Abstract
The aim of this study is to investigate the clinical outcomes of the elderly patients with Non ST-segment elevation myocardial infarction (NSTEMI) undergoing coronary artery bypass surgery (CABG) compared to non-elderly patients. Patients with NSTEMI and undergoing CABG (n=451) who were registered in the Korea Acute Myocardial Infarction Registry between December 2003 and August 2012 were divided into two groups.; the non-elderly group (<75 years, n=327) and the elderly group (≥75 years, n=124). In-hospital mortality was higher in the elderly group (4.9% vs. 11.3%, p=0.015), but cardiac death, myocardial infarction, and major adverse cardiovascular events (MACE) including cardiac death, myocardial infarction, percutaneous revascularization, and redo-CABG after a one-year follow up were not different between the two groups. Predictors of in-hospital mortality in patients with NSTEMI undergoing CABG were left ventricular (LV) dysfunction (ejection fraction ≤40%) [hazard ratio (HR): 2.76, 95% confidence interval (CI): 1.16–6.57, p=0.022] and age (HR: 1.05, 95% CI: 1.01–1.10, p=0.047). So elderly NSTEMI patients should be considered for CABG if appropriate, but careful consideration for surgery is required, especially if the patients have severe LV systolic dysfunction.
As the technique and equipment of percutaneous coronary intervention (PCI) have improved, PCI has replaced coronary artery bypass surgery (CABG) for treating patients with acute myocardial infarction (AMI) and complex coronary lesions such as left main and multi-vessel disease. However, CABG is still reserved for left main, and/or 3-vessel disease, failed PCI, and coronary anatomy not amenable to PCI, based on the patient's clinical status, comorbidities, and disease severity including lesion distribution and angiographic lesion characteristics.1 In other words, PCI dose not completely replace CABG in treating patients with AMI and complex coronary lesions.
In the case of elderly patients, however, they often have, more comorbid conditions2 so it is not easy for them to undergo surgery, despite the fact that CABG has been getting safer owing to the improvement in surgical techniques and pharmacology. The greatest risk is in the elderly patients for whom the CABG operation may be the best of several high-risk options.3 It can lead them and their families to hesitate about whether to have the operation.
So the authors investigated the clinical outcomes of the Korean elderly patients with NSTEMI undergoing CABG compared to non-elderly patients. Patients with ST-segment elevation myocardial infarction (STEMI) were excluded in this study, because primary PCI is almost always the main strategy in treating these kinds of patients.
The Korea Acute Myocardial Infarction Registry (KAMIR) is a Korean prospective multicenter online registry designed to describe characteristics and clinical outcomes of Korean patients with AMI.4 Data was collected by an experienced study coordinator based on a standardized protocol, and the study was approved by the ethics committee at each participating institution.
From December 2003 to August 2012, 451 NSTEMI patients undergoing CABG during index hospitalization were enrolled from the KAMIR. Patients were divided into two groups according to the age; 327 patients were non-elderly (<75 years), and 124 patients were elderly (≥75 years).
Elderly was defined as individuals ≥75 years of age. The previous American College of Cardiology/American Heart Association (ACC/AHA) practice guidelines categorize elderly patients as a special at-risk group.156 Acute myocardial infarction was defined by clinical signs or symptoms, increased cardiac biomarkers, and 12-lead electrocardiographic findings.7 Non-ST segment elevation myocardial infarction (NSTEMI) was defined as elevated cardiac biomarkers without persistent ST-elevation.8 Left ventricular ejection fraction (LVEF) was measured by two-dimensional echocardiography using the biplane Simpson's method.9 And the estimated glomerular filtration rate (eGFR) was measured using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation.10 The morphology of the lesion was examined using coronary angiography and was classified using criteria established by ACC/AHA.11 Failed PCI was defined as Thrombolysis In Myocardial Infarction (TIMI) flow of grade 0 or I after the procedure.
Clinical follow-up was performed one year after the commencement of the study. Major adverse cardiac events (MACE) included cardiac death, myocardial infarction, percutaneous revascularization, and redo-CABG.
All analyses were performed using Statistical Package for the Social Sciences (SPSS) for Windows, version 21 (SPSS Inc, Chicago, IL, USA). Continuous variables are expressed as means±standard deviations and they were compared by unpaired Student's t-tests or Mann-Whitney rank-sum test. Discrete variables are presented as frequencies and percentages and were compared by chi-square test (or Fisher's exact). All statistical tests were 2-tailed with a statistical significance defined as p<0.05. Survival curves of one-year cardiac death, myocardial infarction, and MACE were calculated by Kaplan-Meier and log rank test was applied to compare the two groups. Furthermore, Cox regression analyses were performed using all available variables considered potentially relevant in determining the impact of different age groups on one-year MACE. Included variables were age (≥75 years), sex, smoking history, atrial fibrillation, previous IHD history, hypertension, diabetes mellitus, dyslipidemia, LV dysfunction (EF ≤40%), and renal insufficiency (estimated GFR <60 mL/min/1.73 m2), 3-vessel disease, LM lesion, and prescribed medications before discharge. In addition, multivariate logistic regression analyses were performed to identify the predictors of in-hospital mortality. Included variables were age, sex, BMI (≥25 kg/m2), smoking, shock (systolic blood pressure <90 mmHg) at arrival, atrial fibrillation, previous IHD history, hypertension, diabetes mellitus, dyslipidemia, LV dysfunction (EF ≤40%), and renal insufficiency (estimated GFR <60 mL/min/1.73 m2), use of a GP IIb/IIIa inhibitor, failed PCI, 3-vessel disease, LM lesion and Killip class ≥3. Multivariate analyses were performed using the variables showing p<0.1 in univariate analyses. The results are expressed as estimated hazard ratios with 95% confidence intervals (CIs) and p-values with clinical significance defined as p<0.05.
Lots of NSTEMI patients undergoing CABG were included between 60 to 79 years of age (n=306, 67.8%). Of the patients included in this study, the proportion of patients between 70 to 79 years old was largest (n=169, 37.4%), and the next was between 60 to 69 years old (n=137, 30.4%). Approximately, 27% of patients were elderly patients (≥75 years of age) (Fig. 1).
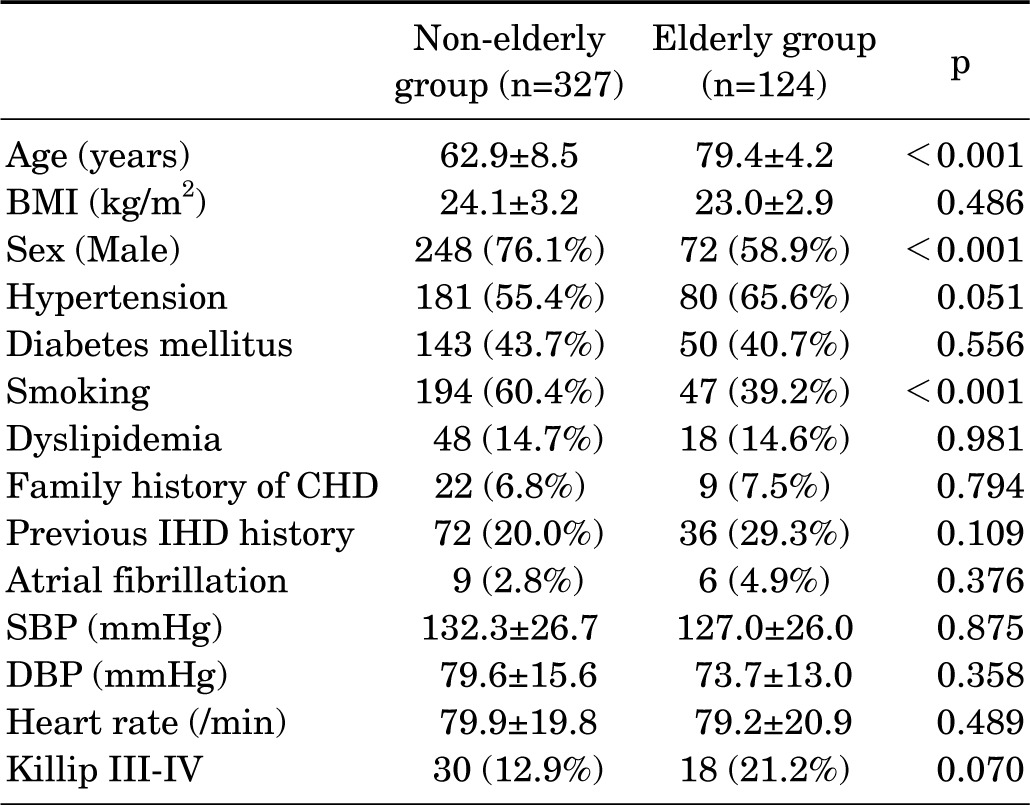
In comparing the clinical characteristics of the two groups, the elderly group had less male patients (76.1% vs.58.9%, p<0.001) and less smokers (60.4% vs. 39.2%, p<0.001). Furthermore, there were no significant differences in body mass index (BMI), histories of hypertension, diabetes mellitus, dyslipidemia, family history of coronary heart disease (CHD), history of ischemic heart disease (IHD), atrial fibrillation, systolic and diastolic blood pressure, heart rate, or proportion of Killip class III–IV (Table 1).
The LVEF measured by 2-dimentional echocardiogram was not significantly different between the two groups. However, Levels of serum creatine kinase (617.6±795.4 vs. 425.3±504.4, p=0.005) and triglyceride (132.6±75.2 vs. 105.4±64.2, p<0.001) were lower in the elderly group. There were no significant differences in the level of serum glucose, creatinine, creatine kinase-MB (CK-MB), troponin I, total cholesterol, high density lipoprotein-cholesterol(HDL-C), low density lipoprotein-cholesterol (LDL-C), high sensitivity C-reactive protein (Hs-CRP), N-terminal pro B-type natriuretic peptide (NT-proBNP), or hemoglobin A1c (HbA1c) between the groups (Table 2).
Three vessel disease was the most common in both non-elderly (57.3%) and elderly patients (60%) with NSTEMI who underwent CABG. The next most frequently involved vessels were left main in both groups. The most frequent target vessel was left anterior descending artery (LAD) and the most common morphology of the lesion was type C by ACC/AHA classification in both groups. The proportion of failed PCI was not significantly different between two groups (Table 2).
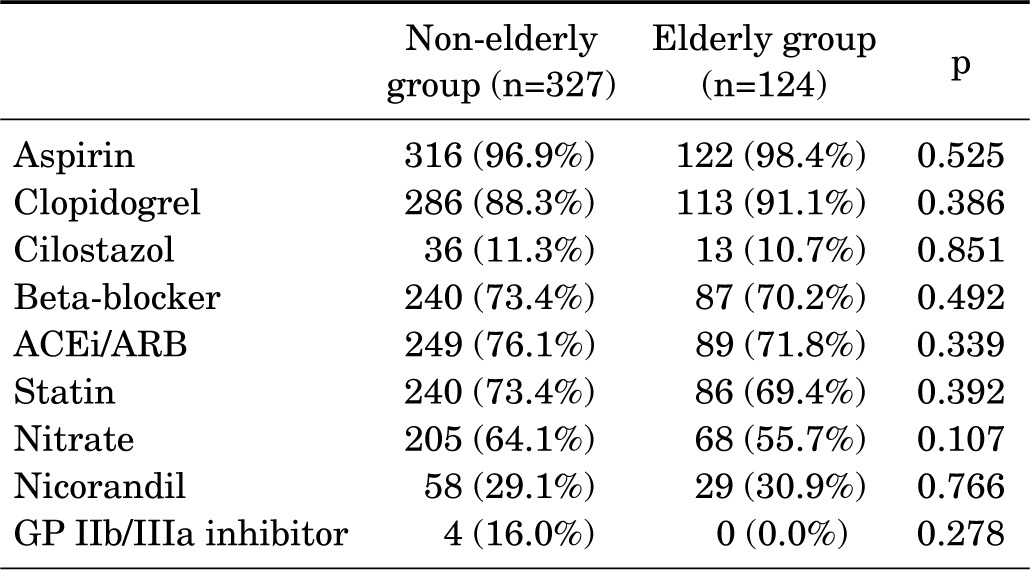
We compared the prescribed medications during admission. There were no significant differences in prescribed medications including aspirin, clopidogrel, cilostazol, beta-blockers, angiotensin converting enzyme inhibitor/angiotensin receptor blockers (ACEi/ARB), statin, nitrate, nicorandil, or the use of glycoprotein (GP) IIb/IIIa inhibitor (Table 3).
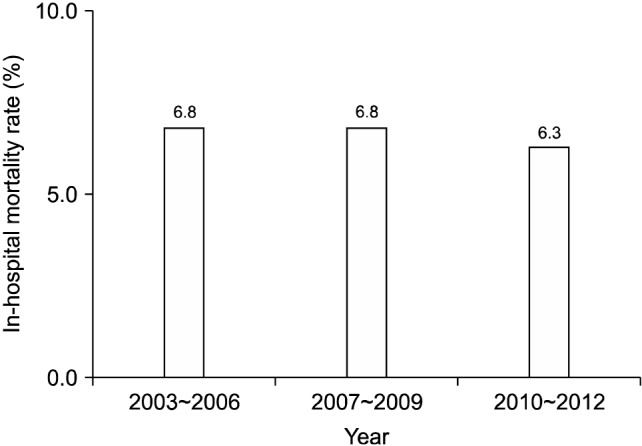
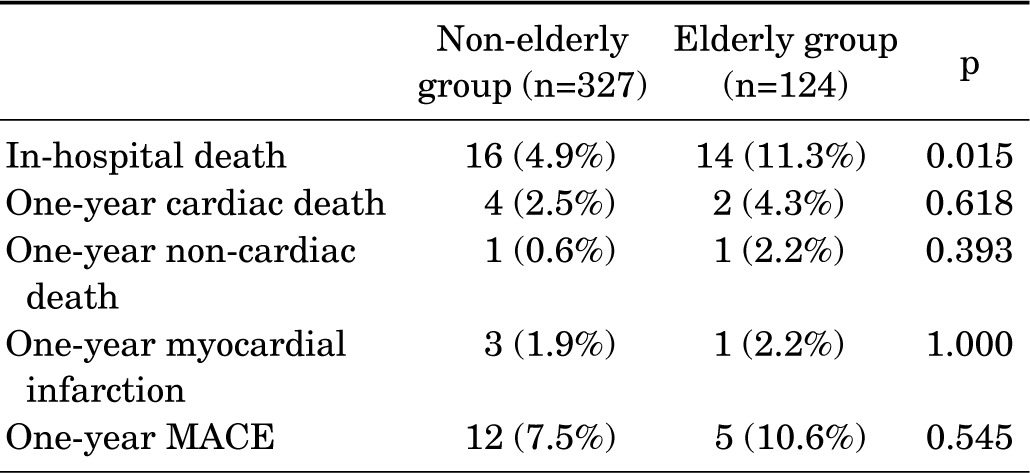
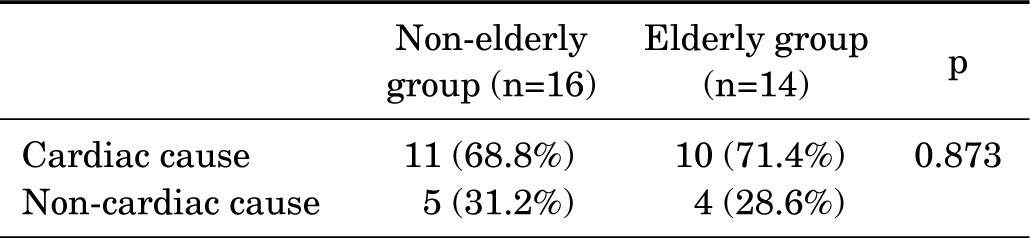
The average in-hospital mortality was 6.6%. The in-hospital mortality rate was 6.8% from 2003 to 2006, 6.8% from 2007 to 2009, and 6.3% from 2010 to 2012 respectively (Fig. 2). The in-hospital mortality was higher in the elderly group (4.9% vs. 11.3%, p=0.015) (Table 4). The causes of in-hospital mortality were not different between two groups. The rate of cardiac in-hospital mortality was 68.8% in the non-elderly group and 71.4% in the elderly group (Table 5). The most common cardiac cause of in-hospital mortality was low-output cardiac failure.
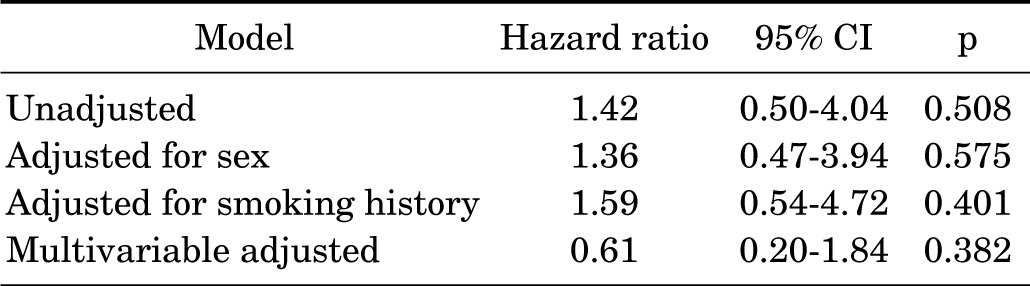
There were no significant differences in the cardiac death, non-cardiac death, myocardial infarction, or MACE at the one-year follow-up, unlike the in-hospital mortality (Table 4). On the basis of the Kaplan-Meier estimates, there were also no significant differences in the occurrence of cardiac death, myocardial infarction, and MACE between the two groups (Fig. 3). Furthermore, the unadjusted and adjusted MACE rates by Cox regression analyses were not different between the two group at the one-year follow-up (Table 6).
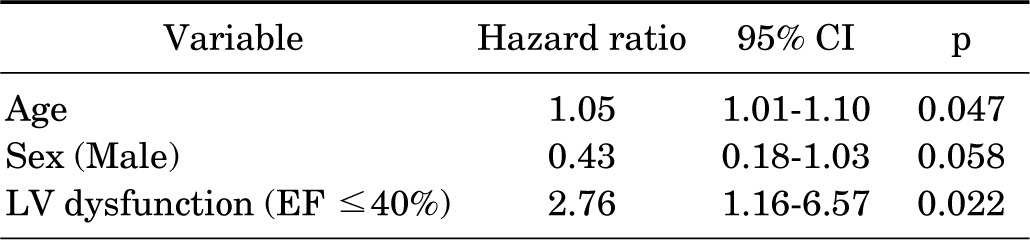
Multivariate logistic analysis was performed to identify the predictors of in-hospital mortality. Among the variables considered potentially relevant, age (HR 1.05, 95% CI 1.01–1.10, p=0.047) and LV dysfunction (EF ≤40%) (HR 2.76, 95% CI 1.16–6.57, p=0.022) were independent predictors of in-hospital mortality. In multivariate analysis, male sex showed a low hazard ratio of less than 1.0, but it was slightly insignificant (Table 7).
This study allows us to know the clinical outcomes and relevant factors for in-hospital mortality in Korean elderly NSTEMI patients undergoing CABG. Therefore, our results can be helpful to guide whether to perform cardiac surgery or to seek other therapeutic strategies. Our result showed that the elderly NSTEMI patients receiving CABG have higher in-hospital mortality, but one-year clinical outcomes were not different compared to non-elderly patients. Furthermore, this study found that left ventricular (LV) dysfunction (ejection fraction ≤40%) and older age was associated with higher in-hospital mortality.
Several studies mentioned the in-hospital mortality of elderly patients undergoing CABG. According to the some reports, the operative mortality rate among the elderly receiving CABG was 2.6% in a population >75 years of age and 11% in a population >80 years of age undergoing urgent or emergency surgery.1213 Other studies showed that in-hospital mortality in NSTEMI patients undergoing CABG is approximately 3.7%14 and operative mortality rates for CABG in patients ≥80 years of age with NSTEACS were between 5% and 8% (11% for urgent cases) and increased to approximately 13% at ≥90 years of age.1315 In our study, approximately 27% of patients were elderly patients, more than 75 years of age. In-hospital mortality of non-elderly patients was 4.9% and that of elderly patients was 11.3%. In-hospital mortality of the elderly was 2.3 times higher than non-elderly patients in our study.
However, one-year clinical outcomes including one-year cardiac death, myocardial infarction, and MACE were not significantly different in this study. Although in-hospital outcomes are poorer, the long term outcomes seem to be good for the elderly survivors of surgery. According to an analysis of nearly 25,000 patients >80 years of age who underwent CABG, in those who survived, the long-term survival rate was similar to that of the general population of octogenarians matched for age, sex and race.16 And Suguru et al. reported that age at operation does not affect long-term outcomes in patients undergoing off-pump CABG (OPCAB) with regard to cardiac death and cardiac events.17 Hillis et al.2 also reported that the majority of elderly patients achieve functional improvement after CABG, despite higher rates of in-hospital morbidity and mortality. According to the other studies, elderly patients ≥80 years of age who underwent CABG had improvements in quality of life, as assessed by the Seattle Angina Questionnaire.1819 In one of these, angina relief and quality of life improvement scores after CABG did not differ between the patients >75 and ≤75 years of age.13
A number of peri-operative factors have been demonstrated to influence the rate of operative mortality after CABG. In our study, the predictors of in-hospital mortality in NSTEMI patients after CABG were age and LV dysfunction (EF ≤40%). Old age was an independent risk factor for poor outcomes after CABG, as mentioned earlier. And the presence of LV dysfunction was one of the important independent predictors of operative mortality after CABG.2021 In a prospective observational study of over 8600 patients undergoing CABG, the operative mortality was less than 2% with a LVEF >40%, 3.5 to 4% with an LVEF between 20 and 40%, and approximately 8% with an LVEF <20%.21 LVEF must be considered in the decision to operate. A low LVEF, especially irreversible, can negate the benefits of surgery.
Although the p-value was not statistically significant, male sex showed a low hazard ratio for in-hospital mortality in this study (hazard ratio 0.43, 95% CI 0.18–1.03, p=0.058). There is controversy regarding the influence of sex on CABG outcomes. Previous studies examining sex differences in mortality after CABG have showed different results. Although most studies have showed higher in-hospital mortality in women compared with men, several studies documented that when an adjustment was made for differences in body size and clinical and angiographic variables, sex was not an accurate predictor.2223 In contrast, other studies have continued to show a higher mortality in women that persisted in multivariable analysis.242526 In a systemic review of sex differences and mortality after CABG, early mortality differences were reduced but not eliminated after adjustment for comorbidities, procedural characteristics, and body habitus.27 The impact of sex on in-hospital mortality should be clarified with a well-planned and controlled study.
This study had several limitations. First, the timing and method of CABG during admission were uncertain due to the absent data in this registry, but other baseline clinical characteristics were relatively similar between two groups. Second, the angina relief and quality of life after CABG is important, however, there was no information about the improvement of angina relief and the quality of life after surgery in this registry data. Third, there may be some bias in choosing elderly NSTEMI patients as candidates for CABG. Fourth, the sample size was relatively small. Therefore, a large-scale and longer-term study is needed including the information about the timing and manner of surgery and the improvement of symptoms.
In conclusion, the elderly patients have higher in-hospital mortality, but one-year outcomes were not different, compared to non-elderly NSTEMI patients receiving CABG. So elderly NSTEMI patients should be considered for CABG if surgery is more appropriate than PCI, but careful evaluation is required for the potential risks and benefits before surgery, especially if the elderly patients have severe LV systolic dysfunction.
ACKNOWLEDGEMENTS
This study was supported by grants of The Korean Society of Cardiology, The Korea Centers for Disease Control and Prevention (2013-E63005-01), and The Korean Health Technology R&D Project (HI13C1527), Ministry of Health & Welfare, Republic of Korea.
References
1. Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014; 130:e344–e426. PMID: 25249585.
2. Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, et al. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011; 58:e123–e210. PMID: 22070836.
3. Natarajan A, Samadian S, Clark S. Coronary artery bypass surgery in elderly people. Postgrad Med J. 2007; 83:154–158. PMID: 17344568.
4. Sim DS, Jeong MH, Cho KH, Ahn Y, Kim YJ, Chae SC, et al. Effect of early statin treatment in patients with cardiogenic shock complicating acute myocardial infarction. Korean Circ J. 2013; 43:100–109. PMID: 23508129.
5. Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, et al. ACC/AHA guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction--2002: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients With Unstable Angina). Circulation. 2002; 106:1893–1900. PMID: 12356647.
6. Alexander KP, Newby LK, Cannon CP, Armstrong PW, Gibler WB, Rich MW, et al. Acute coronary care in the elderly, part I: Non-ST-segment-elevation acute coronary syndromes: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation. 2007; 115:2549–2569. PMID: 17502590.
7. French JK, White HD. Clinical implications of the new definition of myocardial infarction. Heart. 2004; 90:99–106. PMID: 14676259.
8. Newby LK, Jesse RL, Babb JD, Christenson RH, De Fer TM, Diamond GA, et al. ACCF 2012 expert consensus document on practical clinical considerations in the interpretation of troponin elevations: a report of the American College of Cardiology Foundation task force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2012; 60:2427–2463. PMID: 23154053.
9. Quinones MA, Waggoner AD, Reduto LA, Nelson JG, Young JB, Winters WL Jr, et al. A new, simplified and accurate method for determining ejection fraction with two-dimensional echocardiography. Circulation. 1981; 64:744–753. PMID: 7273375.
10. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009; 150:604–612. PMID: 19414839.
11. Ellis SG, Vandormael MG, Cowley MJ, DiSciascio G, Deligonul U, Topol EJ, et al. Multivessel Angioplasty Prognosis Study Group. Coronary morphologic and clinical determinants of procedural outcome with angioplasty for multivessel coronary disease. Implications for patient selection. Circulation. 1990; 82:1193–1202. PMID: 2401060.
12. Ghanta RK, Shekar PS, McGurk S, Rosborough DM, Aranki SF. Nonelective cardiac surgery in the elderly: is it justified? J Thorac Cardiovasc Surg. 2010; 140:103–109. 109.e1PMID: 20005528.
13. Bardakci H, Cheema FH, Topkara VK, Dang NC, Martens TP, Mercando ML, et al. Discharge to home rates are significantly lower for octogenarians undergoing coronary artery bypass graft surgery. Ann Thorac Surg. 2007; 83:483–489. PMID: 17257973.
14. Parikh SV, de Lemos JA, Jessen ME, Brilakis ES, Ohman EM, Chen AY, et al. Timing of in-hospital coronary artery bypass graft surgery for non-ST-segment elevation myocardial infarction patients results from the National Cardiovascular Data Registry ACTION Registry-GWTG (Acute Coronary Treatment and Intervention Outcomes Network Registry-Get With The Guidelines). JACC Cardiovasc Interv. 2010; 3:419–427. PMID: 20398870.
15. Krane M, Voss B, Hiebinger A, Deutsch MA, Wottke M, Hapfelmeier A, et al. Twenty years of cardiac surgery in patients aged 80 years and older: risks and benefits. Ann Thorac Surg. 2011; 91:506–513. PMID: 21256302.
16. Peterson ED, Cowper PA, Jollis JG, Bebchuk JD, DeLong ER, Muhlbaier LH, et al. Outcomes of coronary artery bypass graft surgery in 24,461 patients aged 80 years or older. Circulation. 1995; 92(9 Suppl):II85–II91. PMID: 7586468.
17. Ohira S, Doi K, Numata S, Yamazaki S, Yamamoto T, Fukuishi M, et al. Does age at operation influence the short- and long-term outcomes of off-pump coronary artery bypass grafting? Circ J. 2015; 79:2177–2185. PMID: 26227150.
18. Conaway DG, House J, Bandt K, Hayden L, Borkon AM, Spertus JA. The elderly: health status benefits and recovery of function one year after coronary artery bypass surgery. J Am Coll Cardiol. 2003; 42:1421–1426. PMID: 14563586.
19. Huber CH, Goeber V, Berdat P, Carrel T, Eckstein F. Benefits of cardiac surgery in octogenarians--a postoperative quality of life assessment. Eur J Cardiothorac Surg. 2007; 31:1099–1105. PMID: 17369044.
20. Fortescue EB, Kahn K, Bates DW. Development and validation of a clinical prediction rule for major adverse outcomes in coronary bypass grafting. Am J Cardiol. 2001; 88:1251–1258. PMID: 11728352.
21. Yau TM, Fedak PW, Weisel RD, Teng C, Ivanov J. Predictors of operative risk for coronary bypass operations in patients with left ventricular dysfunction. J Thorac Cardiovasc Surg. 1999; 118:1006–1013. PMID: 10595971.
22. Aldea GS, Gaudiani JM, Shapira OM, Jacobs AK, Weinberg J, Cupples AL, et al. Effect of gender on postoperative outcomes and hospital stays after coronary artery bypass grafting. Ann Thorac Surg. 1999; 67:1097–1103. PMID: 10320257.
23. O'Connor GT, Morton JR, Diehl MJ, Olmstead EM, Coffin LH, Levy DG, et al. The Northern New England Cardiovascular Disease Study Group. Differences between men and women in hospital mortality associated with coronary artery bypass graft surgery. Circulation. 1993; 88:2104–2110. PMID: 8222104.
24. Brandrup-Wognsen G, Berggren H, Hartford M, Hjalmarson A, Karlsson T, Herlitz J. Female sex is associated with increased mortality and morbidity early, but not late, after coronary artery bypass grafting. Eur Heart J. 1996; 17:1426–1431. PMID: 8880029.
25. O'Rourke DJ, Malenka DJ, Olmstead EM, Quinton HB, Sanders JH Jr, Lahey SJ, et al. Northern New England Cardiovascular Disease Study Group. Improved in-hospital mortality in women undergoing coronary artery bypass grafting. Ann Thorac Surg. 2001; 71:507–511. PMID: 11235698.
26. Vaccarino V, Abramson JL, Veledar E, Weintraub WS. Sex differences in hospital mortality after coronary artery bypass surgery: evidence for a higher mortality in younger women. Circulation. 2002; 105:1176–1181. PMID: 11889010.
27. Kim C, Redberg RF, Pavlic T, Eagle KA. A systematic review of gender differences in mortality after coronary artery bypass graft surgery and percutaneous coronary interventions. Clin Cardiol. 2007; 30:491–495. PMID: 17880013.
FIG. 1
Graph of age distribution in Non ST-segment elevation myocardial infarction (NSTEMI) patients undergoing coronary artery bypass surgery (CABG).
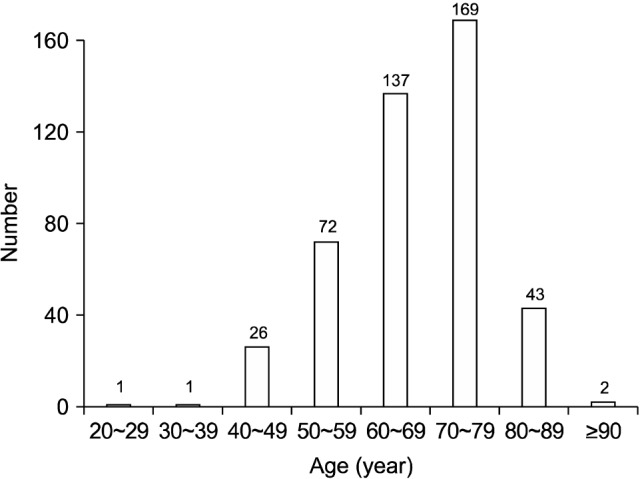
FIG. 3
Kaplan-Meier estimates of the incidences of (A) cardiac death, (B) myocardial infarction, (C) major adverse cardiac event (MACE) between non-elderly and elderly groups at one-year follow up.
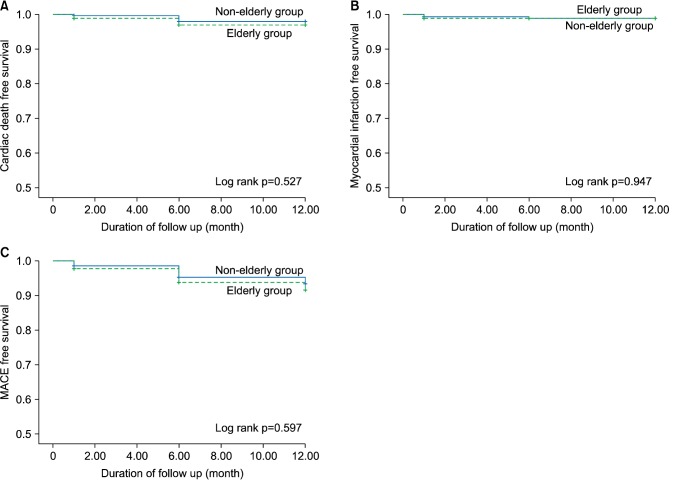
TABLE 2
Baseline echocardiographic, laboratory, and coronary angiographic findings
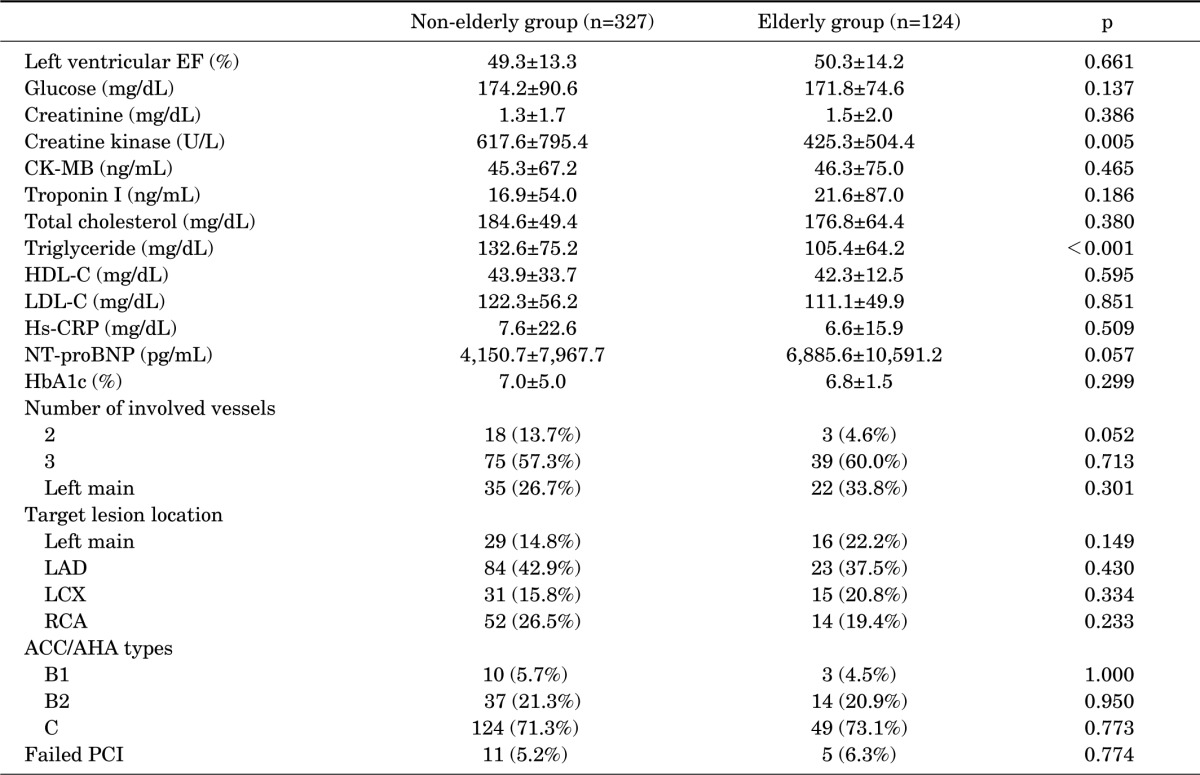
Values are presented as mean±standard deviation or number (%). EF: ejection fraction, CK-MB: creatine kinase-MB, HDL-C: high density lipoprotein-cholesterol, LDL-C: low density lipoprotein-cholesterol, Hs-CRP: high sensitivity C-reactive protein, NT-proBNP: N-terminal pro B-type natriuretic peptide, HbA1c: hemoglobin A1c, LAD: left anterior descending artery, LCX: left circumflex artery, RCA: right coronary artery, ACC/AHA: American College of Cardiology/American Heart Association, PCI: percutaneous coronary intervention.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download