. Gómez Vera J, Flores Sandoval G, Orea Solano M, López Tiro J, Jiménez Saab N. Safety and efficacy of specific sublingual immunotherapy in patients with asthma and allergy to Dermatophagoides pteronyssinus. Rev Alerg Mex. 2005; 52:231–236.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download