Abstract
Salmonella enterica serovar Typhimurium is one of the most important bacterial pathogens causing diarrhea. The resistance of S. typhimurium to antimicrobial agents, which has recently been isolated from patients, is causing serious problems. We investigated the effects of salicylic acid (Sal) and acetyl salicylate (AcSal) on the susceptibility of S. typhimurium to cephalosporin antibiotics, which are known to increase resistance to cephalosporin and quinolone antibiotics. The MIC of cephalosporin antibiotics was higher than that of the media without Sal. The rate of accumulation of ethidium bromide (EtBr) in the bacteria by the outer membrane protein (Omp) was not different from that of the bacteria cultured in the medium containing Sal. However, Carbonyl cyanide-m-chlorophenylhydrazone (CCCP), an inhibitor of bacterial efflux pumps, significantly reduced the rate of accumulation of EtBr in bacteria cultured on Sal containing medium. In the medium containing CCCP, the MIC of the antimicrobial agent tended to decrease as compared with the control. In addition, the MIC of the bacteria treated with CCCP and Sal was higher than that of the antimicrobial agent against the CCCP treated experimental bacteria. These results suggest that Sal decreases the expression of OmpF in the Omp of S. typhimurium and reduces the permeability of cephalosporin antibiotics to bacteria, which may induce tolerance to cephalosporin antibiotics.
Antibiotics are powerful medicines that fight certain infections and can save lives when used properly. Antibiotics either stop bacteria from reproducing or destroy them. This benefit of antibiotics comes with the risk of induced antibiotic resistance.1 Antibiotic resistance of gram-negative bacteria occurs through spontaneous mutation or the acquisition of gene(s) encoding enzymes that degrade antibiotics, increase mutation rates against stress responses and alteration of the active sites of antibiotics.2 The mechanism of resistance to cephalosporin in gram negative bacteria is the hydrolysis of antibiotics by beta-lactamases and the removal of antibiotics by modified cell wall permeability or efflux mechanisms.3456
Sal is biosynthesized from the amino acid phenylalanine. It can be prepared by the hydrolysis of AcSal or methyl Sal.7 Sal is one of the drug groups that are used as a non-steroidal anti-inflammatory agent.78 Sal, as a medicine, is used as an antipyretic, an analgesic and an anti-inflammatory agent. It has been shown to inhibit the coagulation of blood, and low doses are used to prevent cardiac infarction, stroke and thrombosis.78 Sal is known to act not only on the human body but also on bacteria, leading to morphological and physiological changes of bacteria. In particular, it may lead to an increase in expression of bacterial virulence factors or an increase in tolerance to various types of antimicrobial agents.9101112
In order for the antimicrobial effect of cephalosporin antibiotic to function against gram-negative bacteria such as Escherichia coli (E. coli) and Salmonella enterica, it is necessary to pass through porin protein in the Omp of bacteria to participate in the synthesis of peptidoglycan in bacteria. The resistance to cephalosporin antibiotics in gram-negative bacteria such as Salmonella enterica is mainly due to the hydrolysis of antimicrobial agents by β-lactamase, which is mainly in the space around the cytoplasmic membrane.23456 Sal treatment of E. coli induces increased expression of MarA and MarR, resulting in increased expression of AcrAB-TolC efflux pumps and decreased expression of OmpF, leading to increased resistance to quinolone antibiotics, tetracycline, and chloramphenicol.1131415
S. typhimurium also has the same marRAB gene as E. coli and has been reported to increase resistance to chloramphenicol and enoxacin when cultured in a medium containing Sal.16 In addition, Hartog et al.12 reported that Sal treatment of S. typhimurium resulted in an increased expression of MarA, leading to the expression of acrAB gene, thereby increasing the active excretion of antibiotics outside the cells and inducing resistance to ciprofloxacin.
In this study, we investigate the effect of Sal and AcSal on the susceptibility of S. typhimurium to cephalosporin antibiotics widely used for gram-negative bacterial infections. In particular, we investigated the effect of Sal and AcSal on the efficacy of antimicrobial agents released by the efflux pump controlled by MarA and the induction of tolerance by decreasing the antimicrobial permeability to bacteria through the pore protein OmpF.
S. typhimurium SCH2005 were isolated at Chonnam National University Hospital, Gwangju, Korea. S. typhimurium 14028S (ATCC, VA, USA) were cultured in Difco Mueller-Hinton agar (MHA) or broth Becton Dickinson and Co. (Franklin Lakes, NJ).
The media-dilution test was used to determine MIC values against antibiotics in the presence of Sal.13 MHB with or without 5 mM Sal or AcSal was serially diluted with cephalosporin antibiotics and then, S. typhimurium (105–106colony forming units (CFU)/ml) were inoculated. Bacterias were cultured for 24 h at 37℃. The concentration ranges of the antibiotics were selected according to the National Committee for Clinical Laboratory Standards (NCCLS) guidelines.1415 The bacterial numbers were determined by measuring the optical density at 600 nm (OD600) and comparing the results with a standard curve. Efflux of antibiotics and Sal out of bacteria was assessed by the disc diffusion method and MIC measurements in the presence of cyanide m-chlorophenyl hydrazone (CCCP), an efflux pump inhibitor (Sigma-Adrich, CA, USA).
Extraction of S.typhimurium Omp and analysis were performed as described previously1617 with modification. Briefly, bacteria were cultured in MHB with 5 mM Sal or AcSal for 24 h at 37℃. The cultured bacteria were centrifuged at 3,000×g for 10 min and the cell pellets were washed three times with phosphate-buffered saline (PBS). The final pellets were resuspended in 62.5 mM Tris-HCl buffer (pH 6.8), crushed twice using a French press operating at 15,000 lbs/in2 and centrifuged at 3,000×g for 10 min. Cell debris were removed and each supernatant was centrifuged at 12,000×g at 10℃. To separate the various Omps, the pellets were resuspended in 2% N-lauryl sarcocinate (Sigma-Aldrich) in 10 mM phosphate buffer (pH 7.0) for 20 min, and then centrifuged at 100,000×g for 40 min. The Omp pellets were resuspended in 10 mM phosphate buffer. Protein concentrations were determined by the Bradford method2 and protein samples were separated by SDS-polyacrylamide gel electrophoresis (SDS-PAGE) followed by Coomassie blue staining.
EtBr accumulation in bacterial cells was measured by a previously detailed fluorometric method.18 S. typhimurium was cultured in MHB containing 5 mM Sal or AcSal to a log-phase of growth, centrifuged and resuspended in 10 mM phosphate buffer (pH 7.0). Bacteria (OD600 of 0.2) were inoculated into a culture medium containing 2 µg/ml EtBr and cultured. EtBr accumulation in bacteria was measured at an emission and excitation wavelength of 530 nm and 600 nm, respectively, using a SPECTRA max GEMINI fluorometer (Molecular Devices, CA, USA).
The preparation of complementary DNA (cDNA) and Q-RT-PCR was done as per the manufacturer's instructions. Briefly, total RNA was extracted from cultures using a Qiagen RNeasy Mini Kit (QIAGEN, CA, USA). Five micrograms of total RNA was reverse transcribed using superscript III reverse transcriptase (Invitrogen, CA, USA) and random hexamers to generate cDNA. RT-PCR for quantification of the specific mRNA molecules (ompA, ompC, ompF, acrA, acrD, tolC and micF) was performed with a LightCycler-R 96 System (Roche Diagnostics, Mannheim, Germany). The primers used are described in Table 1. Threshold cycle (Ct) values were determined from triplicate reactions for the test and reference samples of each target and the internal control gene (rfaH). Concentrations of the experimental transcripts were calculated from the linear expression of a standard curve of a PCR product and normalized by rfaH mRNA calculated concentrations. For each sample, the normalized concentration of the untreated sample was set at 1 and the other normalized concentrations were calculated proportionally.
In order to observe the increase in resistance to cephalosporin by Sal, MIC was measured in MHB containing Sal. The MIC of cephalothin in MHB without Sal was 100 µg/ml, but the MIC in MHB with 5 mM Sal or AcSal was 200 µg/ml, a more than 2-fold increase. The MIC of cefmetazole increased 8–16 times from 1.6 µg/ml to 12.5–25 µg/ml, and the MIC of cefotaxime increased more than 8-fold from 3.2 µg/ml to 25 µg/ml (Table 2).
In the presence of CCCP, the MIC in bacteria treated with cephalosporins such as cephalothin, cefmetazole and cefotaxime, was significantly decreased versus the control bacteria (Table 3). This suggested that CCCP inhibition promotes accumulation of the tested antibiotics, increasing the susceptibility of S. typhimurium. In the presence of both CCCP and Sal/AcSal, the cephalosporin MIC increased 2-8-fold compared to bacteria treated only with CCCP. This indicated that Sal or AcSal repress accumulation of the antibiotics by CCCP, thereby decreasing susceptibility to these antibiotics. This increase in MIC was also observed at comparable levels for bacteria treated only with Sal or AcSal (Table 2, 3).
EtBr is a useful fluorometric probe to measure the membrane permeability activity in bacteria.19 In order to investigate whether Sal is involved mainly in the reduction of antimicrobial permeability into the cell or the increase of the active excretion outside the cell, which is the cause of the increased resistance to cephalosporin antimicrobial agents, accumulation of EtBr in the cells was performed. The bacteria was treated in a medium of 5 mM Sal or AcSal. EtBr accumulation rates were unchanged during the culture, indicating that Sal or AcSal did not affect the bacterial efflux pump activity (Fig. 1). However, when the AcrAB efflux pump inhibitor, CCCP was treated at 100 µM, the fluorescence intensity of EtBr increased rapidly in the control group but gradually increased in the experimental group treated with 5 mM of Sal or AcSal (Fig. 1). Interestingly, the accumulation of EtBr in bacteria tended to decrease dose-dependence during Sal or AcSal treatment (Fig. 2). After 5 minutes of measuring the EtBr fluorescence intensity in the cells, CCCP was added to block the active efflux pump of bacteria. Sal-treated bacteria showed a gradual increase in the fluorescence intensity of EtBr as compared to the control group (Fig. 3), indicating that the permeability of EtBr into bacteria was decreased in the Sal-treated bacteria compared to the control.
Antibiotics enter bacteria via various Omp proteins that act as porins.1120 Sal reportedly decreases OmpF levels.121 S. typhimurium was cultured in MHB with or without 5 mM of Sal for 24 h, the membrane proteins of the bacteria were separated and electrophoresed. Then, the expressions of three proteins, OmpA, OmpF and OmpC, were examined. These three proteins are proteins that form porin, which is used as a transport channel for various substances such as antimicrobial agents. OmpA, OmpC and F were detected at 34 kD, 36 kD and 35 kD, respectively, (Fig. 4) as expected.122223 In normal bacteria, 35 kD of OmpF was expressed most strongly among the three proteins, but OmpF expression was decreased and OmpC expression was relatively increased in bacteria grown on a Sal containing medium.
Next, we measured the expression levels of ompA, ompC and ompF, and mRNA expressions by the efflux genes acrA, acrD and tolC by Q-RT-PCR. Sal treatment reduced ompF mRNA levels 20-fold compared to the untreated control. However, no significant change was noted for ompA and ompC (Fig. 5). These changes in mRNA levels of Omp protein genes were similar to the protein levels. micF, which is an antisense RNA regulator of ompF, was increased 12.7-fold after Sal treatment as compared to the control. This may account, at least in part, for the decrease in OmpF by Sal. However, levels of acrA, acrD and tolC did not significantly change with Sal treatment.
Salmonella is a gram-negative condition anaerobic intracellular parasitic bacterium that was first isolated by Salmon and Smith in 1886 and is the most common pathogenic bacterium causing gastroenteritis, septicemia, and intestinal inflammation. More than 2,300 serotypes are known, Enteritidis and Typhimurium are frequently reported as the most frequently detected.2425 Recently, resistance to antimicrobial agents observed in Salmonella isolated from patients has caused serious problems worldwide. In the United States in the 1980s, the isolation rate of strains resistant to one or more antimicrobial agents was 16%, but increased to 31% in the 1990s. In Korea, the resistance rate to antimicrobial agents is high, the rate of resistance to the disease has been reported to be very high.27
In general, resistance to antimicrobial agents occurs when a bacterium that was originally susceptible is mutated or acquires resistance genes from other bacteria.28 Bacteria that are susceptible to antimicrobial agents may also have tolerance to non-genetic origin, depending on their growth conditions. In particular, bacteria cultured in a medium containing Sal have been reported to induce non-hereditary resistance to various antimicrobial agents. 79101112 In this study, the MIC of 5 mM Sal or AcSal was found to be more than 2 times higher than cephalothin, 8–16 times higher than cefmetazole, and 8 times higher than that of cefotaxime, so that Sal was more effective than cephalosporin Based antimicrobial agents (Table 2).
The cause of low susceptibility to cephalosporin antimicrobials in gram-negative bacteria such as Salmonella is attributed to reduced permeability and active efflux by overproduction of the AcrAB efflux pump.3456 Sal-induced antimicrobial resistance is known to be due to changes in the protein synthesis of cell membranes associated with the accumulation of antimicrobial agents in the cytoplasm of bacteria.293031 It is known that E. coli grown in a medium containing Sal is resistant to quinolone antibiotics, tetracycline, chloramphenicol, ampicillin and cephalosporin due to increased expression of AcrAB-TolC efflux pump and decreased expression of OmpF.233132
S. typhimurium also has the same marRAB gene as E. coli and increased resistance to chloramphenicol and enoxacin when cultured in Sal-containing media.32 In addition, Hartog et al.12 reported that when Sal was administered, acrAB induction by increased expression of MarA resulted in increased efflux of antimicrobial agents outside the cells, leading to tolerance to ciprofloxacin.
In order to investigate the effect of Sal on the antimicrobial activity, we investigated whether Sal is involved in the pathogenesis of bacterial resistance to cephalosporin. EtBr accumulation experiments were carried out. When CCCP, an inhibitor of the AcrAB efflux pump, was treated with 100 µM, the fluorescence intensity of ethidium bromide in normal bacteria tended to be significantly higher than that of the experimental strain treated with 5 mM of Sal or AcSal. In particular, the accumulation of EtBr in bacteria tended to decrease dose-dependently during Sal treatment, suggesting that the permeability of ethidium bromide into bacteria was decreased in Sal-treated strains. This result is different from the report that Sal treatment of S. typhimurium induced acrAB induction by increasing expression of MarA, resulting in an increase in the active excretion of the antimicrobial agent out of the cell and resistance to ciprofloxacin.12
The permeation of Cephalosporin and quinolone antibiotics into the cells occurs through an outer membrane protein called porin, which forms hydrophilic pores in the outer membrane. There are three types of porosity in E. coli: OmpA, OmpC, and OmpF. In particular, the decrease in the permeability of cephalosporin and quinolone antibiotics has been reported to be due to the decreased expression of OmpF, which forms larger pores in the three porins.16 It has been reported that OmpF expression is reduced to reduce the absorption of these substances when exposed to toxins, and Sal has been shown to reduce the expression of OmpF in E. coli and Serratia marcescens.213334 In this study, the expression of OmpF was significantly decreased in the culture medium supplemented with 5 mM of Sal, indicating that induction of resistance to cephalosporin antibiotics was caused by a decrease in permeability into bacteria. In addition, the bacterial accumulation of ethidium bromide did not change. However, after 5 minutes, CCCP was added to block the active emission of bacteria. As a result, the rate of accumulation of ethidium bromide in Sal-treated bacteria was significantly lower than that of normal control, Was found to be correlated with the decrease in permeability of ethidium bromide into bacteria. As a result of measuring the MIC of cephalosporin antibiotics by treating CCCP, an inhibitor of AcrAB efflux pump, the MIC of the test strains in the medium containing CCCP was 2–8 times lower than that of the normal control. However, when Sal and CCCP were treated simultaneously, it was 2–8 times higher than the MIC for the CCCP-treated test bacteria. It was found that Sal treatment reduced the permeability of cephalosporin into the cells of experimental strains and induces resistance.
In S. typhimurium, there is a report that Sal treatment increases the expression of MarA, inducing the expression of acrAB gene and discharging the antimicrobial agent out of the cells to induce tolerance to ciprofloxacin.12 However, in this experiment, the inhibitor of the AcrAB efflux pump, CCCP Were treated with 100 µM of Sal, the rate of accumulation of ethidium bromide was significantly lower than that of normal bacteria, and the MIC of strains treated with CCCP and Sal was lower than that of strains treated only with CCCP The increase of 2–8 fold, which is different from quinolone antimicrobial resistance induction, is considered to be the most important factor to induce tolerance of cephalosporin antibiotics. In order to prove this conclusion, real-time PCR or microarray will be performed to confirm the increase or decrease of expression of each gene during Sal treatment.
These results suggest that careful consideration should be given to the combination of Sal and cephalosprin antibiotics. To maintain plasma levels of 150 µg/ml (1.1 mM) in patients with rheumatoid arthritis, such as large doses of aspirin, the highest plasma concentration is expected to be 1–2 mM, It is the concentration that can cause enough. In addition, in order to maintain this plasma concentration, doses of 60 mg/kg/day may be effective in inducing resistance to intestinal bacteria in the intestinal tract and sufficient antimicrobial resistance.
Figures and Tables
FIG. 1
Accumulation of EtBr in S. typhimurium by treated with Sal (5 mM) or AcSal (5 mM), and CCCP (100 µM) was added at the same time with ethidium bromide. EtBr accumulation in bacteria was measured as bacterial fluorescence intensity.
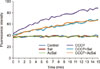
FIG. 2
Effect of Sal on EtBr accumulation in S. typhimurium. (A and C) EtBr accumulation in bacteria treated with 5 mM Sal (A) or AcSal (C). (B and D) EtBr accumulation in bacteria treated with indicated concentrations of Sal (B) or AcSal (D) in the presence of 100 µM CCCP.
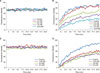
FIG. 3
Effects of Sal on EtBr accumulation are increased by CCCP in S. typhimurium. Bacteria were left untreated (control) or treated with 5 mM Sal or AcSal. CCCP (100 µM) was added at the indicated time (arrow) and further cultured.
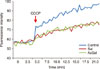
FIG. 4
The change in Omp protein levels by Sal in S. typhimurium. Omp proteins were isolated from bacteria cultured overnight in the absence (control) or presence (Sal) of 5 mM Sal. Same amounts of proteins were separated in SDS-PAGE and stained with Coomassie blue. M: protein standards.

FIG. 5
Effects of Sal on the expression of outer membrane protein genes and active efflux pump genes, quantified by real-time RT-PCR. Bacteria were cultured overnight in the absence or presence of 5 mM Sal and the amounts of the transcripts were measured using Q-RT-PCR analysis against their RNAs. The experiment was carried out triplicate.

References
1. Cohen SP, McMurry LM, Hooper DC, Wolfson JS, Levy SB. Cross-resistance to fluoroquinolones in multiple-antibiotic- resistant (Mar) Escherichia coli selected by tetracycline or chloramphenicol: decreased drug accumulation associated with membrane changes in addition to OmpF reduction. Antimicrob Agents Chemother. 1989; 33:1318–1325.

2. Arlet G, Barrett TJ, Butaye P, Cloeckaert A, Mulvey MR, White DG. Salmonella resistant to extended-spectrum cephalosporins: prevalence and epidemiology. Microbes Infect. 2006; 8:1945–1954.

3. Baucheron S, Tyler S, Boyd D, Mulvey MR, Chaslus-Dancla E, Cloeckaert A. AcrAB-TolC directs efflux-mediated multidrug resistance in Salmonella enterica serovar typhimurium DT104. Antimicrob Agents Chemother. 2004; 48:3729–3735.

4. Eaves DJ, Ricci V, Piddock LJ. Expression of acrB, acrF, acrD, marA, and soxS in Salmonella enterica serovar Typhimurium: role in multiple antibiotic resistance. Antimicrob Agents Chemother. 2004; 48:1145–1150.

5. Medeiros AA, O'Brien TF, Rosenberg EY, Nikaido H. Loss of OmpC porin in a strain of Salmonella typhimurium causes increased resistance to cephalosporins during therapy. J Infect Dis. 1987; 156:751–757.

6. Miró E, Vergés C, García I, Mirelis B, Navarro F, Coll P, et al. Resistance to quinolones and beta-lactams in Salmonella enterica due to mutations in topoisomerase-encoding genes, altered cell permeability and expression of an active efflux system. Enferm Infecc Microbiol Clin. 2004; 22:204–211.

7. Price CT, Lee IR, Gustafson JE. The effects of salicylate on bacteria. Int J Biochem Cell Biol. 2000; 32:1029–1043.

8. Vane JR, Flower RJ, Botting RM. History of aspirin and its mechanism of action. Stroke. 1990; 21:12 Suppl. IV12–IV23.
9. Coban AY, Birinci A, Ekinci B, Durupinar B. Effects of acetyl salicylate and ibuprofen on fluoroquinolone MICs on Salmonella enterica serovar typhimurium in vitro. J Chemother. 2004; 16:128–133.

10. Riordan JT, Muthaiyan A, Van Voorhies W, Price CT, Graham JE, Wilkinson BJ, et al. Response of Staphylococcus aureus to salicylate challenge. J Bacteriol. 2007; 189:220–227.

11. Randall LP, Woodward MJ. Role of the mar locus in virulence of Salmonella enterica serovar Typhimurium DT104 in chickens. J Med Microbiol. 2001; 50:770–779.

12. Hartog E, Menashe O, Kler E, Yaron S. Salicylate reduces the antimicrobial activity of ciprofloxacin against extracellular Salmonella enterica serovar Typhimurium, but not against Salmonella in macrophages. J Antimicrob Chemother. 2010; 65:888–896.

13. Stalons DR, Thornsberry C. Broth-dilution method for determining the antibiotic susceptibility of anaerobic bacteria. Antimicrob Agents Chemother. 1975; 7:15–21.

14. Cockerill FR, Wikler MA, Alder J, Dudley MN, Eliopoulos GM, Ferraro MJ, et al. Performance standards for antimicrobial disk susceptibility tests; approved standard. 11th ed. Wayne, PA: :Clinical and Laboratory Standards Institute;2012.
15. Kiehlbauch JA, Hannett GE, Salfinger M, Archinal W, Monserrat C, Carlyn C. Use of the National Committee for Clinical Laboratory Standards guidelines for disk diffusion susceptibility testing in New York state laboratories. J Clin Microbiol. 2000; 38:3341–3348.

16. Aoyama H, Sato K, Kato T, Hirai K, Mitsuhashi S. Norfloxacin resistance in a clinical isolate of Escherichia coli. Antimicrob Agents Chemother. 1987; 31:1640–1641.

17. Martinez MB, Flickinger M, Higgins L, Krick T, Nelsestuen GL. Reduced outer membrane permeability of Escherichia coli O157:H7: suggested role of modified outer membrane porins and theoretical function in resistance to antimicrobial agents. Biochemistry. 2001; 40:11965–11974.

18. Baranova NN, Neyfakh AA. Apparent involvement of a multidrug transporter in the fluoroquinolone resistance of Streptococcus pneumoniae. Antimicrob Agents Chemother. 1997; 41:1396–1398.

19. Paixão L, Rodrigues L, Couto I, Martins M, Fernandes P, de Carvalho CC, et al. Fluorometric determination of ethidium bromide efflux kinetics in Escherichia coli. J Biol Eng. 2009; 3:18.

20. Cohen SP, McMurry LM, Levy SB. marA locus causes decreased expression of OmpF porin in multiple-antibiotic-resistant (Mar) mutants of Escherichia coli. J Bacteriol. 1988; 170:5416–5422.

21. Cohen SP, Levy SB, Foulds J, Rosner JL. Salicylate induction of antibiotic resistance in Escherichia coli: activation of the mar operon and a mar-independent pathway. J Bacteriol. 1993; 175:7856–7862.

22. Hutsul JA, Worobec E. Molecular characterization of the Serratia marcescens OmpF porin, and analysis of S. marcescens OmpF and OmpC osmoregulation. Microbiology. 1997; 143:2797–2806.

23. Rosner JL, Chai TJ, Foulds J. Regulation of ompF porin expression by salicylate in Escherichia coli. J Bacteriol. 1991; 173:5631–5638.

24. Rodrigue DC, Tauxe RV, Rowe B. International increase in Salmonella enteritidis: a new pandemic? Epidemiol Infect. 1990; 105:21–27.

25. Chalker RB, Blaser MJ. A review of human salmonellosis: III. Magnitude of Salmonella infection in the United States. Rev Infect Dis. 1988; 10:111–124.

26. Lee LA, Puhr ND, Maloney EK, Bean NH, Tauxe RV. Increase in antimicrobial-resistant Salmonella infections in the United States, 1989–1990. J Infect Dis. 1994; 170:128–134.

27. Yang SJ, Park KY, Kim SH, No KM, Besser TE, Yoo HS, et al. Antimicrobial resistance in Salmonella enterica serovars Enteritidis and Typhimurium isolated from animals in Korea: comparison of phenotypic and genotypic resistance characterization. Vet Microbiol. 2002; 86:295–301.

29. Nikaido H. Outer membrane barrier as a mechanism of antimicrobial resistance. Antimicrob Agents Chemother. 1989; 33:1831–1836.

30. Osborn MJ, Wu HC. Proteins of the outer membrane of gram-negative bacteria. Annu Rev Microbiol. 1980; 34:369–422.

31. Sawai T, Hirano S, Yamaguchi A. Repression of porin synthesis by salicylate in Escherichia coli, Klebsiella pneumoniae and Serratia marcescens. FEMS Microbiol Lett. 1987; 40:233–237.

32. Sulavik MC, Dazer M, Miller PF. The Salmonella typhimurium mar locus: molecular and genetic analyses and assessment of its role in virulence. J Bacteriol. 1997; 179:1857–1866.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download