Abstract
Nonunion is caused by various factors related to fracture characteristics, patient characteristics, treatment, and infection. Aseptic nonunion, is divided into three categories in accordance with the biological activity of the fracture: atrophic nonunion, oligotrophic nonunion, and hypertrophic nonunion. Treatment of nonunion depends on the cause and classification. Here, we report our experiences and review the various causes of nonunion and treatment methods available.
Figures and Tables
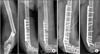 | Figure 1(A) A nonunion of distal humeral shaft with screw breakage was shown after internal fixation. (B) With the resection of bone with of poor vitality, compression plating was performed. (C) Union was achieved uneventfully. |
 | Figure 2(A) Proximal tibia shaft fracture was fixed with a thin intramedullary nail. (B) Although an abundant callus was seen, hypertrophic nonunion occurred with breakage of interlocking screws. A small diameter nail might result in insufficient mechanical stability. |
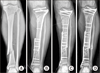 | Figure 3(A, B) For a segmental tibial shaft fracture, plate fixation was performed; however, hypertrophic nonunion occurred with insufficient numbers of screws and relatively short length of plate. (C) With the correction of alignment, more numbers of screws and a longer length of plate were fixed. (D) Complete bony union was achieved at 10 months later. |
 | Figure 4(A, B) A nonunion occurred after intramedullary nailing of proximal humeral shaft, probably from the unstable fixation with one interlocking screw at the distal segment. (C) The increase of isotope uptake shows the viability of fracture site. Compression plating was performed without bone graft (D), and bony union was achieved (E). |
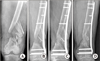
 | Figure 5(A) A plate was fixed for a segmental fracture of tibia shaft. (B) Due to the relatively short length of medial plate, hypertrophic nonunion occurred with the implant loosening. (C) Reamed intramedullary nailing was performed after removal of previous plate without bone graft. (D) Bony union was achieved after one year. |
 | Figure 6(A) Distal shaft fracture of the femur showed the hypertrophic nonunion with abundant callus formation, at 6 months after nailing. (B) To obtain additional stability, an additional interlocking screw and interference screws were added to the distal femur. (C) Complete bone union was achieved without bone graft, after 9 months. |
 | Figure 7(A, B) After intramedullary nailing for a distal femoral shaft fracture, a hypertrophic nonunion of the femur was observed, probably from insufficient working length of distal fixation. (C) An augmentation plate with the minimally invasive technique was fixed to add stability, without bone graft. (D) Solid bone union was achieved with bridging of the callus. |
 | Figure 8(A, B) An atrophic nonunion developed after static intramedullary nailing of femoral shaft fracture with a gap at the fracture site. (C) The procedure of dynamization was performed with removing the static interlocking screw at the proximal segment. (D) A complete bony union was achieved. |
 | Figure 9(A) A nonunion with segmental bone defect occurred after the management of open tibia fracture. (B, C) Bone transport over the plate was performed. (D) After the completion of bone transport, screws were fixed at the transported segment through empty holes of plate followed by the bone graft at the docking site and the removal of external fixator. (E) At 8 months, radiograph showed the consolidation at the distraction area and union at the docking site. |
 | Figure 10Nailing was done in open fracture of the distal tibia (A); however, the atrophic nonunion occurred without callus formation on the radiograph (B). Bone defect was observed at the fracture site (C), and autogenous bone graft was performed (D). (E) After 7 months, complete bone union was achieved. |
References
1. McKee MD, DiPasquale DJ, Wild LM, Stephen DJ, Kreder HJ, Schemitsch EH. The effect of smoking on clinical outcome and complication rates following Ilizarov reconstruction. J Orthop Trauma. 2003; 17:663–667.

2. Castillo RC, Bosse MJ, MacKenzie EJ, Patterson BM. LEAP Study Group. Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fractures. J Orthop Trauma. 2005; 19:151–157.

3. Giannoudis PV, MacDonald DA, Matthews SJ, Smith RM, Furlong AJ, De Boer P. Nonunion of the femoral diaphysis. The influence of reaming and non-steroidal anti-inflammatory drugs. J Bone Joint Surg Br. 2000; 82:655–658.
5. Park J, Kim SG, Yoon HK, Yang KH. The treatment of nonisthmal femoral shaft nonunions with im nail exchange versus augmentation plating. J Orthop Trauma. 2010; 24:89–94.

6. Brinker MR, O'Connor DP. Exchange nailing of ununited fractures. J Bone Joint Surg Am. 2007; 89:177–188.

7. Oh JK, Bae JH, Oh CW, Biswal S, Hur CR. Treatment of femoral and tibial diaphyseal nonunions using reamed intramedullary nailing without bone graft. Injury. 2008; 39:952–959.

8. Yang KH, Kim JR, Park J. Nonisthmal femoral shaft nonunion as a risk factor for exchange nailing failure. J Trauma Acute Care Surg. 2012; 72:E60–E64.

9. Eom TW, Kim JJ, Oh HK, Kim JW. Challenge to treat hypertrophic nonunion of the femoral shaft: the Poller screw augmentation technique. Eur J Orthop Surg Traumatol. 2016; 26:559–563.

10. Litrenta J, Tornetta P 3rd, Vallier H, et al. Dynamizations and exchanges: success rates and indications. J Orthop Trauma. 2015; 29:569–573.
11. Oh CW, Apivatthakakul T, Oh JK, et al. Bone transport with an external fixator and a locking plate for segmental tibial defects. Bone Joint J. 2013; 95:1667–1672.

12. Oh CW, Song HR, Roh JY, et al. Bone transport over an intramedullary nail for reconstruction of long bone defects in tibia. Arch Orthop Trauma Surg. 2008; 128:801–808.

13. Ziran BH, Smith WR, Morgan SJ. Use of calcium-based demineralized bone matrix/allograft for nonunions and posttraumatic reconstruction of the appendicular skeleton: preliminary results and complications. J Trauma. 2007; 63:1324–1328.

14. Masquelet AC, Fitoussi F, Begue T, Muller GP. Reconstruction of the long bones by the induced membrane and spongy autograft. Ann Chir Plast Esthet. 2000; 45:346–353.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download