Abstract
Purpose
To describe the technical skills and to estimate the clinical outcomes of port-hole decompression preserving the posterior ligaments during lumbar spinal stenosis surgery.
Materials and Methods
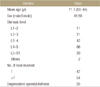
Between March 2014 and March 2016, a total of 101 patients who underwent port-hole decompression were retrospectively analyzed. The mean age was 71.3 years (58–84 years) and there were 46 males and 55 females. The mean follow-up period was 18 months. Degenerative spondylolisthesis was observed in 24.8% of patients (25/101). Port-hole decompression was performed by removing the central portion of the distal part of the upper lamina with a burr. Then, the contralateral side of ligamentum flavum and hypertrophied facet joints were removed. We estimated the lumbar lordotic angle using radiographs, and measured the depth from skin to upper lamina central area using magnetic resonance imaging axial images. We estimated the mean slip angle and mean degree of slip in preoperative and postoperative radiography in standing flexion and extension. We also measured the operational time, length of skin incision, and blood loss. The clinical results were estimated by a walking distance caused by neurologic intermittent claudication, visual analogue scale, and Oswestry disability index.
Results
Most patients were generally older, and the mean lordotic angle was 25.3°, which is considered to be lower when compared with younger people. The mean depth from skin to lamina was mean 5.4 cm. With respect to the radiological results, there were no significant differences between the preoperative and postoperative groups. The operation time, length of skin incision, and bleeding were not increased proportionally to the operation level. The walking distance caused by neurologic intermittent claudication, visual analogue scale, and Oswestry disability index of the post-operative group were all improved compared with the pre-operative group.
Figures and Tables
Figure 1
Port-hole decompression is different from the conventional laminectomy. (A) The figure show spinal stenosis with thickened ligamentum flavum and hypertrophied facet joints. (B) The figure show resected posterior ligaments and medial facets in conventional laminectomy. (C) The figure show the port-hole decompression preserving posterior ligaments and facet joints which are important for segmental stability.

Figure 2
Intraoperative photograph of port-hole decompression, showing fully decompressed dura after the removal of hypertrophied ligamentum flavum and preserved posterior ligaments (arrow).

Figure 3
Preoperative and postoperative magnetic resonance imaging (MRI). Sagittal (A), axial L3-4 (B), and axial L4-5 (C) preoperative MRI of the patient with degenerative spondylolisthesis. Sagittal (D), axial L3-4 (E), and axial L4-5 (F) postoperative MRI of the patient shows removed ligamentum flavum and preserved posterior ligament after port-hole decompression.

Figure 4
Axial magnetic resonance imaging suggesting the depth of the operating field. It is estimated by the distance between the skin and central lamina inner surface at the axial image of the disc level.

References
1. Kleeman TJ, Hiscoe AC, Berg EE. Patient outcomes after minimally destabilizing lumbar stenosis decompression: the “Port-Hole” technique. Spine (Phila Pa 1976). 2000; 25:865–870.
2. Chatani K. A novel surgical approach to the lumbar spine involving hemilateral split-off of the spinous process to preserve the multifidus muscle: technical note. J Neurosurg Spine. 2016; 24:694–699.

3. Reinshagen C, Ruess D, Molcanyi M, et al. A novel translaminar crossover approach for pathologies in the lumbar hidden zone. J Clin Neurosci. 2015; 22:1030–1035.

4. Kakiuchi M, Fukushima W. Impact of spinous process integrity on ten to twelve-year outcomes after posterior decompression for lumbar spinal stenosis: study of open-door laminoplasty using a spinous process-splitting approach. J Bone Joint Surg Am. 2015; 97:1667–1677.
5. Jalil Y, Carvalho C, Becker R. Long-term clinical and radiological postoperative outcomes after an interspinous microdecompression of degenerative lumbar spinal stenosis. Spine (Phila Pa 1976). 2014; 39:368–373.

6. Adachi K, Futami T, Ebihara A, et al. Spinal canal enlargement procedure by restorative laminoplasty for the treatment of lumbar canal stenosis. Spine J. 2003; 3:471–478.

7. Iguchi T, Kurihara A, Nakayama J, Sato K, Kurosaka M, Yamasaki K. Minimum 10-year outcome of decompressive laminectomy for degenerative lumbar spinal stenosis. Spine (Phila Pa 1976). 2000; 25:1754–1759.

8. Aizawa T, Ozawa H, Kusakabe T, et al. Reoperation rates after fenestration for lumbar spinal canal stenosis: a 20-year period survival function method analysis. Eur Spine J. 2015; 24:381–387.

9. Henky J, Yasuda M, Arifin MZ, Takayasu M, Faried A. Trumpet laminectomy microdecompression for lumbal canal stenosis. Asian Spine J. 2014; 8:667–674.

10. Thomé C, Zevgaridis D, Leheta O, et al. Outcome after less-invasive decompression of lumbar spinal stenosis: a randomized comparison of unilateral laminotomy, bilateral laminotomy, and laminectomy. J Neurosurg Spine. 2005; 3:129–141.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download