Abstract
Purpose
There have been a few reports of bizarre parosteal osteochondromatous proliferation (BPOP) in Korea to date. The purpose of this study was to investigate the etiology, diagnosis, treatment, and prognosis of BPOP and to report the clinical outcomes from a single institution.
Materials and Methods
Between 1999 and 2016, six patients who were diagnosed and treated operatively at Yeungnam University Medical Center were reviewed retrospectively. The analysis was performed using medical records, simple radiographs, magnetic resonance imaging (MRI), and pathology results, based on clinical and oncological results. All patients underwent surgical treatment for complete resection. We also analyzed one patient who was initially diagnosed with BPOP, showing different clinical features during the follow-up period.
Results
The age of patients ranged from 17 to 60 years. All patients did not show a history of trauma. All patients showed localized edema on the tumor lesion, and three patients also showed tenderness. The tumor lesions were distributed to the femur, tibia, and humerus. All patients underwent marginal resection or wide resection. The mean follow-up period was 50.3 months. There was a malignant change in one patient, but no recurrence or metastasis.
Conclusion
In this study, there was no difference in the incidence of BPOP in accordance with sex. Moreover, there was no significant relationship between trauma and onset of BPOP. Unlike previous reports, no recurrence occurred after complete resection. If BPOP is diagnosed, it is necessary to consider the possibility of malignant change and distinguish it from other malignant tumors.
Figures and Tables
Figure 1
(A) Preoperative radiographs of a 60-year-old female. The tumor was grown in the ulnar aspect of the middle phalangeal head of the index finger. (B) Postoperative radiographs.

Figure 2
(A) Radiographs of the right ankle. The anteroposterior (left) and oblique (right) views demonstrate a well-defined, exophytic bony mass attached to the lateral cortex of the metaphysis of the distal fibula. Continuity between the central part of the lesion and the medullary cavity of the fibular is absent. (B) The excised mass revealed two distinctive areas (left): An area resembling osteochondroma with a cartilaginous cap and medullary bone, as well as an unusual, gray-white, fleshy soft tissue mass (arrows) in the periphery. Note a broad base (arrowheads) attached to the cortical surface of the distal fibula. The whole mount section of the excised mass (H&E) shows an osteochondromatous area with a cartilaginous cap and medullary bone, and a fibrosarcomatous area in the periphery (right).
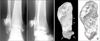
Figure 3
(A) A low-magnification view shows a cartilaginous cap maturing into the bony trabeculae (H&E, ×40). (B) A higher-magnification view shows cartilage with bizarre, enlarged nuclei and a blue tinctorial quality in the woven bone spicules (H&E, ×200). (C) A higher-magnification view shows loosely arranged spindle cells between the bony trabeculae, rimmed by osteoblasts (H&E, ×200).

Figure 4
(A) The lower part of the photomicrograph shows an osseous element of the bizarre parosteal osteochondromatous proliferation. The fibrosarcomatous area can be seen above. (B) The fibrosarcomatous area is moderately cellular with mild nuclear pleomorphism and occasional mitotic figures (A, B: H&E, ×200).

Figure 5
(A) Initial radiographs of a 24-year-old male. The exophytic osteoblastic tumor in the antero-medial aspect of the distal humerus (arrows). (B) The tumor had grown up for 3 years (arrows). (C) Postoperative radiographs and intraoperative photographs. The right distal humerus mass was excised (arrows). The biopsy result was parosteal osteosarcoma, grade 1. (D) Distal humerus was excised and tumor prosthesis inserted. Radiographs were taken postoperatively.

References
1. Nora FE, Dahlin DC, Beabout JW. Bizarre parosteal osteochondromatous proliferations of the hands and feet. Am J Surg Pathol. 1983; 7:245–250.

2. Meneses MF, Unni KK, Swee RG. Bizarre parosteal osteochondromatous proliferation of bone (Nora's lesion). Am J Surg Pathol. 1993; 17:691–697.

3. Dhondt E, Oudenhoven L, Khan S, et al. Nora's lesion, a distinct radiological entity? Skeletal Radiol. 2006; 35:497–502.

4. Fechner RE, Mills SE. Tumors of bones and joints. In : Rosai J, Leslie H, editors. Atlas of tumor pathology. Third series, Fascicle 8. Washington, DC: Armed Forces Institute of Pathology;1993. p. 268–269.
5. Gruber G, Giessauf C, Leithner A, et al. Bizarre parosteal osteochondromatous proliferation (Nora lesion): a report of 3 cases and a review of the literature. Can J Surg. 2008; 51:486–489.
6. Torreggiani WC, Munk PL, Al-Ismail K, et al. MR imaging features of bizarre parosteal osteochondromatous proliferation of bone (Nora's lesion). Eur J Radiol. 2001; 40:224–231.

7. Cooper PN, Malcolm AJ. A bizarre parosteal osteochondromatous proliferation of the radius. Histopathology. 1993; 22:78–80.

8. Kim SW, Suh JH, Shin SM, Cho BK. Bizarre parosteal osteochondromatous proliferation (Nora's lesion) of the big toe. (A report of two cases and review). J Korean Foot Ankle Soc. 2013; 17:68–73.
9. Noh HK, Jeon HS, Jeon SJ, Moon CS, Kang SG, Song GS. Bizarre parosteal osteochondromatous proliferation in the proximal phalanx of the third toe: A case report. J Korean Bone Joint Tumor Soc. 2011; 17:91–94.

10. Kim MS, Kim YH, Hwang YJ, et al. Bizarre parosteal osteochondromatous proliferation with cortical erosion in the hand: a case report. J Korean Soc Radiol. 2011; 65:415–419.

11. Horiguchi H, Sakane M, Matsui M, Wadano Y. Bizarre parosteal osteochondromatous proliferation (Nora's lesion) of the foot. Pathol Int. 2001; 51:816–823.

12. Soejima O, Isayama T, Ogata K. Extensor pollicis longus tendon rupture caused by a bizarre parosteal osteochondromatous proliferation of the wrist. Hand Surg. 1998; 3:277–281.

13. Smith NC, Ellis AM, McCarthy S, McNaught P. Bizarre parosteal osteochondromatous proliferation: a review of seven cases. Aust N Z J Surg. 1996; 66:694–697.

14. Boussouga M, Harket A, Bousselmame N, Lazrak K. Bizarre parosteal osteochondromatous proliferation (Nora's lesion) of the forefoot. Acta Orthop Belg. 2008; 74:562–565.
15. Nilsson M, Domanski HA, Mertens F, Mandahl N. Molecular cytogenetic characterization of recurrent translocation breakpoints in bizarre parosteal osteochondromatous proliferation (Nora's lesion). Hum Pathol. 2004; 35:1063–1069.

16. Unni KK. Dahlin's bone tumors: general aspects and data on 11,087 cases. 5th ed. Philadelphia: Lippincott-Raven;1996. p. 197–206.
17. Choi JH, Gu MJ, Kim MJ, Choi WH, Shin DS, Cho KH. Fibrosarcoma in bizarre parosteal osteochondromatous proliferation. Skeletal Radiol. 2001; 30:44–47.

18. Unni K, Inwards CY, Bridge JA, Kindblom L, Wold LE. Tumors of the bones and joints (Atlas of Tumor Pathology series IV). Washington, DC: American Registry of Pathology;2005. p. 324–330.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download