Abstract
Objective
This study aimed to explore the usefulness of adjunctive buccal and palatal corticotomy for adult maxillary expansion in an animal model using cone-beam computed tomography (CBCT).
Methods
Twelve adult sheep were randomly divided into two groups (each n = 6): a control group, where no treatment was administered, and a treatment group, where buccal and palatal corticotomy-assisted maxillary expansion was performed. CBCT scans were taken before (T1) and after (T2) treatment. Differences in all transverse dental and alveolar dimensions, alveolar width at crest level, hard palate level, horizontal bone loss, interdental cusp width and inter-root apex were assessed using Wilcoxon signed-rank and Mann-Whitney U-tests. Kruskal-Wallis tests and pairwise comparisons were used to detect the significance of differences among the inter-premolar and inter-molar widths.
Results
CBCT data revealed significant changes in all transverse dental and alveolar dimensions. The mean interpremolar alveolar width showed an increase of 2.29 to 3.62 mm at the hard palate level, 3.89 to 4.38 mm at the alveolar crest level, and 9.17 to 10.42 mm at the buccal cusp level. Dental changes in the vertical dimension were not significant.
Conclusions
Our findings based on an adult animal model suggest that adjunctive buccal and palatal corticotomy can allow for both skeletal and dental expansion, with the amount of dental expansion exceeding that of skeletal expansion at alveolar crest and hard palate levels by two and three folds, respectively. Therefore, this treatment modality is potential to enhance the outcomes of maxillary expansion in adults.
Transverse maxillary deficiency is one of the most common orthodontic problems in both children and adults. This condition leads to an unattractive smile and improper occlusion, thus raising esthetic as well as functional concerns to the patients. Currently, the main treatment approached for this condition involve nonsurgical and surgical expansion.12
Nonsurgical expansion entails the use of several appliances, including removable and fixed appliances. These maxillary expanders have been used with various effects on the dental alveolar and underlying skeletal bone. In recent years, rapid maxillary expander (RME) has gained popularity.3456 McNamara et al.3 and Gurel et al.4 stated that the maxilla could be expanded up to 7 mm or more in children aged less than 13 years. The total expansion in this young age group is generally attributed to opening of the midpalatal suture and displacement of the alveolar bone in a ratio of 1:1.27 However, a similar method of expansion was less successful in adults.689 Some hypotheses have been proposed to explain the discrepancy in treatment outcomes between adults and children, with the main cause considered to be the increased interdigitation of the midpalatal suture in patients aged more than 14 years. Angelieri et al.,10 in 2013, proposed five stages of maturation of the midpalatal suture. From stage A to stage C, the suture is increasingly tortuous and fusion is in the initial stages. RME can be carried out in patients in these stages with good skeletal effects. In stages D and E, ossification between the two halves of the palate occurs in a posterior to anterior direction; this makes suture opening via RME impossible. In such cases, the maxilla can be expanded using surgically assisted rapid maxillary expansion (SARME), which involves surgical splitting of the anterior nasal spine and osteotomy or buccal corticotomy. Although fusion begins earlier than 11 years of age in girls, 21% girls aged more than 18 years are still found to be in stages B and C. In addition, only 58% girls and 23% boys aged 11 to 19 years are found to have reached stages D and E. Knaup et al.11 revealed a low percentage of ossification in the suture in all subjects aged 18 to 63 years; consequently, they rejected this hypothesis. Korbmacher et al.12 published similar findings, suggesting that the rate of suture obliteration was very low and independent of chronological age in human specimens aged 14 to 71 years.
Recently, corticotomy has been attracting considerable interest in the field of orthodontics. The concept of “bony block movement,” which was first introduced by Kole,13 was believed to enhance tooth movement in various cases. Later, Suya modified Kole's technique and referred to it as “corticotomy-facilitated orthodontics.”14 However, both authors applied their theories for individual tooth movement. Chung and co-workers1516 continued to develop Suya's concept to devise “speedy surgical orthodontics,” wherein the entire anterior segment is retracted. They showed that perisegmental corticotomy around the anterior segment could decrease the rigidity of the cortical bone, with bone-bending effects through heavy force application on the corticotomized segment. As a result, incisors can be retracted en-masse within 3 to 6 months, taking full advantage of the regional acceleratory phenomenon.
Corticotomy has been utilized for correction of maxillary constriction.1718 Lines17 introduced a method that combined incisions placed in the lateral walls of the maxillary sinus and mid-palatal sutures. Meanwhile, Echchadi et al.18 applied a new approach on a younger patient (14 years old) using piezo-bone perforations on the buccal alveolar bone. However, the effectiveness of corticotomy for maxillary expansion in adults is controversial, and the following question remains unanswered: if corticotomy can decrease the rigidity of the buccal and palatal alveolar bone, will it overcome existing limitations and increase the possibility of successful treatment outcomes in adults? Currently, there is no available literature on the usefulness of this method for moving blocks of teeth in the lateral dimension. Therefore, the purpose of this animal study was to investigate the usefulness of adjunctive buccal and palatal corticotomy for adult maxillary expansion using cone-beam computed tomography (CBCT).
This study used adult male Dorper sheep aged 20 to 48 months and weighing 50 to 60 kg, and it was conducted at the Animal Experimental Unit, Faculty of Veterinary Medicine, University Putra Malaysia (UPM), Malaysia. The study protocols were approved by the Institutional Animal Care and Use Committee (IACUC) at UPM (No. UPM/IACUC/AUP-R031). The sheep were selected according to the following inclusion criteria: good general health without any noticeable disease, eruption of all six maxillary premolars, absence of periodontal disease, and absence of any other intraoral infections.
The sample size was calculated using the formula of Mead: E = total number of animals − total number of groups, where E should be between 10 and 20.19 On the basis of these calculations, we included 12 sheep randomly divided into two groups (n = 6 each): a control group, where no treatment was performed, and a treatment group, where buccal and palatal corticotomy + RME was performed. All sheep were kept in a raised pen with a wooden floor for 1 month before the procedure for acclimatization. They were fed with custom-formulated food including pellets and grass in a ratio of 1:1 w/w and were provided with a mineral lick and pipe water.
All procedures, including CBCT, appliance fixation, and corticotomy, were performed under general anesthesia. The sheep were made to fast for 24 hours before anesthesia induction to minimize the risk of regurgitation. Anesthesia was induced with intravenous ketamine 7 mg/kg (Narketan® 10; Vetoquinol, Buckingham, UK) and diazepam 0.6 mg/kg (Diapine; Atlantic Laboratories Ltd., Bangkok, Thailand). Following endotracheal intubation, anesthesia was maintained with 2% to 3% isoflurane in 100% oxygen. Following corticotomy, the animals were injected with one dose of intramuscular antibiotics and analgesics. Intramuscular vitamin C and vitamin B were also administered to stimulate apatite formation.
RME was performed using a hyrax appliance comprising a 16-mm Super-Screw® (Great Lakes Orthodontics, Tonawanda, NY, USA) soldered on two bands placed on the first premolars and two bands placed on the third premolars. The Super-Screw® was positioned parallel to the midpalatal suture in the region of the second premolars and cemented using glass ionomer luting cement (Ketac™ Cem Easymix; 3M Deutschland GmbH, Neuss, Germany; Figure 1A).
All sheep in the treatment group underwent corticotomy involving the maxillary premolar segments. The buccal and palatal mucosae were infiltrated with lidocaine HCl 2% with epinephrine 1:100,000 (Lignospan; Septodont, Saint-Maur-des-Fossés, France). Cervical mucoperiosteal incisions were placed buccally and palatally along the gingival sulcus from the mesial of the first premolar to the mesial of the first molar, with the horizontal releasing incision at the mesial of the first premolar. A full-thickness flap was raised using a periosteal elevator to expose the alveolar bone. A 2-mm diameter round bur was used to perform decortication up to a depth of 2 to 2.5 mm, which is the average thickness of the cortical alveolar bone in sheep. On the buccal aspect, a cutting line was created 5 mm from the mesial alveolar crest of the first premolar; it extended upward in an orientation parallel to the axis of the first premolars, horizontally 2 to 5 mm above the premolar roots, and downward between the third premolar and first molar roots to the distal crest of the third premolar (Figure 1B). The vertical cuts on the palatal aspect were similar to those on the buccal aspect, with the horizontal lines placed approximately 5 mm from the cervical regions of the teeth (Figure 1C). The bone was cut under copious saline irrigation. The flaps were sutured using absorbable suture material (PDS™ Plus, 3–0; Ethicon, Sommerville, NJ, USA). Immediately after surgery, the hyrax appliance was cemented and the screw was turned by 1 mm. After 5 days, the screw was turned by 0.5 mm/day for 14 consecutive days in order to achieve 8 mm of arch expansion. The appliance was removed 4 weeks after the treatment followed by CBCT scans.
Before (T1) and after treatment (T2), CBCT (Fidex; Animage LLC., Pleasanton, CA, USA) was performed using the following parameters: voxel size, 0.3 mm; 110 kV; and 0.15 mA. The anteroposterior axis of the head was positioned paralleled to the center of the table. For measurement purposes, the transverse plane in all images was rotated so that it was parallel to the palatal plane, sagittal plane along the palatal suture and nasal septum, and coronal plane perpendicular to the nasal septum (Figure 2). Linear measurements, as defined in Table 1, were acquired using Fidex software (Animage LLC.). Mimics software version 19.0 (Materialise NV, Leuven, Belgium) was used for three-dimensional pre- and post-intervention superimposition.
All acquired data were analyzed using IBM SPSS Statistics version 20.0 (IBM Co., Armonk, NY, USA). Wilcoxon signed-rank nonparametric tests were used to assess differences between T1 and T2 within groups, while Mann-Whitney U-tests were used to assess differences between the two groups. Differences among the transverse dentoalveolar width at the first premolar, second premolar, third premolar, and first molar were tested using Kruskal-Wallis and pairwise comparison tests. A p-value of 0.05 was considered statistically significant.
All measurements were repeated 30 days after the first measurement by the same rater. Intraclass correlation coefficients (ICCs) were calculated to determine the intraexaminer reliability.
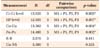
Opening of the midpalatal suture was not observed on any CBCT image. The control group showed no meaningful changes in any parameter after the study period for all parameters (p > 0.05, Table 2).
In contrast, the values of the maxillary expansion in the experimental group demonstrated that transverse maxilla was expanded significantly compared to control group (p < 0.05, Table 2). The alveolar width at the crest level (Cr-Cr level) showed the highest average increase of 4 mm in the premolar region (p < 0.05). Similarly, the alveolar width at the hard palate level (HP level) showed the maximum increase in the premolar region (2.29–3.12 mm, p < 0.05); this was approximately 50%–80% of the increase at the Cr-Cr level. The interpremolar width also increased significantly (9–10 mm) at the buccal cusp level (Cu-Cu level; p < 0.05). Not only the premolar crowns but also the root apices (2.47–2.91 mm, p < 0.05) moved substantially in the buccal direction. The amount of root movement (R-R) in the premolar region was approximately similar to the amount of increase in the alveolar width at the HP level (2.47–2.91 mm vs. 2.29–3.12 mm, respectively). The vertical tooth positions relative to the nasal line (Cu-NS) showed no significant changes after treatment (p > 0.05). Dental expansion was approximately 2 and 3 times greater than skeletal expansion at the Cr-Cr and HP levels, respectively. No evidence of root resorption was detected on the CBCT images. ICC was 0.87 for Cu-NS and > 0.94 for the other measurements, confirming high intraexaminer reliability.
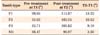
Tables 2 and 3 show that the increase in the alveolar width in the premolar region was four times that in the molar region at the Cr-Cr level (3.89–4.38 mm vs. 1.34 mm, p < 0.05) and two to three times that in the molar region at the HP level (2.29–3.62 mm vs. 0.86 mm, p < 0.05). Similarly, the increase in the alveolar width in the premolar region was five times that in the molar region at the Cu-Cu level (9.17–10.42 mm vs. 2.08 mm, p < 0.05). There were no significant differences in any parameter among the three premolars (p > 0.05, Table 3).
The T1 and T2 images revealed changes (red) in the regions of the incisions and no changes in mid-palatal region (Figure 3).
The effectiveness and stability of maxillary expansion in adults have been the subject of discussions for many years. Tightly interdigitated midpalatal sutures and the increasing rigidity of the surrounding bones are reported to be the causes of these unsatisfactory results.120 Chung and co-workers,1516 in 2009, suggested that decortication may overcome the rigidity of the surrounding bones. Therefore, this theory could be utilized in facilitating maxillary expansion in adults.
Our study was conducted in adult sheep because of the size of the maxilla in these animals. Compared with those in rodents, the palate and dental arch in sheep are wider and more suitable for the planned procedures. The shape of their teeth was also similar to that of human teeth, which aided in fabrication of the expansion appliance. A control group was included for comparison to eliminate the effects of natural skull growth. The acquired CBCT images confirmed that there was no opening of the midpalatal suture as a result of expansion, suggesting that the net effect of expansion was due to the intervention, not the separation of the suture.
According to a previous study, RME is the treatment of choice for growing adolescents.34518 However, nonsurgical maxillary expansion method has not been considered a viable option for adults because of interdigitation of the midpalatal suture. Accordingly, research on this approach for adults is rare. These authors have described that dental expansion up to 5 mm can be achieved using nonsurgical expansion, without a remarkable increment at the basal bone level.72122 Only one study7 reported that minimal expansion at the palatal roof (0.9 mm) was achieved when the gingival level was expanded up to 5.1 mm. In general, conventional maxillary expansion in adults can be primarily achieved by alveolar bending (82%).7 Compared with nonsurgical expansion, corticotomy-assisted expansion used in our study showed conspicuous basal bone expansion at the HP level (0.9 mm vs. 2.29–3.62 mm). In addition, the alveolar width at the Cr-Cr level expanded up to 4.38 mm. Thus, the increment at the palatal roof level contributed to approximately 50%–75% (2.29–3.62 mm/3.89–4.38 mm) of the total bone expansion. The remaining 25%–50% of the expansion was due to alveolar bending. Furthermore, the interpremolar width at the Cu-Cu level increased by 9–10 mm with a 8-mm increase by screw turns; this was noticeably higher than the amount achieved by the nonsurgical approach.
Currently, there are numerous reports on SARME, which can result in mean dental changes up to 12 mm.23 With regard to skeletal changes, the amount of expansion at the maxillary base is 2–5 mm, and 4–5 mm of expansion at the Cr-Cr level can be achieved by splitting the midpalatal suture in combination with osteotomy or partial corticotomy.23 The expansion achieved in our study was slightly less than that achieved by SARME (mean skeletal changes at the maxillary base: 2.29–3.62 mm vs. 2–5 mm, at the crestal level: 3.89–4.38 mm vs. 4–5 mm; mean dental changes: 9–10 mm vs. 8.5–12 mm). However, SARME is not without adverse effects. Consistent clinical findings after SARME include widening of the nose, which may be unfavorable in patients with a wide alar base.24 Other iatrogenic problems include facial swelling, sinus infection and severe hemorrhage.2
Minor bone surgery has also been suggested to facilitate arch expansion.1718 Corticotomy-assisted maxillary expansion was first suggested by Lines in 1975.17 This technique included the placement of a buccal incision at the maxillary sinus, combined with splitting of the midpalatal suture, and it resulted in the release of all resistance from the skull complexes. However, the dental and skeletal changes following this procedure were not described. Furthermore, this technique can be difficult for inexperienced surgeons. Recently, Echchadi et al.18 reported a simpler technique using piezo-bone perforations on the buccal alveolar bone for the treatment of maxillary transverse deficiency in a 14-year-old girl. They achieved 8.4–10.6 mm of dental expansion, which is approximately similar to that achieved in our study. In addition, changes in the tooth inclination after treatment were also similar to our results (Table 4). Therefore, we believe that corticotomy can be used to enhance the outcomes of RME in adults.
Alveolar crest resorption may be evident following expansion procedures.252627 The average decrease in the alveolar crest height (Cu-Cr) in our study was 1.8 to 3.15 mm, which is similar to the values in previous studies. Brunetto et al.25 reported that horizontal bone loss of 0.75 to 3.28 mm was observed after 8 mm of expansion in 9-year-old children. Likewise, Rungcharassaeng et al.26 described increased crestal bone loss (2.92–4.42 mm) in 14-year-old children after nonsurgical expansion of 6 mm. In addition, with bone cuts surrounding the maxilla, SARME is believed to release resistance from the maxillary complexes and facilitate expansion in adults. Nevertheless, buccal crest resorption was also reported to increase by 1.5–3.3 mm.27 Although any expansion procedure has the potential to cause root resorption,28 our study showed no evidence of root resorption when assessed using CBCT scans.
According to Chung et al.,1516 when the cortical bone layer is interrupted around a targeted segment, the remaining medullary bone around that segment can be easily displaced by heavy forces. With regard to maxillary expansion, alveolar displacement accounted for a large proportion of the total expansion, varying from 50% in children to 82% in adults. However, in adults, the cortical bone is more rigid; therefore, expansion of the dental arch becomes more difficult with the conventional nonsurgical approach. In the present study, performing adjunctive buccal and palatal corticotomy was aimed at breaking the continuity of the alveolar segment at the basal bone level. As a result, the bony segments could be displaced buccally to compensate for any transverse maxillary deficiency and provide an additional arch perimeter. Because the tooth apices were around the HP level, horizontal incisions on the buccal side were placed slightly higher than the HP level. Under the expansion force, basal bone may act as a fulcrum for outward movement of the alveolar bone. This could be the reason for the increase in the alveolar width at the HP level. Accordingly, our findings supported Chung's theory for expansion of rigid alveolar bone.141516
The recent development of an ultrasonic device allows corticotomy to be performed under local anesthesia. This device provides the advantages of minimal flap elevation for surgery and less pain and associated risks.29 However, the drawback is the device is rather costly.
Our study has provided a new insight regarding the movement of blocks of teeth in the lateral dimension for overcoming dental crossbites and transverse skeletal discrepancies in adults. However, further research should clarify our findings, because the craniofacial skeleton of sheep is evidently different from that of humans. In addition, variations in the rigidity and thickness of the cortical bone may have affected the results of our study. In our research, the intervention was carried out in a short period, hence, we were not able to assess the long-term stability of the procedure in our study. Nevertheless, Chung et al.15 illustrated that fractured bone with adequate mineralization would retain its final deformed shape permanently. Therefore, the remineralized decorticotomy segment is likely to be stable in its new buccal position, and our outcomes are expected to be maintained in the long term.
In adult animal model, buccal and palatal corticotomy assisted maxillary expansion showed combination of skeletal and dental expansion. Dental expansion was approximately 2 and 3 times greater than bony expansion at alveolar crest and hard palate respectively. In summary, adjunctive buccal and palatal corticotomy with RME may be a potential treatment modality for moderate transverse maxillary deficiency in adults. With the advantages of adjunctive corticotomy, compensation treatment can be performed easily. This procedure may also provide an increase in the vestibular region width and widen the smile, proving beneficial in select cases. Furthermore, it may be useful for cases of clefts exhibiting large palatal deficiencies, considering that it may not lead to further enlargement of the defects.
Figures and Tables
Figure 1
Hyrax appliance for rapid maxillary expansion (RME) in a sheep model and placement of corticotomy incisions. A, RME appliance with a Super-Screw® (Great Lakes Orthodontics, Tonawanda, NY, USA) positioned parallel to the midpalatal suture. B, Buccal view showing the corticotomy incision from the mesial aspect of the first premolar to the distal aspect of the third premolar. C, Occlusal view showing the palatal aspect of the corticotomy incision.

Figure 2
Linear skeletal and dental measurements on cone-beam computed tomography images for evaluation of the effects of buccal and palatal corticotomy-assisted rapid maxillary expansion in sheep. A, Alveolar width at the crest level (Cr-Cr level) and hard palate level (HP level) and marginal alveolar bone loss (Cu-Cr). B, Tooth displacement at the cusp level (Cu-Cu), central pulp level (Pu-Pu), and root apex level (R-R), and vertical tooth displacement (Cu-NS).

Figure 3
Superimposition of images acquired before (green) and after (red) buccal and palatal corticotomy-assisted rapid maxillary expansion in sheep using Mimics Software (Materialise NV, Leuven, Belgium). The red part revealed the significant changes after treatment from left side view (A); from occlusal view (B); and from right side view (C); and the mean transverse skeletal (hard palate [HP] and alveolar crest levels) and dental changes (cusp level) in the premolar region (D).

Table 2
Changes in dentoalveolar dimensions in the control group (no treatment) and treatment (buccal and palatal corticotomy + rapid maxillary expansion) group

Values are presented as mean ± standard deviation.
T1, Before treatment; T2, after treatment; P1, first premolar; P2, second premolar; P3, third premolar; M1, first molar.
*Wilcoxon signed-rank test for comparison between T1 and T2 within groups; †Mann-Whitney U-test for comparison between the control and treatment groups.
See Table 1 for the definitions of each measurement.
Table 3
Findings of Kruskal-Wallis test and pairwise comparison for changes in dentoalveolar dimensions at the premolars and molars after buccal and palatal corticotomy + rapid maxillary expansion
H, Results from Kruskal-Wallis H test; df, degree of freedom; M1, first molar; P1, first premolar; P2, second premolar; P3, third premolar.
*p < 0.05.
See Table 1 for the definitions of each measurement.
ACKNOWLEDGEMENTS
This research is supported by the High Impact Research MoE Grant UM.C/625/1/HIR/MoE/Dent21 from the Ministry of Education Malaysia and University of Malaya Postgraduate Research Grant PG275-2016A.
References
1. Northway W. Palatal expansion in adults: the surgical approach. Am J Orthod Dentofacial Orthop. 2011; 140:463. 465. 467 passim.

2. Handelman C. Palatal expansion in adults: the nonsurgical approach. Am J Orthod Dentofacial Orthop. 2011; 140:462. 464. 466 passim.

3. McNamara JA Jr, Baccetti T, Franchi L, Herberger TA. Rapid maxillary expansion followed by fixed appliances: a long-term evaluation of changes in arch dimensions. Angle Orthod. 2003; 73:344–353.
4. Gurel HG, Memili B, Erkan M, Sukurica Y. Long-term effects of rapid maxillary expansion followed by fixed appliances. Angle Orthod. 2010; 80:5–9.

5. Lagravere MO, Major PW, Flores-Mir C. Long-term skeletal changes with rapid maxillary expansion: a systematic review. Angle Orthod. 2005; 75:1046–1052.
6. Suri L, Taneja P. Surgically assisted rapid palatal expansion: a literature review. Am J Orthod Dentofacial Orthop. 2008; 133:290–302.

7. Handelman CS, Wang L, BeGole EA, Haas AJ. Nonsurgical rapid maxillary expansion in adults: report on 47 cases using the Haas expander. Angle Orthod. 2000; 70:129–144.
8. Bishara SE, Staley RN. Maxillary expansion: clinical implications. Am J Orthod Dentofacial Orthop. 1987; 91:3–14.

9. Bassarelli T, Dalstra M, Melsen B. Changes in clinical crown height as a result of transverse expansion of the maxilla in adults. Eur J Orthod. 2005; 27:121–128.

10. Angelieri F, Cevidanes LH, Franchi L, Gonçalves JR, Benavides E, McNamara JA Jr. Midpalatal suture maturation: classification method for individual assessment before rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2013; 144:759–769.

11. Knaup B, Yildizhan F, Wehrbein H. Age-related changes in the midpalatal suture. A histomorphometric study. J Orofac Orthop. 2004; 65:467–474.
12. Korbmacher H, Schilling A, Püschel K, Amling M, Kahl-Nieke B. Age-dependent three-dimensional microcomputed tomography analysis of the human midpalatal suture. J Orofac Orthop. 2007; 68:364–376.

13. Kole H. Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg Oral Med Oral Pathol. 1959; 12:515–529.

14. Choo H, Heo HA, Yoon HJ, Chung KR, Kim SH. Treatment outcome analysis of speedy surgical orthodontics for adults with maxillary protrusion. Am J Orthod Dentofacial Orthop. 2011; 140:e251–e262.

15. Chung KR, Kim SH, Lee BS. Speedy surgical-orthodontic treatment with temporary anchorage devices as an alternative to orthognathic surgery. Am J Orthod Dentofacial Orthop. 2009; 135:787–798.

16. Chung KR, Mitsugi M, Lee BS, Kanno T, Lee W, Kim SH. Speedy surgical orthodontic treatment with skeletal anchorage in adults--sagittal correction and open bite correction. J Oral Maxillofac Surg. 2009; 67:2130–2148.

18. Echchadi ME, Benchikh B, Bellamine M, Kim SH. Corticotomy-assisted rapid maxillary expansion: A novel approach with a 3-year follow-up. Am J Orthod Dentofacial Orthop. 2015; 148:138–153.

19. Charan J, Kantharia ND. How to calculate sample size in animal studies? J Pharmacol Pharmacother. 2013; 4:303–306.

20. Wertz RA. Skeletal and dental changes accompanying rapid midpalatal suture opening. Am J Orthod. 1970; 58:41–66.

21. Cao Y, Zhou Y, Song Y, Vanarsdall RL Jr. Cephalometric study of slow maxillary expansion in adults. Am J Orthod Dentofacial Orthop. 2009; 136:348–354.

22. Lin L, Ahn HW, Kim SJ, Moon SC, Kim SH, Nelson G. Tooth-borne vs bone-borne rapid maxillary expanders in late adolescence. Angle Orthod. 2015; 85:253–262.

23. Lagravère MO, Major PW, Flores-Mir C. Dental and skeletal changes following surgically assisted rapid maxillary expansion. Int J Oral Maxillofac Surg. 2006; 35:481–487.

24. O'Ryan F, Schendel S. Nasal anatomy and maxillary surgery. II. Unfavorable nasolabial esthetics following the Le Fort I osteotomy. Int J Adult Orthodon Orthognath Surg. 1989; 4:75–84.
25. Brunetto M, Andriani Jda S, Ribeiro GL, Locks A, Correa M, Correa LR. Three-dimensional assessment of buccal alveolar bone after rapid and slow maxillary expansion: a clinical trial study. Am J Orthod Dentofacial Orthop. 2013; 143:633–644.

26. Rungcharassaeng K, Caruso JM, Kan JY, Kim J, Taylor G. Factors affecting buccal bone changes of maxillary posterior teeth after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2007; 132:428.e1–428.e8.

27. Gauthier C, Voyer R, Paquette M, Rompré P, Papadakis A. Periodontal effects of surgically assisted rapid palatal expansion evaluated clinically and with cone-beam computerized tomography: 6-month preliminary results. Am J Orthod Dentofacial Orthop. 2011; 139:4 Suppl. S117–S128.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download