Abstract
Background
A stellate ganglion block (SGB) causes increased blood flow in the maxillofacial region, exhibiting the potential for regenerative effects in damaged tissue. The focus of this study was to understand the efficacy of SGB for regenerative effects against nerve damage. A rat model of the superior cervical ganglion block (SCGB) was created instead of SGB, and facial blood flow, as well as sympathetic nervous system function, were measured.
Methods
A vertical incision was made on the left side of the neck of a Wistar rat, and a 5-mm resection of the superior cervical ganglion was performed at the back of the bifurcation of the internal and external branches of the left common carotid artery. Blood flow in the skin at the mandibular angle and mean facial temperature were measured using a laser-Doppler blood flow meter and a thermographic camera, respectively, over a 5-week period after the block. In addition, the degree of ptosis and miosis were assessed over a period of 6 months.
Results
The SCGB rat showed significantly higher blood flow at the mandibular angle on the block side (P < 0.05) for 3 weeks, and significantly higher skin temperature (P < 0.05) for 1 week after the block. In the SCGB rat, ptosis and miosis occurred immediately after the block, and persisted even 6 months later.
Abundant blood flow is essential for the repair of damaged tissue, particularly in cases involving nerve damage where cells show limited regenerative ability. An increase in blood flow can be achieved via dilation of blood vessels, which occurs through the blocking of sympathetic nerves that dominate the damaged area. Sympathetic nerves that dominate the head and neck form ganglions at the lateral region of the spinal column after exiting the spinal cord, and among these, the cervical ganglions fuse with either the first or second thoracic ganglion, producing the stellate ganglion. If the stellate ganglion can be blocked, it is possible that blood flow will increase, as the sympathetic function of the head and neck is also being blocked. Accordingly, a stellate ganglion block (SGB) using local anesthetics is performed to promote the treatment of nerve damage in the head and neck [12345]. However, there is no objective basis for the effectiveness of SGB in repairing tissue damage. Shionoya et el. [6] injected ethanol into the cervical sympathetic ganglion of a beagle to create a canine SGB model that exhibited an increase in blood flow for 6 weeks and an increase in skin temperature for 11 weeks. Similarly, Tsujimoto et el. [7] performed cervical sympathetic ganglion resection in a beagle dog and recorded an increase in blood flow for 6 weeks and an increase in skin temperature for 11 weeks. The authors presumed that an animal model suitable for studying the efficacy of SGB could be obtained if an increase in blood flow could be achieved by blocking the sympathetic ganglion in rats. However, thoracotomy surgery is required to accurately resect the cervical sympathetic ganglion, which is located on the ventral side of the first thoracic vertebra. Therefore, the feasibility of using a superior cervical ganglion block (SCGB), which can be performed using cervical incision only, to increase blood flow by blocking the sympathetic ganglion of the facial area was studied. Based on these considerations, this study aimed to create a rat model of SCGB that could be used to observe sympathetic nervous function and measure changes in blood flow.
Two rats per cage were housed in the animal room of the University facility and given unrestricted access to water and food. The rats were euthanized by intraperitoneal administration of 150 mg/kg pentobarbital sodium after the experiments. This study was conducted in conformance with regulations after obtaining approval from the Animal Experiment Committee of the Nippon Dental University School of Life Dentistry at Tokyo (approval numbers: 11-19).
A male Wistar rat (age, 10–12 weeks; weight, 250–300 g) was administered 50 mg/kg pentobarbital in the abdominal cavity for one week, followed by shaving of the animal's face. Next, the rat was placed in a supine position, and a laser-Doppler blood flow meter (ALF21™, Advance, Tokyo) was set up (Fig. 1) such that its true center aligned with the line dividing the angle between the inferior mandibular border and mandibular ramus plane into 2 equal angles. Following a 20-min rest period, the mean blood flow in the mandibular angle skin of the rat was measured for 5 min using the laser-Doppler blood flow meter. The obtained data were recorded at 1/100 s using an A/D converter (OMEGALAB-8™, OMEGAWAVE, Tokyo).
Three images were captured, one each in the frontal, left lateral, and right lateral orientations, using a thermographic camera (Thermo GEAR G100™, NEC Avio, Tokyo), yielding thermal images with a temperature resolution of 0.08℃. The frontal image was captured in the prone position, the lateral images were captured in a lateral decubitus position, and all images were captured from a distance of 15 cm. Using lateral thermography, the mean temperature on one side of the face excluding the ear and eye was calculated with thermal image analysis software (Infree Analyzer NS9500 Standard™, NEC Avio, Tokyo). The images were captured at room temperature (23℃ ± 1℃) and a humidity of 50% ± 10% respectively.
Three days after obtaining the baseline measurements, 50 mg/kg pentobarbital was administered into the abdominal cavity of the rat. After disinfecting the left cervical area with alcohol, a vertical skin incision was made. Next, using an actual microscope, the sheath around the bifurcation of the common left carotid artery into the internal and external branches was peeled and exposed. A 5-mm resection of the superior cervical ganglion on the back was performed to create a rat model of SCGB. For comparison, a sham rat was created with only the cervical incision.
Blood flow and skin temperature were measured after following administration of 50 mg/kg pentobarbital into the abdominal cavity. The measurements were obtained 3 days after SCGB, 1 week later, and then once each week for 5 weeks. As for assessments of Horner syndrome, the degree of ptosis and miosis was determined each month for 6 months as follows:
The blood flow in the mandibular angle increased after SCGB, reaching a maximum value 1 week later. Significant differences were observed between the blood flow in the SCGB and sham rats until 3 weeks after the block (Fig. 2).
The skin temperature increased after SCGB, reaching a maximum value 1 week later. Significant differences were observed between the skin temperature in the SCGB and sham rats until 1 week after the block (Fig. 3a, 3b; Fig. 4a, 4b; Fig. 5).
In general, restoration of damaged tissue requires abundant blood flow to the damaged region. In particular, increasing the blood flow in surrounding areas is considered to be an effective approach for cases involving nerve damage, where the cells have limited regeneration capability and there is no effective treatment [89]. Accordingly, SGB is often used for the treatment of cervical nerve damage, but there has been no objective study of its efficacy. One reason for the lack of objective data is the time required to increase the blood flow using local anesthetics (about 30–60 min), which necessitates the application of at least 1–2 blocks per day to confirm SGB efficacy. In addition, frequent insertion of block needles to the cervical spine of animals is considered technically difficult. Therefore, Shionoya et al. [6] damaged the cervical sympathetic ganglion in a beagle dog using alcohol, and created a canine SGB model that exhibited a blood flow increase for 7 weeks and an increase in skin temperature for 10 weeks. However, a large experimental setup is required for conducting tests with dogs, and the resultant higher experimental costs can make data collectiondifficult. Accordingly, this study aimed to create an SGB model using rats. However, permeation of alcohol is likely to cause significant damage to the surrounding tissue in rats. Therefore, on the basis of the method proposed by Tsujimoto et al. [7], ganglion resection was considered. However, accurate resection of the stellate ganglion located towards the back of the first thoracic vertebra would necessitate thoracotomy surgery, making the procedure extremely invasive for rats. In humans, since a superior or middle ganglion block is clinically termed as SGB, it was presumed that an SCGB in rats, which can be achieved by cervical incision only, could be a good model for SGB. The results revealed that SCGB increased blood flow in the left mandibular angle, which was on the same side as the block, for about 3 weeks after the block. Moreover, the skin temperature, which reflects blood flow, also increased for about 1 week after the block. The results clearly indicate that it is possible to increase blood flow over a long period of time using a superior ganglion resection (block) in rats.
However, the increase in blood flow and skin temperature was not persistent. Tsujimoto et al. [7] also reported that the SCGB-induced increase in blood flow to the oral mucosa in dogs settled back to the pre-block level after about 7 weeks. One reason cited for this finding was that the blood flow may have shifted from the block side to the non-block side due to dilation of the collateral vessels. Moreover, Kakuyama et al. [10] reported that the sympathetic ganglion is also dominated by the opposite side. In this study, it is likely that the dominance by the non-block side progressed with time, resulting in restoration of sympathetic nerve function and a consequent constriction of blood vessels. Since the speed of angiogenesis in animals is constant regardless of the species, and the total area of blood vessels running through the mandibular angle is smaller in rats compared to dogs, the shorter period for return of blood flow and skin temperature to the pre-block levels in rats in comparison with that in dogs was presumed to be attributable to the reduced time required for reconstruction of blood vessels in rats. Accordingly, it was considered difficult to persistently increase cervical blood flow using SCGB.
Horner syndrome refers to the ocular depression, miosis, and ptosis that occur due to impairment of the sympathetic nervous system function around the eyeball [11], and it is used clinically to judge the efficacy of SGB. Although, SCGB in this study was considered useful for creating an SGB model because ptosis and miosis were confirmed immediately after the block, and unlike the short-term changes noted in blood flow and skin temperature, the ptosis and miosis persisted even after 6 months. This indicates that dysfunction of the levator palpebrae superioris muscle and iris dilator muscle, which are dominated by the sympathetic nervous system, was sustained. Accordingly, it was presumed that the sympathetic nerve block continued on the blocked cervical side even 6 months after the procedure. Based on these observations, restoration of blood flow does not clearly indicate restoration of sympathetic nervous function.
One limitation of this study is that in comparison with SGB, which needs intermittent local anesthetic administration, resection of the superior cervical stellate ganglion persistently blocks the sympathetic nervous system, and induces an increase in blood flow over a longer duration. As a result, it can be implied from this study that SCGB has a greater effect on nerve regeneration than SGB. However, this was considered to be a suitable experimental model for studying the effect of an increase in blood flow on tissue regeneration. In conclusion, the results clearly showed that a sympathetic nervous block performed using SCGB in rats could result in a blood flow increase for about 3 weeks.
Figures and Tables
 | Fig. 1Probe position of blood flow meter.Probe was put on the center of the inferior mandibular border and mandibular ramus plane angle. white circle: blood flow probe.
|
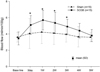 | Fig. 2Changes in blood flow. Blood flow significantly increased for 3 weeks after the block. * P<0.05: significant differences between two groups. |
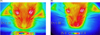 | Fig. 3Observation by thermography (front view). (A) Before Superior cervical ganglion block (SCGB) (B) One week after SCGB. Skin temperature increased on the block side (left). |
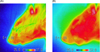 | Fig. 4Observation by thermography (left side view). (A) Before Superior cervical ganglion block (SCGB) (B) One week after SCGB. Skin temperature increased on the block side (left). |
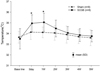 | Fig. 5Changes in skin temperature. Skin temperature significantly increased for 1 week after the block. * P<0.05: significant differences between two groups. |
References
1. Salvaggio I, Adducci E, Dell'Aquila L, Rinaldi S, Marini M, Zappia L, et al. Facial pain: a possible therapy with stellate ganglion block. Pain Med. 2008; 9:958–962.

2. Milligan NS, Nash TP. Treatment of post-herpetic neuralgia. a review of 77 consecutive cases. Pain. 1985; 23:381–386.

3. Melis M, Zawawi K, al-Badawi E, Lobo S, Mehta N. Complex regional pain syndrome in the head and neck: a review of the literature. J Orofac Pain. 2002; 16:93–104.
4. Lynch ME, Elgeneidy AK. The role of sympathetic activity in neuropathic orofacial pain. J Orofac Pain. 1996; 10:297–305.
5. Kohjitani A, Miyawaki T, Kasuya K, Shimada M. Sympathetic activity-mediated neuropathic facial pain following simple tooth extraction: a case report. Cranio. 2002; 20:135–138.

6. Shionoya Y, Sunada K, Shigeno K, Nakada A, Honda M, Nakamura T. Can nerve regeneration on an artificial nerve conduit be enhanced by ethanol-induced cervical sympathetic ganglion block? PLoS One. 2017; 12:e0189297.

7. Tsujimoto G, Sunada K, Nakamura T. Effect of cervical sympathetic ganglionectomy on facial nerve reconstruction using polyglycolic acid-collagen tubes. Brain Res. 2017; 1669:79–88.

8. de la Torre JC, Goldsmith HS. Increased blood flow enhances axon regeneration after spinal transection. Neurosci Lett. 1988; 94:269–273.

9. Haapaniemi T, Nylander G, Kanje M, Dahlin L. Hyperbaric oxygen treatment enhances regeneration of the rat sciatic nerve. Exp Neurol. 1998; 149:433–438.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download