Abstract
Background
The purpose of this study was to determine the impact of an educational intervention that includes information sharing about absolute fracture risk on the knowledge of osteoporosis and modifiable risk factors among Korean patients with osteoporosis.
Methods
Adults aged >50 years who visited the outpatient clinic for osteoporosis were recruited. Subjects with trauma-related fractures or pathological fractures were excluded. The anthropometric data and clinical risk factors for fracture were collected at baseline. The participants completed the survey questionnaire that measured their knowledge regarding osteoporosis at baseline and then received information about the risk of fracture and individual education. Fracture risk was classified into five groups according to degree. The post-survey was conducted 3 months later. The pretest results were compared with the posttest results.
Results
In this study, 179 subjects (15 men and 164 women) were enrolled. After the educational intervention, the mean osteoporosis knowledge score significantly increased from 10.6±5.7 at pre-education (baseline) to 11.7±6.3 at post-education (P<0.001). When comparing the pre- and post-education Korean fracture risk scores, a negligible difference was found between the “very low risk” and “low risk” groups. However, the scores in the “very high risk” and “high risk” groups decreased from 77.6% to 76.0%. We found a difference over time only in physical activity.
Osteoporosis is generally known as a silent disease. However, if an osteoporotic fracture occurs as a complication, it causes serious problem such as chronic pain and disability, loss of independence, decreased the quality of life, and increased mortality.[1] Therefore, for chronic conditions like osteoporosis, the health care system needs to focus on improving awareness of the disease through education. Educational intervention is ideal for osteoporosis because many of its risk factors are modifiable, such as poor dietary calcium intake and limited amounts of physical activity. It also has the potential to improve poor compliance with osteoporosis medications. Previous studies have shown that interventions ranging from several weeks long to single sessions can result in increased knowledge about osteoporosis and increased calcium consumption and more weight-bearing exercises.[234]
Most educational programs contain information on risk factors for osteoporotic fracture such as low bone mass, lifestyle, family history, comorbid medical conditions, medication use, and falls. In addition to education, awareness of the individual risk for fracture may help to motivate behavioral improvements regarding bone health. In a previous study, we developed the Korean Fracture Risk Score (KFRS) as a novel predictive model for the risk of osteoporotic fracture over 7 years in Koreans.[5] It is used for the service of predicting fracture risk in Korean over 50 years provided by National Health Insurance Corporation. We hypothesized that if patients knew their risk of fracture, they would try to reduce the risk by improving lifestyle habits. The purpose of this study was to determine the impact of educational intervention including information about absolute fracture risk on the knowledge of osteoporosis and modifiable risk factors among Korean osteoporosis patients.
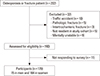
The present study enrolled 222 eligible candidates who visited the outpatient clinic with diagnoses of osteoporosis and volunteered to participate in the study between December 1, 2014 and September 17, 2015. Patient registration was performed in the endocrinology and orthopedics outpatient clinics of five hospitals. Inclusion criteria were subjects ≥50 years of age, not residing in a long-term care facility, able to understand the program information and consent form, and willing and able to answer questions via interviews. Of these candidates, 32 (14.4%) subjects were excluded if they had a fracture related to traffic accident, had a pathological fracture or intertrochanteric fracture, were not able to visit next session, or were mentally unstable. Eleven (5.0%) subjects were excluded due to refusal to participate in the follow-up survey. Ultimately, 179 subjects (15 males and 164 females) were deemed eligible and were included in the analyses (Fig. 1). Participants who provided written informed consent completed their surveys and then attended individual education programs. Demographic and anthropometric data and clinical risk factors used in the KFRS [5] were collected at baseline (prior to education). The follow-up survey was conducted at the second visit three months later. The study protocol was reviewed and approved by the Institutional Review Board (IRB) of Wonkwang University Sanbon Hospital (IRB No. 2014-32).
All participants received information about their individual risks for osteoporotic fracture, nutrition and lifestyle modifications to improve bone mass. We informed them of their risks of osteoporosis fracture within 7 years calculated via the KFRS. The KFRS is a Korean fracture risk calculation tool for which detailed methods have been previously published.[5] Clinical risk factors used in the KFRS were age, gender, body mass index (BMI), recent fragility fractures, current smoking status, heavy alcohol intake, weekly exercise of one or more times, recent use of oral glucocorticoids, rheumatoid arthritis, and other causes of secondary osteoporosis. Other causes of secondary osteoporosis included drugs such as anticonvulsants, anticoagulants (e.g., warfarin and heparin), aromatase inhibitors, and a suppressive dose of thyroid hormone; thyrotoxicosis; hyperparathyroidism; hyperprolactinemia; hypopituitarism; Cushing's syndrome; hypogonadism; premature menopause (<45 years); chronic renal failure; chronic obstructive lung disease; bypass surgery; inflammatory bowel disease; multiple myeloma; and idiopathic hypercalciuria. The risk of osteoporotic fracture is presented in comparison with the average risk within the same age, taking into account gender and age. It is classified into five groups according to rankings (Very high, High, Average, Low, and Very low).
The participants received educational materials on osteoporosis (developed by the Korean Society for Bone and Mineral Research) and attended an individualized education program. The education program consisted of the following: 1) basic summaries of what osteoporosis is and its risk factors; 2) nutritional education stressing the importance of calcium and vitamin D intake; and 3) an interactive exercise presentation. Education session was performed by nurse.
The primary outcome measure was knowledge change, assessed using the Osteoporosis Knowledge Assessment Test (OKAT) developed by Winzenberg et al.[6]. We evaluated current knowledge about osteoporosis before and after the educational intervention. The OKAT was developed based on the Osteoporosis Australia Prevention and Self-Management courses and promotional material. The OKAT is a validated and reliable questionnaire for the assessment of knowledge about osteoporosis. The questionnaire had a satisfactory index of difficulty and item discrimination. The 20 item had a Ferguson's sigma of 0.96 and a Cronbach's α of 0.69. The OKAT questionnaire comprises 20 items for the assessment of knowledge about osteoporosis; the first 12 questions assess knowledge, questions 13 to 16 assess attitude to osteoporosis, and the last 4 questions assess practice and perception towards the prevention of osteoporosis. It consists of multiple choice questions with each question having 3 answers (true, false, and I don't know). The analysis was performed by scoring 1 for a correct response and 0 for an incorrect or “I don't know” response. The total score could range from 0 to 20, with higher scores indicating greater comprehension of osteoporosis.
We calculated the required study sample size. According to the Korea National Health and Nutrition Examination Survey 2008 to 2009, the estimated diagnosis rate was 26.2% (women 29.9% and men 5.8%) and the treatment rate was 12.8% (women 14.4% and men 4.0%).[7] Based on a power of 80%, a significance level of 5%, and the estimated increase in the treatment rate after intervention of 22.4% (75% increase), 168 was found to be the optimal sample size. Considering an expected drop-out rate of 20% during follow-up, 202 patients were included in the intervention study. All data are expressed as mean±standard deviation for continuous variables and number (percentage) for categorical variables. Descriptive statistics were obtained to report demographic, socioeconomic status, and lifestyle characteristics. In order to be conservative, Spearman's correlation coefficients were determined for pairs of continuous variables. The paired t-test was used to determine whether the difference between the pre- and post-tests were significant. McNemar's test was obtained for each item of the adapted OKAT. Post-hoc analyses focused on individual test items using McNemar's test to compare the pre- and post- results obtained for each question. Statistical analyses were performed using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA), and P<0.05 was considered statistically significant.
A total of 179 (80.6%) out of 222 potentially eligible participants were enrolled in this study. Demographic characteristics of these 179 participants are summarized in Table 1.
Table 2 provides the frequency of correct responses for each item in both baseline and follow up surveys. The item with the highest percentage of correct answers was “Osteoporosis leads to an increased risk of bone fractures” (79.3%). On the other hand, “Any type of physical activity is beneficial for osteoporosis” and “From age 50, most women can expect at least one fracture before they die” had the lowest percentage of correct answers (16.8%–36.3%). The results indicated a statistically significant difference for 11 out of 20 questions in the frequency of correct responses. For example, patients reported the highest increase in knowledge on the following: “Alcohol in moderation has little effect on osteoporosis” and “Having a higher peak bone mass at the end of childhood gives no protection against the development of osteoporosis in later life.” After the educational intervention, the osteoporosis knowledge score had significantly increased from a mean of 10.6±5.7 at pre-education (baseline) to 11.7±6.3 at post-education (P<0.001). Of these 179 participants, 99 (55.3%) participants had improved osteoporosis knowledge scores while 46 (25.7%) had worse scores. This means that knowledge and awareness of osteoporosis had increased after receiving counseling and education.
The 7-year risk of osteoporotic fracture was calculated via the KFRS at baseline and follow up. At the baseline visit, the overall average risk was 28.0%. It was much higher in women (91.6%) than in men (8.4%) (Table 3). The distribution of fracture risk for the “Very high risk group” was 67.6%, followed by 10.6% for the “Average risk group” and 10% for the “High risk group”. Comparing the results at pre- and post-education, there was little difference between the “Very low risk group” and the “Low risk group.” However, the proportion of patients in the “Very high risk group” and “High risk group” dropped from 77.6% to 76.0%. There was a statistically significant decrease in the mean risk of fracture from 28.0% to 25.7% by about 2.3% (P<0.05). To determine the risk factors affecting fracture risk reduction, we analyzed the change in modifiable risk factors such as physical activity, smoking and alcohol consumption. There was no change in smoking status and alcohol behavior. We found that the proportion of subjects who exercise more than once a week had increased (Fig. 2).
In the present study, we have evaluated the effect of the education and information about individual fracture risk of osteoporosis knowledge and life style. We observed that simple educational intervention using written material was helpful to increase osteoporosis knowledge in osteoporosis patients. Additional information about fracture risk was considered to be helpful in changing lifestyles.
Most studies on the effectiveness of educational programs are targeted at community residents.[38] Although the content of program was similar, intervention was conducted with various tools (e.g., written material, power point presentation or video). Some of them were one session,[91011] but the Osteoporosis Prevention and Self-Management Course (OPSMC) developed in Australia was conducted once a week for 4 weeks.[212] In this study, we conducted one session of education using written materials for osteoporosis patients in hospital. The finding of an increase in participant knowledge is consistent with other osteoporosis intervention.[348] The baseline OKAT score for the current study (mean score, 10.6) was greater than that found in other studies.[48] The mean change in knowledge score of 1.1 observed in the current study shows that the increase in knowledge following the education was lower in magnitude to that seen in the previous study.[8] In our study, the participants visited the outpatient clinic for osteoporosis, so they may have had a high knowledge of osteoporosis. According to a study comparing a 4 weeks and a one session course, both improved osteoporosis knowledge but 4 week course only blunted decline in the use of osteoporosis medication.[4] If we develop more detailed education program such as OPSMC, the effect would have been more marked.
The most effective intervention should motivate individuals to change their behaviors. Increased osteoporosis knowledge does not always lead to changes in behavior.[13] In addition to the education provided in this study, we provided information on the 7-year fracture risk calculated using the KFRS to motivate changes in patient behavior. The KFRS tool offers a more precise prediction of total fracture risk by including epidemiologically-derived risk factors. In a recent study, use of the fracture-risk assessment tool, introduced by the World Health Organization, did not change physician prescribing behavior for patients at increased risk of fracture when included in the bone density report.[14] In our study, we focused on the behavioral changes of patients, not physicians. Risk factors that can be modified include dietary intake of calcium and vitamin D, physical activity, low BMI, excessive alcohol use, and smoking. We did not measure dietary calcium and vitamin D intake. It is not very surprising that the interventions did not influence smoking status and alcohol intake in our study since only a small number of subjects were current smokers (0.6%) or drank alcohol (10.1%). However, the proportions that exercised regularly have increased and the mean value of KFRS slightly decreased after the educational intervention. The findings of this study suggested that patients may be motivated by the knowledge of high fracture risk to initiate better health behaviors. Therefore, the need to use the fracture risk calculation tool in clinical practice should be emphasized more.
The strength of this study is that we performed multi-center study and provided the information about fracture risk calculated by Korean specific tool. Our study had several limitations. First, this study probably included participants that are more motivated and inclined to change their behavior than those from the general population. Therefore, we cannot be certain that our results are generalizable to other populations. Second, there was no control group, thus, it is difficult to confirm the additional benefit of providing a fracture risk. Another limitation is that there may be differences in the education program depending on the center. To overcome this, standardized educational material and questionnaires were used. Third, we performed follow-up the survey at 3 months after the initial visit. Longer follow-up periods are desirable to assess the impact on chronic diseases such as osteoporosis. Further, it relied on patients' self-reports of their lifestyle behaviors, which may not be accurate. Finally, we did not measure self-efficacy data. Information-only interventions (e.g., media awareness campaigns, leaflets) are insufficient to change behavior.[151617] Behavioral change is predicted by knowledge when mediated by attitudes and self-efficacy.[18] Therefore, education must focus on improving self-efficacy in addition to knowledge. Further studies should focus on longer-term follow-up, looking at self-efficacy change and behavioral change.
In conclusion, simple educational intervention is effective in increasing osteoporosis knowledge among Korean osteoporosis patients. It may confer additional benefits by providing information about osteoporotic fracture risks. Awareness is important in the prevention or treatment of chronic diseases such as osteoporosis. Therefore, it will contribute to reducing the burden of diseases that provide opportunities for osteoporosis education at the national level.
Figures and Tables
References
1. Lee SR, Ha YC, Kang H, et al. Morbidity and mortality in Jeju residents over 50-years of age with hip fracture with mean 6-year follow-up: a prospective cohort study. J Korean Med Sci. 2013; 28:1089–1094.

2. Winzenberg TM, Oldenburg B, Frendin S, et al. Effects of bone density feedback and group education on osteoporosis knowledge and osteoporosis self-efficacy in premenopausal women: a randomized controlled trial. J Clin Densitom. 2005; 8:95–103.

3. Brecher LS, Pomerantz SC, Snyder BA, et al. Osteoporosis prevention project: a model multidisciplinary educational intervention. J Am Osteopath Assoc. 2002; 102:327–335.
4. Laslett LL, Lynch J, Sullivan TR, et al. Osteoporosis education improves osteoporosis knowledge and dietary calcium: comparison of a 4 week and a one-session education course. Int J Rheum Dis. 2011; 14:239–247.

5. Kim HY, Jang EJ, Park B, et al. Development of a Korean fracture risk score (KFRS) for predicting osteoporotic fracture risk: Analysis of data from the Korean national health insurance service. PLoS One. 2016; 11:e0158918.

6. Winzenberg TM, Oldenburg B, Frendin S, et al. The design of a valid and reliable questionnaire to measure osteoporosis knowledge in women: the Osteoporosis Knowledge Assessment Tool (OKAT). BMC Musculoskelet Disord. 2003; 4:17.

7. Choi YJ, Oh HJ, Kim DJ, et al. The prevalence of osteoporosis in Korean adults aged 50 years or older and the higher diagnosis rates in women who were beneficiaries of a national screening program: the Korea National Health and Nutrition Examination Survey 2008–2009. J Bone Miner Res. 2012; 27:1879–1886.

8. Francis KL, Matthews BL, Van Mechelen W, et al. Effectiveness of a community-based osteoporosis education and self-management course: a wait list controlled trial. Osteoporos Int. 2009; 20:1563–1570.

9. Kulp JL, Rane S, Bachmann G. Impact of preventive osteoporosis education on patient behavior: immediate and 3-month follow-up. Menopause. 2004; 11:116–119.

10. Evenson AL, Sanders GF. Educational intervention impact on osteoporosis knowledge, health beliefs, self-efficacy, dietary calcium, and vitamin D intakes in young adults. Orthop Nurs. 2016; 35:30–36. quiz 7-8.

11. Beaudoin C, Bessette L, Jean S, et al. The impact of educational interventions on modifiable risk factors for osteoporosis after a fragility fracture. Osteoporos Int. 2014; 25:1821–1830.

12. Tanner EK. Chronic illness demands for self-management in older adults. Geriatr Nurs. 2004; 25:313–317.

13. Kasper MJ, Peterson MG, Allegrante JP. The need for comprehensive educational osteoporosis prevention programs for young women: results from a second osteoporosis prevention survey. Arthritis Rheum. 2001; 45:28–34.

14. Izuora KE, Alazraki N, Byrd-Sellers J, et al. Fracture assessment tool risk scores in bone density reports do not change physician prescribing behavior for osteoporosis. Am J Med Sci. 2011; 342:5–8.

15. Winzenberg T, Oldenburg B, Frendin S, et al. The effect on behavior and bone mineral density of individualized bone mineral density feedback and educational interventions in premenopausal women: a randomized controlled trial [NCT00273260]. BMC Public Health. 2006; 6:12.

16. Guilera M, Fuentes M, Grifols M, et al. Does an educational leaflet improve self-reported adherence to therapy in osteoporosis? The OPTIMA study. Osteoporos Int. 2006; 17:664–671.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download