Abstract
Background
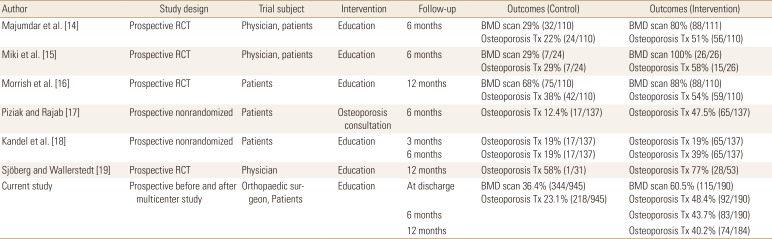
The authors had earlier conducted a retrospective cohort study from 2008 to 2011 in Jeju Island, among 945 hip fracture patients above 50 years of age. Of these 945 patients, 344 patients (36.4%) underwent a bone mineral density test and 218 patients (23.1%) received treatment for osteoporosis. The purpose of this study was to determine whether a patient education program could improve osteoporosis management after hip fracture. The data of the previous study was used for comparison.
Methods
From November 1, 2014 to September 30, 2015, 190 patients above 50 years of age who were admitted for hip fractures at six different hospitals, were enrolled in the present study. During the hospitalization period, patients underwent education sessions and were provided brochures. Patients were evaluated for diagnosis and treatment of osteoporosis at six months after discharge and were followed-up for at least a year.
Results
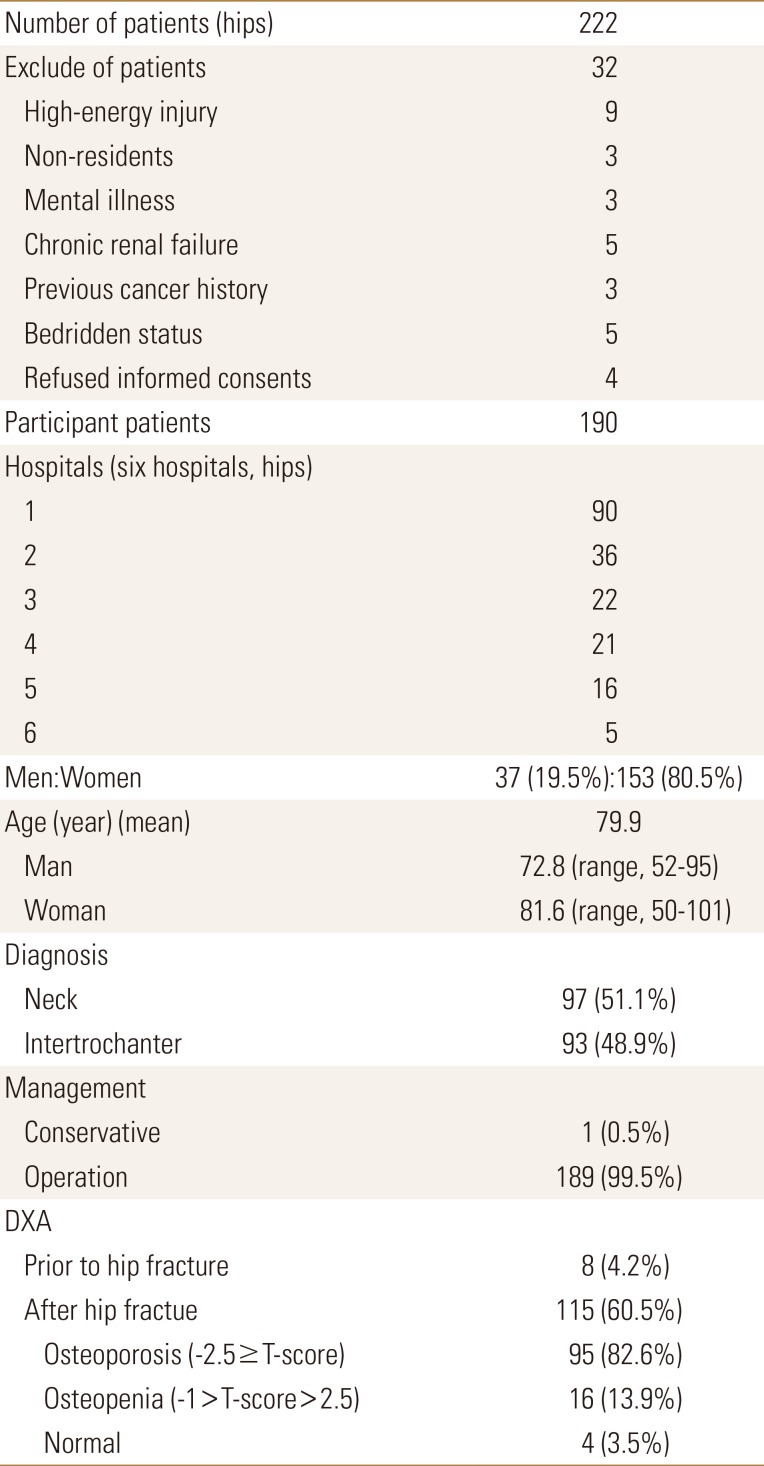
Of the 222 patients with hip fractures, 190 patients (37 men, 153 women) were enrolled at six hospitals in 2015. Dual energy X-ray absorptiometry was performed on 115 patients (60.5%) and 92 patients (48.4%) were prescribed medication for osteoporosis at the time of discharge. A total of 43.7% and 40.2% of the patients were found to be compliant with osteoporosis medication at 6 months and 12 months follow-up respectively.
Go to : 
Hip fracture is most serious complication of osteoporosis related fractures and is associated with several adverse effects in the elderly. The incidences of hip fracture in global populations are reporting that number and incidence of hip fracture are increasing trends.[1] In Korea, numbers and incidence of hip fracture is also expected increasing trend until 2026.[2] Hip fractures are notorious high mortality, morbidity, secondary hip fracture, and considerable socioeconomic burdens.[345]
To minimize complications after hip fracture, appropriate osteoporosis medication are recommend to reduce risks of subsequent fractures and mortality.[678] However, treatment rates after osteoporotic fracture are still insufficient.[910] To improve diagnosis and treatment rate of osteoporosis, physician, patients, and reimbursement system are very important.[11]
Previously we reported that increased awareness of orthopaedic surgeons after educations improved the detection rate of osteoporosis from 20.1% to 45% and treatment rates from 15.1% to 32.2%.[12] However, during follow-up, maintenance of osteoporosis medication was steeply reduced 12% at mean of 9.5 months follow-up.[12] In addition, follow-up observational study after finishing interventional study was disappointed,[13] detection and treatment rate of osteoporosis following hip fracture in same cohort from 2008 to 2011 were still not enough (mean, 36.4% [range, 24.2%–40.5%]; mean, 23.1% [range, 20%–29%], respectively).[13]
Therefore, we designed additional intervention studies for patients with hip fracture are required to further improvement of osteoporosis treatment rates after hip fracture. This prospective intervention multicenter study was to determine whether an education program after surgery in patients with hip fracture could increase the osteoporosis treatment rate after a hip fracture, and to confirm maintenance of osteoporosis medications.
Go to : 
The design and protocol of this study was approved by the Institutional Review Board (IRB) at our hospital. Patients were informed their medical data might be used in a scientific study and provided consent.
This prospective interventional multicenter study was performed on patients over 50 years of age who were admitted for a hip fracture between November 1, 2014 and September 30, 2015 at the six hospitals. There are six hospitals (one university hospital and five general hospitals) on the island with orthopedic department and emergency admission facilities and all hospitals used dual energy X-ray absorptiometry (DXA) to determine bone mineral densities. Medical charts and radiological records were reviewed. Patients who met the diagnostic criteria of a femoral neck or intertrochanteric fractures based on the International Classification of Diseases, 10th revision (ICD-10; S720, S721) and who were over 50 years of age at fracture diagnosis were enrolled. The exclusion criteria were; a non-resident of Jeju Island, a pathologic bone fracture (metastasis), serious medical illness including chronic renal failure, cancer history, mental illness, and refusal of participating study. Diagnosis at admission, mechanism of injury, detection of osteoporosis (DXA), and procedures performed during hospitalization, and discharge medications were then extracted and analyzed.
We calculated the required study sample size using the 2008 to 2011 data, in which the initiation rate of osteoporosis treatment was 23.1% (218/945 patients).[13] Based on a power of 80%, significance level of 5%, and an estimated increasing rate of osteoporosis treatment of 17.3% in the patients who were diagnosed with hip fracture, the inclusion of 112 patients was estimated as optimal sample size. Since we expected a drop-out rate of 20% during follow-up due to the high mortality rate after hip fracture, we included 135 patients.
Prior to start intervention study, all of orthopaedic surgeons and assistants in the cohort completed standardization for patient's education. To standardization of patient's education, all orthopaedic surgeon and participant were provided with education sessions at prior to study. The education program included the relationship between osteoporosis and hip fracture, necessity of DXA for the detection of osteoporosis, importance of osteoporotic drugs in its treatment and routine follow-up for medication. After acquiring informed consent, patients at six hospitals were provided with education sessions during admission and brochures for increasing osteoporosis management. These education sessions involved providing information on the knowledge of osteoporosis, exercise and foods for preventing osteoporosis, the efficacy of DXA for the diagnosis of osteoporosis, the effectiveness of osteoporotic drugs and the importance of follow-up for the management of osteoporosis and of routine orthopaedic follow-up. Diagnosis at admission, mechanism of injury, detection of osteoporosis (DXA), procedures performed during hospitalization, and discharge medications were extracted from hospital records and analyzed. Osteoporosis treatment was defined as medication including a selective estrogen receptor modulator (SERM), bisphosphonate, or calcitonin therapy or parathyroid hormone (PTH) therapy. Treatment initiation and duration were confirmed by reviewing medical records at 6 months and 12 months after discharge from hospital.
Mortality status of the patients was identified from hospital record and/or interview with patient's family. In addition, a death certificates at the National Registry Office were search for information on patients lost to follow-up.
The primary study outcome was detection rate of osteoporosis (DXA) and rate of osteoporosis medication at 6 months after discharge from hospital. Secondary outcome was treatment rate of osteoporosis at 12 months follow-up.
The χ2 test was used to analyze categorical variables. P-values were reported two sided, with P<0.05 indicating statistical significance. Statistical analyses were performed using SPSS software version 19.0 (SPSS Inc., Armonk, NY, USA).
The design and protocol of this study were approved by the IRB at the Jeju National University Hospital (JNUH-IRB No. 2014-12-001). Informed consent was submitted by all subjects when they were enrolled.
Go to : 
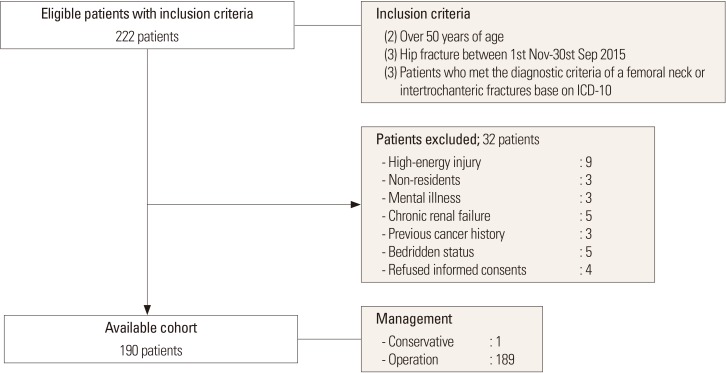
During study periods, 222 patients that sustained a hip fracture and who were treated at one of the six participating hospitals were identified as possible candidates for this study. Thirty-two patients were excluded for the following reasons; nine for a high-energy injury resulting from a traffic accident or a fall from height, three because they were non-residents, three for mental illness, five for chronic renal failure, three for previous cancer history, five for bedridden status, and four who refused informed consents (Fig. 1). One hundred ninety patients (37 men and 153 women) patients with a hip fracture, 97 femoral neck fractures (51.1%) and 93 intertrochanteric fractures (48.9%) were enrolled. Mean age at time of diagnosis was 79.9 years (72.8 years in men [range, 52–95 years]; and 81.6 years in women [range, 50–101 years]). Of these 190 patients, 189 patients underwent surgery, but one patient underwent conservative treatment for a non-displaced fracture (Table 1).
Eight of the 190 patients had received a diagnosis of osteoporosis prior to hip fracture, but only two of these eight were taking prescribed osteoporosis medications at time of admission. After education sessions, DXA was performed on 115 patients (60.5%) during admission and first visit of out-patients clinics after discharge; at the hip and spine in 90 and at the spine in 25. Of them, there were 95 patients (82.6%) in osteoporosis (T-score≤−2.5), 16 patients (13.9%) in osteopenia (−2.5<T-score<−1) and four patients in normal.
Of these 115 patients, 92 patients (80%) were prescribed osteoporosis medications (73 patients [79.3%] in bisphosphonates, 16 patients in SERM, and 3 in PTH) at time of discharge and first visit of out-patients clinic after discharge. Other anti-osteoporotic drugs, such as, calcitonin, and hormone replacement therapy were not prescribed. At six months follow-up, 83 patients (72.2%) were maintained osteoporosis medications (67 patients in bisphosphonates, 13 patients in SERM, and 3 in PTH). Six patients were stopped medication due to gastrointestinal-related complication and 3 patients were loss of follow-up. At 12 months follow-up, 74 patients (64.3%) were maintained osteoporosis medications (63 patients in bisphosphonates and 11 patients in SERM). Two patients were refused osteoporosis medications due to difficulty of medication and/or complications. Six patients were died during follow-up. One patient was lost of follow-up at 12 months follow-up.
Go to : 
Undertreatments of osteoporosis in patients with hip fracture are notorious and considering problems to overcome. We found that improvement of patient's awareness through education could lead to increase rate of detection and treatment of osteoporosis after hip fracture. Comparing with previous reports (36.4% of BMD testing and 23.1% of osteoporosis medication) in the same cohort,[13] education of patients with hip fracture are increasing 60.5% of BMD testing, and 48.4% of osteoporosis medication at discharge and 40.2% of osteoporosis medication at the 12 months follow-up.
Several interventional studies for improving osteoporosis management following hip fracture have demonstrated that patients and/or physicians education can lead to improvement of initiation rate of anti-osteoporosis medications in patients with hip fracture.[141516171819] Previously, we performed interventional study for improving orthopaedic surgeon awareness and reported an improved medication rate of osteoporosis from 15% to 32% in patients with hip fracture.[12] However, 32% of the osteoporosis treatment rate at six months following hip fracture was still lower than other intervention studies.[12] Therefore, we designed multimodal interventional study for patients and orthopaedic surgeons and resulted in improvement of osteoporosis medication from 23.1% to 40.2% at 12 months follow-up.
In terms of medication persistence in interventional study, for preventive effect of osteoporotic fracture, anti-osteoporosis medication should be taken for minimum 6 months. [20] However, medication duration times in several studies are relatively short within 6 months.[20] Increasing rate of osteoporosis medication in patient with hip fracture use beyond 6 months of the intervention ranged from 16% to 34.1% (Table 2).[141516171819] Our findings are corresponded with other previous reports. In this study, comparing with control group, increasing rate of anti-osteoporosis medication was increased by 17.2% and medication persistence was 40.2% at the 12 months follow-up. Especially, intervention study for patients with hip fracture is important advantage, because patients after surgical intervention should be recommended regularly scheduled visits for radiological and clinical evaluations.
So far, intervention studies have involved one or two specific centers, and it is difficult to extrapolate their results at other university and local hospitals. The results of this multicenter study could be shown possibility to expendable an effective and easily applied intervention method in osteoporotic patients with a hip fracture. The fracture liaison services for hip fracture patients have been introducing since last decade. Fracture liaison services are proven as an effective method to address the post-fracture care gap, cost effectiveness, and to reduce the risk of secondary fracture.[11212223] Program of fracture liaison service are mainly consisted with patient's education including knowledge of osteoporosis, importance of anti-osteoporosis medications, calcium and vitamin D rich food intake, and physical exercise.[24] Education programs in this study were very similar to program of fracture liaison service. Therefore, success of this prospective multicenter interventional study was shown possibility of conversion to fracture liaison service in Korea.
This study has some limitations. First, this study was performed in various hospital settings within the same cohort, although education programs were standardized in all institutions. Second, the medical care system in Korea is not a same to other countries, because orthopedic surgeons undertake the role of primary care physicians after surgery. Therefore, the results of intervention programs in this study might be difficult to generalize in the other countries. However, recent studies have shown that the active participation of orthopedic surgeons is possible to improve osteoporosis treatment in patients with hip fracture. Finally, comparing control study, two hospitals had to exclude because of IRB permission. This change might have influenced on the outcomes.
Go to : 
In conclusion, the osteoporosis detection and medication rate after hip fracture increased two fold after the multimodal approach with orthopaedic surgeon and patients. This interventional multicenter study demonstrate that patients education program in patients with hip fracture can improve osteoporosis medication and well maintained up to 12 months follow-up and could be possible to potentially converse to fracture liaison service.
Go to : 
ACKNOWLEDGMENT
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Korea (grant number : HI13C1522, HI15C1189).
Go to : 
References
1. Ha YC, Park YG, Nam KW, et al. Trend in hip fracture incidence and mortality in Korea: a prospective cohort study from 2002 to 2011. J Korean Med Sci. 2015; 30:483–488. PMID: 25829818.

2. Ha YC, Kim TY, Lee A, et al. Current trends and future projections of hip fracture in South Korea using nationwide claims data. Osteoporos Int. 2016; 27:2603–2609. PMID: 27112763.

3. Abrahamsen B, van Staa T, Ariely R, et al. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2009; 20:1633–1650. PMID: 19421703.

4. Choi HJ, Shin CS, Ha YC, et al. Burden of osteoporosis in adults in Korea: a national health insurance database study. J Bone Miner Metab. 2012; 30:54–58. PMID: 21633927.

5. Lee SR, Ha YC, Kang H, et al. Morbidity and mortality in Jeju residents over 50-years of age with hip fracture with mean 6-year follow-up: a prospective cohort study. J Korean Med Sci. 2013; 28:1089–1094. PMID: 23853495.

6. Lee YK, Ha YC, Yoon BH, et al. Incidence of second hip fracture and compliant use of bisphosphonate. Osteoporos Int. 2013; 24:2099–2104. PMID: 23247329.

7. Lee YK, Ha YC, Choi HJ, et al. Bisphosphonate use and subsequent hip fracture in South Korea. Osteoporos Int. 2013; 24:2887–2892. PMID: 23681088.

8. Lyles KW, Colón-Emeric CS, Magaziner JS, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007; 357:1799–1809. PMID: 17878149.

9. Shibli-Rahhal A, Vaughan-Sarrazin MS, Richardson K, et al. Testing and treatment for osteoporosis following hip fracture in an integrated U.S. healthcare delivery system. Osteoporos Int. 2011; 22:2973–2980. PMID: 21271339.

10. Lai MM, Ang WM, McGuiness M, et al. Undertreatment of osteoporosis in regional Western Australia. Australas J Ageing. 2012; 31:110–114. PMID: 22676170.

11. Bogoch ER, Elliot-Gibson V, Beaton DE, et al. Effective initiation of osteoporosis diagnosis and treatment for patients with a fragility fracture in an orthopaedic environment. J Bone Joint Surg Am. 2006; 88:25–34.

12. Kim SR, Ha YC, Park YG, et al. Orthopedic surgeon's awareness can improve osteoporosis treatment following hip fracture: a prospective cohort study. J Korean Med Sci. 2011; 26:1501–1507. PMID: 22065908.

13. Kim SR, Park YG, Kang SY, et al. Undertreatment of osteoporosis following hip fractures in jeju cohort study. J Bone Metab. 2014; 21:263–268. PMID: 25489575.

14. Majumdar SR, Beaupre LA, Harley CH, et al. Use of a case manager to improve osteoporosis treatment after hip fracture: results of a randomized controlled trial. Arch Intern Med. 2007; 167:2110–2115. PMID: 17954806.
15. Miki RA, Oetgen ME, Kirk J, et al. Orthopaedic management improves the rate of early osteoporosis treatment after hip fracture. A randomized clinical trial. J Bone Joint Surg Am. 2008; 90:2346–2353. PMID: 18978403.
16. Morrish DW, Beaupre LA, Bell NR, et al. Facilitated bone mineral density testing versus hospital-based case management to improve osteoporosis treatment for hip fracture patients: additional results from a randomized trial. Arthritis Rheum. 2009; 61:209–215. PMID: 19177538.

17. Piziak VK, Rajab MH. An effective team approach to improve postoperative hip fracture care. J Orthop Trauma. 2011; 25:72–75. PMID: 21245708.

18. Kandel L, Schler D, Brezis M, et al. A simple intervention for improving the implementation rate of a recommended osteoporosis treatment after hip fracture. Endocr Pract. 2013; 19:46–50. PMID: 23186951.

19. Sjöberg C, Wallerstedt SM. Effects of medication reviews performed by a physician on treatment with fracture-preventing and fall-risk-increasing drugs in older adults with hip fracture-a randomized controlled study. J Am Geriatr Soc. 2013; 61:1464–1472. PMID: 24028354.

20. Gallagher AM, Rietbrock S, Olson M, et al. Fracture outcomes related to persistence and compliance with oral bisphosphonates. J Bone Miner Res. 2008; 23:1569–1575. PMID: 18505366.

21. Sale JE, Beaton D, Posen J, et al. Systematic review on interventions to improve osteoporosis investigation and treatment in fragility fracture patients. Osteoporos Int. 2011; 22:2067–2082. PMID: 21607808.

22. Eisman JA, Bogoch ER, Dell R, et al. Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res. 2012; 27:2039–2046. PMID: 22836222.

23. Ganda K, Puech M, Chen JS, et al. Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int. 2013; 24:393–406. PMID: 22829395.

24. Bogoch ER, Elliot-Gibson V, Beaton D, et al. Fracture prevention in the orthopaedic environment: outcomes of a coordinator-based fracture liaison service. J Bone Joint Surg Am. 2017; 99:820–831. PMID: 28509822.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download