Abstract
Purpose
Patients with a history of radiocontrast media (RCM) hypersensitivity can be overlooked, resulting in repeated reactions. Therefore, a consultation support system for RCM hypersensitivity has been in operation at Seoul National University Bundang Hospital since December 2011. We analyzed the effect of this system on physicians' practice.
Methods
A retrospective study was conducted on patients with previous RCM reactions (December 1, 2010 to November 30, 2012). The control period was December 2010 to November 2011, and the intervention period was December 2011 to November 2012. The primary outcome was the composite outcome of premedication and consultation. Premedication was defined as preventive medication prescribed by the physician who ordered RCM-enhanced computed tomography (CT) at the same time. The secondary outcome was the recurrence rate after using the consultation support system.
Results
A total of 189 clinicians prescribed 913 CT scans during the control period and 225 clinicians performed 1,153 examinations during the intervention period. The odds ratio (OR) of achieving the composite outcome increased significantly after use of the consultation support system (OR, 1.54; 95% confidence interval [CI], 1.15–2.05). Clinicians in both medical (OR, 1.48; 95% CI, 1.06–2.07) and surgical (OR, 2.07; 95% CI, 1.24–3.46) departments showed significant changes in their behavior, whereas those in the emergency department did not (OR, 1.07; 95% CI, 0.41–2.78). Professors (OR, 1.47; 95% CI, 1.06–2.04) and trainees (OR, 1.97, 95% CI, 1.22–3.18) showed significant changes in their behavior toward patients with previous RCM reactions. The behavior of 86 clinicians who ordered CT scans during both the control and intervention periods was unchanged.
Iodinated radiocontrast media (RCM) are among the most common causes of immediate-type drug hypersensitivity reactions, such as anaphylaxis in both adults and children.12345 The most important risk factor for RCM hypersensitivity is a previous reaction to RCM.678 The risk of RCM hypersensitivity increases about 11-fold for patients with previous RCM hypersensitivity compared with those without a history of RCM hypersensitivity. 91011 Thus, the best way to reduce the incidence of RCM reactions among patients with previous RCM hypersensitivity is to avoid re-exposure. However, a history of RCM hypersensitivity is often overlooked in a busy real-world clinical setting.612
Considerable effort has been devoted to helping the physicians identify patients with drug allergies, including RCM hypersensitivity since the widespread adoption of electronic medical records (EMRs). An electronic alert system can enhance patient safety; however, too many alerts lead to “alert fatigue” and an overriding of computer-generated alerts.1314 Thus, an evaluation of a drug-allergy alert system should include whether the system detects patients at risk, promotes changes in physician behavior, and is associated with actual reductions in the incidence of drug allergies.
We previously reported on the effectiveness of a RCM hypersensitivity alert system embedded in our EMR.15 Our RCM hypersensitivity alert system communicates with physicians through a pop-up window when they prescribe a RCM-enhanced computed tomography (CT) scan for a patient with previous RCM hypersensitivity. Then, they could decide whether to consult to an allergist, prescribe premedication themselves, or ignore the pop-up window and keep ordering RCM-enhanced CT scan. Further details of our consultation support system have been described elsewhere.15 Our consultation support system has worked excellently and significantly decreased the incidence of RCM hypersensitivity (odds ratio [OR], 0.59; 95% confidence interval [CI], 0.49–0.71; P<0.001) according to our analysis using a generalized estimating equation (GEE) to adjust for repeated exposure. However, we failed to show a reduction in the occurrence of breakthrough reactions among patients with previous RCM hypersensitivity and could not explain the reason for the reduced incidence rate. We speculate that physician awareness of RCM hypersensitivity can be changed in the context of the increased opportunities to access information about RCM hypersensitivity afforded by the EMR system. Awareness of RCM hypersensitivity may change the behaviors of physicians, which may decrease the incidence of RCM hypersensitivity. In this study, we directly confirmed changes in physician behavior toward patients with a RCM reaction following adoption of our consultation support system.
The subjects were physicians who worked at Seoul National University Bundang Hospital (SNUBH) between December 1, 2010 and November 30, 2012. The clinical behaviors of the physicians, such as consulting with specialists or premedicating, when they ordered a RCM-enhanced CT scans for patients with previous RCM hypersensitivity were evaluated. The 2-year study period was divided into 2 one-year periods of before and after December 1, 2011, which was when our consultation support system was started. The first year was designated as the baseline period and the second year was designated as the intervention period. The frequency of consulting with a specialist and premedicating when ordering a RCM-enhanced CT scan for a patient with previous RCM hypersensitivity, the specialty and career stage of the ordering physician, and the occurrence of a breakthrough reaction were compared between the 2 periods.
Data on RCM hypersensitivity were collected from the hospital information center and the Department of Radiology as described previously.15 In short, a list of all CT scans performed during the 2-year study period was collected from the SNUBH Medical Information Center. This dataset included the identification number, specialty and career stage of the ordering physician, the identification number, sex, and age of the patient; and the premedication regimen, including antihistamines and systemic steroids. A problem-reporting sheet was completed by the trained attending nurse in the Department of Radiology. The problem-reporting sheet included all previous and current problems related to radiological examinations, including previous RCM hypersensitivity. The severity of reaction was classified as previously reported.13 Mild reactions included urticaria, flushing, pruritus, chills, and rhinitis symptoms. Moderate-to-severe reactions included angioedema, dizziness, dyspnea, gastrointestinal symptoms, anaphylaxis, loss of consciousness, and desaturation. As the recommended premedication regimen for each did not differ, we did not separate moderate and severe reactions.
Continuous variables are described in terms of means and standard deviations, whereas counts and proportions were used to describe categorical variables. The predefined desirable behaviors of physicians toward patients with previous RCM hypersensitivity when ordering a RCM-enhanced CT scan were consulting with an allergy specialist (‘consultation’ variable) and/or prescribing premedication according to the severity of the previous reaction (‘premedication’ variable). The main variable of interest was achievement of the composite endpoint of desirable behaviors (consultation, premedication, or both) after introduction of the consultation support system. To account for the correlation between multiple actions of the same physician, GEEs were used with a binary logit link function and an autoregressive (1) correlation structure. Consultation and premedication were also analyzed separately. The age and sex of the patients, the number of exposures to RCM after the first RCM hypersensitivity episode, the severity of the previous reactions and the specialty and career stage of the ordering physician were adjusted. Physicians were divided into medical, surgical, and emergency specialty groups: internal medicine, pediatrics, neurology, family medicine, and neuropsychiatry were included in the medical group, and general surgery, neurosurgery, thoracic surgery, plastic surgery, otolaryngology, and ophthalmology were included in the surgical group. Emergency medicine specialists were treated separately because the emergency department setting itself could affect physician behavior. Career stage was divided into faculty and trainee: professors and clinicians were included in the faculty category, and residents and interns were included in the trainee category. As trainees usually rotated through several hospitals (e.g., Seoul National University Hospital, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, etc.), their stay at SNUBH was usually only a few months per year, although this depended on the department. Other variables of interest were differences in the endpoint of consultation and premedication and the occurrence of a breakthrough reaction before and after the start of the consultation support system. IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA) software was used for the statistical analysis, and P values <0.05 were considered significant. This study was approved by the Institutional Review Board of SNUBH (IRB No. B-1210/174-102).
A total of 142,483 examinations were performed during the study period. Among them, 2,066 (913 and 1,153 during the baseline and intervention periods, respectively) were ordered by 328 physicians for 882 patients with previous RCM hypersensitivity. During the baseline and intervention periods, 191 and 227 physicians, respectively, ordered RCM-enhanced CT scans for patients with a history of RCM hypersensitivity. During both the baseline and intervention periods, 86 physicians ordered RCM-enhanced CT scans for patients with previous RCM hypersensitivity. About 67% of physicians were trainees, and 33% were faculty members. There were 155 physicians in the medical, 122 in the surgical and 51 in the emergency groups. Physicians ordered RCM-enhanced CT scans for patients with previous RCM hypersensitivity a median of 2 times during the study period. However, some physicians ordered as many as 198 RCM-enhanced CT scans during the 2-year study period. Of the 882 patients with previous RCM hypersensitivity, 523 and 621 underwent RCM-enhanced CT scans during the baseline and intervention periods, respectively. The severity of the previous reaction was mild in about 50%, moderate-to-severe in about 30%, and unknown in about 20% of patients (Table 1).
The composite outcome of desirable behavior was achieved in 26% and 37.1% of physicians during the baseline and intervention periods, respectively (Figure A). The GEE analysis confirmed that the OR for achieving the composite outcome increased significantly after initiating the consultation support system (OR, 1.71; 95% CI, 1.36–2.15; P <0.001; Table 2). After adjusting for possible covariates, the association remained significant (OR, 1.54; 95% CI, 1.15–2.05; P=0.003; Table 2). The consultation rate increased significantly (OR, 4.64; 95% CI, 2.64–8.15; P<0.001) after introduction of the system; however, the rate of premedication did not (OR, 1.18; 95% CI, 0.93–1.50; P=0.180; Supplementary Tables 1 and 2) when these 2 factors were analyzed separately. To assess the effect of specialty on behavioral change, the physicians were stratified according to specialty. The rate of achieving the outcome tended to increase similarly in the medical and surgical groups. The multivariate analysis using the GEE revealed an increased OR for achieving the composite outcome after the initiating the consultation support system in the medical (OR, 1.48; 95% CI, 1.06–2.07; P=0.020) and surgical (OR, 2.07; 95% CI, 1.24–3.46; P=0.006), but not in the emergency (OR, 1.07; 95% CI, 0.41–2.78; P=0.900) groups (Figure B, Supplementary Table 3). The rate of achieving the composite outcome increased in both career groups after initiating the consultation support system, and the trainee group showed a striking increase in the consultation rate during the intervention period. Interestingly, the trainee group showed better outcomes than did the faculty group for almost all outcomes during both the baseline and intervention periods (Figure C). The multivariate analysis using the GEE confirmed that the OR for achieving the composite outcome increased significantly in the faculty (OR, 1.47; 95% CI, 1.06–2.04; P=0.020) and trainee (OR, 1.97; 95% CI, 1.22–3.18; P=0.006) groups after initiating the consultation support system (Supplementary Table 4).
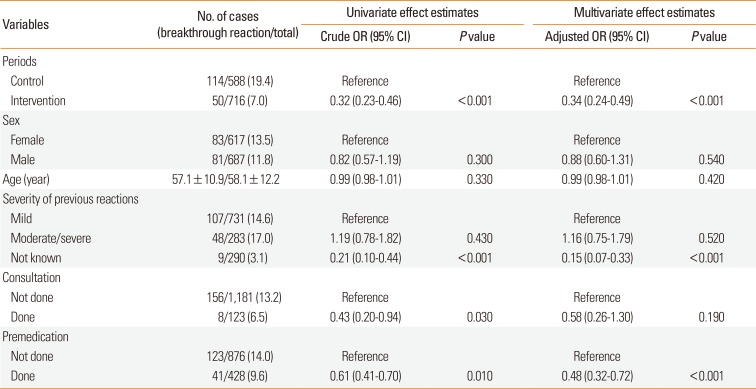
The occurrence rate of a breakthrough reaction was compared between the baseline and intervention periods using only the examinations with known results of RCM re-exposure. In total, 588 examinations during the baseline and 713 during the intervention period were identified, and several demographic differences were detected between the patients in the 2 groups (Supplementary Table 5). The frequency of the occurrence of a breakthrough reaction dropped from 19.4% to 7.0% between the baseline and the intervention periods. The GEE analysis indicated that the decrease was significant in both the univariate (OR, 0.32; 95% CI, 0.23–0.46; P<0.001) and multivariate analyses (OR, 0.34; 95% CI, 0.24–0.49; P<0.001; Table 3).
Outcomes were analyzed according to the severity of the previous reaction. The rate of achieving a composite outcome in patients with mild previous reaction increased from 36% (177/491) to 48% (302/629) between the baseline and the intervention periods (P<0.001). The rate in patients with moderate to severe reaction also increased from 23.3% (60/257) to 31.1% (98/315) after the initiation of consultation support system (P=0.040). However, this increase in achieving a composite outcome was not significant after adjustment for multiple exposure. The breakthrough reaction decreased from 24.1% (79/328) to 6.9% (28/403) for patients with mild previous reaction (P<0.001) and from 22.3% (29/130) to 12.4% (19/153) for those with moderate to severe reaction (P=0.03) after the initiation of consultation support system. The decrease in the breakthrough reaction remained significant after adjustment for multiple comparison (OR, 4.05; 95% CI, 2.56–6.40; P<0.001 for mild previous reaction; OR, 2.08; 95% CI, 1.16–3.71; P=0.010 for moderate to severe previous reaction), but not after adjustment for other covariates.
The results were similar when only the 86 physicians who ordered RCM-enhanced CT scans for patients with previous RCM hypersensitivity during both the baseline and intervention periods were analyzed (data not shown). The OR of achieving the composite outcome after initiating the consultation support system was 1.47 (95% CI, 1.04–2.08; P=0.030) in the multivariate analysis using the GEE for the 86 physicians. The occurrence of a breakthrough reaction when analyzed with 86 physicians reduced even more than the rate when the analysis was restricted to these 86 physicians (OR, 0.27; 95% CI, 0.18–0.42; P<0.001).
In this study, we showed that our consultation support system effectively promoted desirable behaviors of physicians toward patients with previous RCM hypersensitivity with regard to ordering RCM-enhanced CT scans. Moreover, the improved behavior seemed to actually reduce the rate of breakthrough reactions.
Our consultation support system improved the rate of specialist consultations and the frequency of prescribing premedication, suggesting good compliance with the system. System compliance and clinical outcomes of interest should be evaluated when assessing a clinical decision support system (CDSS). A recent systematic review assessed the effectiveness of several CDSSs and concluded that CDSSs generally improve preventive measures, such as vaccination, ordering appropriate tests, and prescribing the proper medication.16 Studies focused on ordering the proper medication usually adopted the program on their preexisting EMR, which was the case for our system; thus, generalization of the results is not possible. However, as the quality of the studies is good and the results indicate that all programs achieved their pre-established outcomes, they concluded that strong evidence demonstrates that such CDSSs can help physicians order proper medication. The OR of ordering proper medication was 1.57 (95% CI, 1.35–1.82) in that meta-analysis, which is similar to that in this study (OR, 1.54; 95% CI, 1.15–2.05).
The strength of the present study was that we showed an actual decline in the occurrence of breakthrough reactions as well as enhanced physician compliance. Two recent studies from Korea evaluated the effects of RCM reaction alert systems on EMRs. Bae et al.17 reported the effectiveness of their EMR-embedded RCM reaction alert system, which provides details of previous reaction-like symptoms and severity and suggests a recommended premedication regimen according to the severity of the previous reaction; this recommendation appears in a pop-up window when the patient is prescribed RCM-enhanced imaging tests. Although they did not consider the effect of repeated exposure to the system, they found a significant reduction in the occurrence of breakthrough reactions (from 15.2% to 6.7%) and an increase in the rate at which systemic steroids were prescribed (from 14% to 65%) as a premedication after adopting the system. Although we took repeated measures into consideration in our previous study, we could not show direct improvements in physician behaviors.15 Two steps are needed to effectively reduce the occurrence of a breakthrough reaction. First, physician compliance must be enhanced and premedication that is effective in preventing the breakthrough reaction must be administered. The effectiveness of premedication in preventing RCM hypersensitivity in a patient with previous hypersensitivity remains controversial.18 The effects of such premedication were significant in this study among the entire sample (OR, 0.59; 95% CI, 0.40–0.88; P=0.010 by GEE analysis adjusting for age and sex), among patients with a previous mild reaction (OR, 0.47; 95% CI, 0.29–0.76; P=0.002 by GEE analysis adjusting for age and sex), and among patients with moderate-to-severe previous reactions (OR, 0.36; 95% CI, 0.17–0.76; P=0.008 by GEE analysis adjusting for age and sex). On the other hand, consultation itself did not affect the occurrence of a breakthrough reaction in multivariate analysis. This might be explained by the small number of consultation. Also, there was a possibility that the patient did not visit the allergists' office even after the consultation.
In this study, we showed the effectiveness of our system in achieving composite outcomes in patients with mild previous reaction but not in those with moderate to severe previous RCM reaction. There can be a few explanations for this failure in improving physicians' behavior to patients with moderate to severe previous reaction. First, there was a possibility that physicians had already consulted the patients with moderate to severe previous reaction to the allergist even before the initiation of the study. In other words, there was no significant change in behavior because the physicians had already been doing well. Secondly, as the optimal premedication for patients with moderate to severe previous reaction was intravenous antihistamine and systemic corticosteroid simultaneously, it could be harder to prescribe the right regimen to them than to those with mild ones. Actually, the rate for achieving composite outcome in patients with mild previous reaction was always higher than that with moderate to severe one regardless of the initiation of consultation support system. We also failed to show the decrease in the breakthrough reaction in patients with moderate to severe previous reaction. This might be because the number of breakthrough reactions was too small. The rate of breakthrough reaction in this study was only 0.03% (48/142,483 exposure) in patients with moderate to severe previous reaction. Thus, to examine the efficacy of preventive measure for patients with moderate to severe previous reaction, it would be necessary to conduct a very large multicenter trial.
The specialty and career stage of physicians seemed to affect their compliance, and social and traditional factors may have influenced these results. The data from the emergency group differed from those of the medical and surgical groups. Although it would be inappropriate to draw conclusions because the number of CT scans ordered by the emergency group was relatively small, it might be easier for emergency physicians to overlook CT scans because of the emergency setting.14 Our consultation support system enhanced desirable behaviors, regardless of the career stage of physicians. Trainees were more accepting than faculty members of the change in their practice pattern.
This study has several limitations. Because of the retrospective design of this study, we could not identify patients who had undergone alternative examination such as magnetic resonance imaging and ultrasound. Although changing RCM is recognized as a good way to prevent RCM hypersensitivity,19 it was not generally recommended at the time of the study. Thus, we could not check whether they changed RCM or not in the Radiology Department. Although the problem-reporting sheet provided information on the RCM hypersensitivity reaction, the details of RCM reactions were difficult to obtain because of the retrospective design. Risk factors other than previous RCM hypersensitivity, such as type of RCM, presence of atopy or asthma, and concomitant use of medications, such as β-adrenergic blockers, were not included in the analysis.620 However, we tried to overcome this shortcoming by including a large number of patients and adjusting for the variables that we could collect. We adjusted for events that were correlated due to the repeated exposures by using a GEE. However, the strength of evidence was weaker than that provided by a well-designed prospective study.
In conclusion, a consultation support system to prevent RCM hypersensitivity was effective in changing physicians' practice patterns and in decreasing recurrent RCM reactions.
References
1. Park CS, Kim TB, Kim SL, Kim JY, Yang KA, Bae YJ, et al. The use of an electronic medical record system for mandatory reporting of drug hypersensitivity reactions has been shown to improve the management of patients in the university hospital in Korea. Pharmacoepidemiol Drug Saf. 2008; 17:919–925. PMID: 18470952.

2. Kim MH, Park CH, Kim DI, Kim KM, Kim HK, Lim KH, et al. Surveillance of contrast-media-induced hypersensitivity reactions using signals from an electronic medical recording system. Ann Allergy Asthma Immunol. 2012; 108:167–171. PMID: 22374199.

3. Yang MS, Lee SH, Kim TW, Kwon JW, Lee SM, Kim SH, et al. Epidemiologic and clinical features of anaphylaxis in Korea. Ann Allergy Asthma Immunol. 2008; 100:31–36. PMID: 18254479.

4. Ye YM, Kim MK, Kang HR, Kim TB, Sohn SW, Koh YI, et al. Predictors of the severity and serious outcomes of anaphylaxis in Korean adults: a multicenter retrospective case study. Allergy Asthma Immunol Res. 2015; 7:22–29. PMID: 25553259.

5. Lee SY, Ahn K, Kim J, Jang GC, Min TK, Yang HJ, et al. A multicenter retrospective case study of anaphylaxis triggers by age in Korean children. Allergy Asthma Immunol Res. 2016; 8:535–540. PMID: 27582405.

6. Katayama H. Adverse reactions to contrast media. What are the risk factors? Invest Radiol. 1990; 25(Suppl 1):S16–S17. PMID: 2283239.

7. Caro JJ, Trindade E, McGregor M. The risks of death and of severe nonfatal reactions with high- vs low-osmolality contrast media: a meta-analysis. AJR Am J Roentgenol. 1991; 156:825–832. PMID: 1825900.

8. Bettmann MA, Heeren T, Greenfield A, Goudey C. Adverse events with radiographic contrast agents: results of the SCVIR Contrast Agent Registry. Radiology. 1997; 203:611–620. PMID: 9169677.

9. Witten DM, Hirsch FD, Hartman GW. Acute reactions to urographic contrast medium: incidence, clinical characteristics and relationship to history of hypersensitivity states. Am J Roentgenol Radium Ther Nucl Med. 1973; 119:832–840.
10. Shehadi WH. Adverse reactions to intravascularly administered contrast media. A comprehensive study based on a prospective survey. Am J Roentgenol Radium Ther Nucl Med. 1975; 124:145–152.
11. Ansell G, Tweedie MC, West CR, Evans P, Couch L. The current status of reactions to intravenous contrast media. Invest Radiol. 1980; 15:S32–S39. PMID: 7203943.

12. Segal AJ, Bush WH Jr. Avoidable errors in dealing with anaphylactoid reactions to iodinated contrast media. Invest Radiol. 2011; 46:147–151. PMID: 21150793.

13. Hsieh TC, Kuperman GJ, Jaggi T, Hojnowski-Diaz P, Fiskio J, Williams DH, et al. J Am Med Inform Assoc. 2004; 11:482–491. PMID: 15298998.
15. Yang MS, Choi SI, Song WJ, Kim SH, Kang HR, Park HW, et al. Impact of an electronic consultant system on hypersensitivity reactions to iodinated radiocontrast media: an observational study. Postgrad Med J. 2015; 91:193–199. PMID: 25737564.

16. Shojania KG, Jennings A, Mayhew A, Ramsay C, Eccles M, Grimshaw J. Effect of point-of-care computer reminders on physician behaviour: a systematic review. CMAJ. 2010; 182:E216–E225. PMID: 20212028.

17. Bae YJ, Hwang YW, Yoon SY, Kim S, Lee T, Lee YS, et al. The effectiveness of automatic recommending system for premedication in reducing recurrent radiocontrast media hypersensitivity reactions. PLoS One. 2013; 8:e66014. PMID: 23840391.

18. Tramèr MR, von Elm E, Loubeyre P, Hauser C. Pharmacological prevention of serious anaphylactic reactions due to iodinated contrast media: systematic review. BMJ. 2006; 333:675–680. PMID: 16880193.

19. Park HJ, Park JW, Yang MS, Kim MY, Kim SH, Jang GC, et al. Re-exposure to low osmolar iodinated contrast media in patients with prior moderate-to-severe hypersensitivity reactions: a multicentre retrospective cohort study. Eur Radiol. 2017; 27:2886–2893. PMID: 27975150.

20. Thomsen HS, Webb JA. Contrast media: safety issues and ESUR guidelines. 3rd ed. Heidelberg: Springer;2014.
SUPPLEMENTARY MATERIALS
Supplementary Table 1
The effect of consultation support system on the rate of premedication prescribed by doctors when ordering a radiocontrast media enhanced CT scan to the patient with previous RCM hypersensitivity
Supplementary Table 2
The effect of consultation support system on the frequency of consultation when ordering a radiocontrast media enhanced CT scan to the patient with previous RCM hypersensitivity
Supplementary Table 3
The differences in the outcomes according to the specialties
Supplementary Table 4
The differences in the outcomes according to the career stages
Supplementary Table 5
Comparison of demographics between all examination and the examinations included in the analyses on breakthrough reactions
Figure
Comparison of the frequencies of achieving outcomes before and after the initiation of the consultation support system. The increasing trends were all similar even when subjects were differently stratified: all doctors (A), specialty group (B), and career group (C).
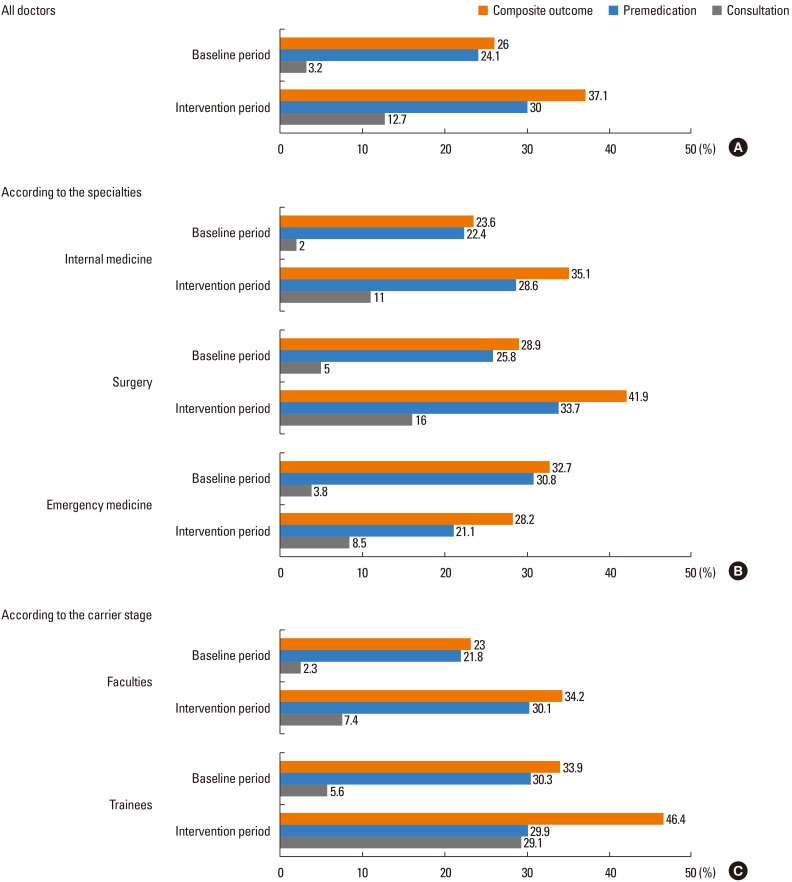
Table 1
Demographics of the study subjects
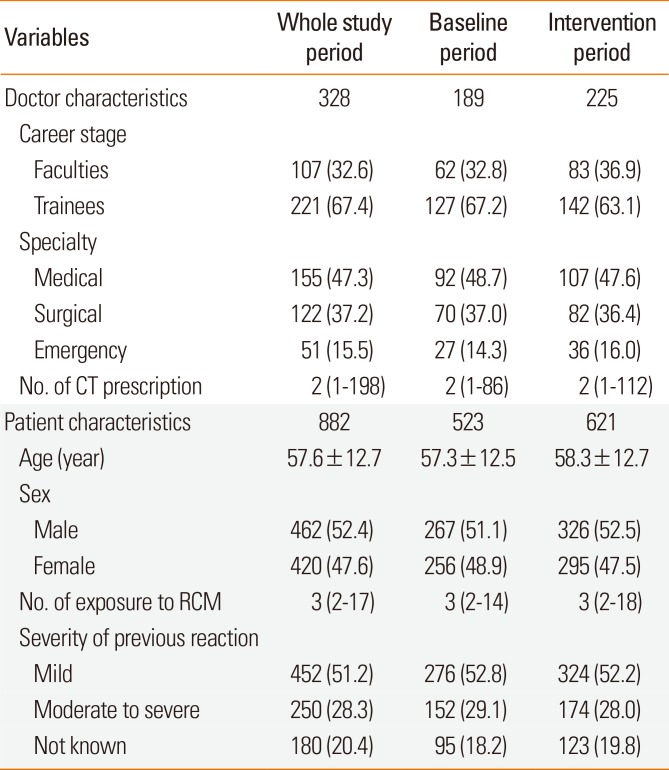
Table 2
The effect of our consultation support system on the composite outcome of desirable behaviors of doctors when ordering a radiocontrast media enhanced CT scan to the patient with previous RCM hypersensitivity
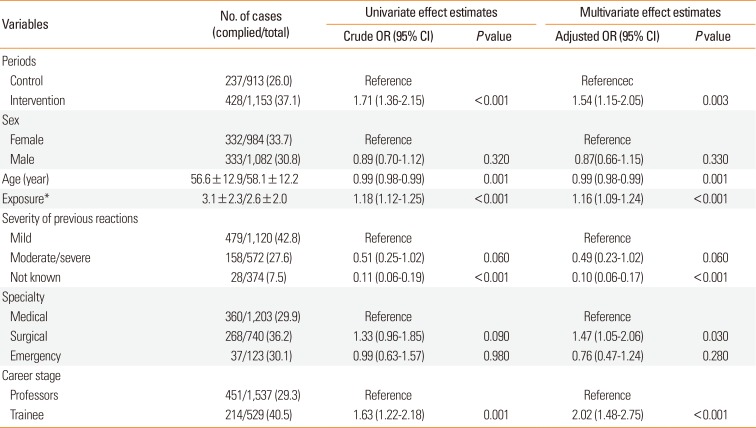
Table 3
The effect of our consultation support system on the occurrence rate of breakthrough reactions




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download