This article has been
cited by other articles in ScienceCentral.
Abstract
Background
To describe the clinical and magnetic resonance imaging findings of ganglion cysts with effusion in the flexor hallucis longus tendon sheath around the hallux to evaluate their origin.
Methods
Patients with recurrent or painful ganglion cysts around the hallux with effusion in the flexor hallucis longus tendon sheath who underwent surgical treatment at St. Vincent's Hospital from February 2007 to August 2016 were investigated. Surgical indication was a painful or recurrent mass caused by the cystic lesions. Those without effusion of the flexor hallucis longus tendon sheath were excluded. We assessed the clinical and magnetic resonance imaging findings.
Results
Magnetic resonance imaging findings in all patients showed several ganglion cysts around the hallux and large fluid accumulations within the flexor hallucis longus tendon sheath. Regarding the location, six ganglion cysts were on the dorsomedial aspect, one on the plantar medial aspect, seven on the plantar lateral aspect, and one in the toe pulp. Ten patients showed joint effusions in both the metatarsophalangeal and interphalangeal joints, two in the metatarsophalangeal joints, and three in the interphalangeal joints. There were communication stalks with a tail shape or abutment between ganglion cysts with surrounding joint effusions. Intraoperatively, connections between ganglion cysts, the synovial cyst of the flexor hallucis longus tendon sheath, and surrounding joints were seen.
Conclusions
Synovial fluid accumulation in the metatarsophalangeal or interphalangeal joint supplies the synovial cyst of the flexor hallucis longus tendon sheath and subsequently ganglion cysts in the hallux. In clinical practice, the surgeon should carefully check surrounding joints with tendon sheaths to prevent recurrence of the ganglion cysts around the hallux.
Go to :

Keywords: Hallux, Ganglion cysts, Recurrence
Ganglion cysts are benign fluid-filled masses that can arise from joint capsules, tendon sheaths, and bursae.
1) They are the most common soft tissue masses in the wrist, foot, and ankle
23) and usually asymptomatic. Ganglion cysts of the toes comprise 6.6% of all ganglia.
4) Patients with ganglion cysts around the hallux usually complain of pain due to a mass effect within shoes and pressure during ambulation.
5) Primary treatment of ganglion cysts is conservative, primarily aspiration,
67) but the recurrence rate after nonoperative treatment is reportedly as high as 33%–62%.
68) Therefore, surgery is the preferred method of treatment, especially in patients with a painful or recurrent ganglion cyst after repeated procedures.
8)
The ganglion around the hallux sometimes resists even surgical treatment, and surgical procedures may need to be repeated several times.
6) Careful preoperative evaluation including magnetic resonance imaging (MRI) is needed due to the high recurrence rate after incomplete surgical excision.
6) However, there are few articles describing the MRI findings of ganglion cysts around the hallux.
910)
In the past, we discovered that some ganglion cysts around the hallux were connected to the synovial cyst in the flexor hallucis longus (FHL) tendon sheath. In most cases of synovial cysts of the FHL, we also found associated effusions in the interphalangeal (IP) and metatarsophalangeal (MTP) joints. We hypothesized that these findings might be associated with the frequent recurrence after simple aspiration or excision of the ganglion around the hallux. The aim of the present study was to describe the clinical and MRI findings of ganglion cysts with a synovial cyst of the FHL tendon around the hallux in order to evaluate their origin.
METHODS
This study was approved by the Institutional Review Board at St. Vincent's Hospital and requirement for informed consent was waived. The study design was a retrospective review. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee. Patients with ganglion cysts around the hallux and effusion in the FHL tendon sheath who underwent surgical treatment at our university hospital from February 2007 to August 2016 were included in the study. The surgical indication was a painful or recurrent mass due to the cystic lesions. Exclusion criteria for this study were ineligibility for MRI preoperatively, less than 12 months of interval between the operation and final follow-up, and absence of a synovial cyst of the FHL tendon sheath on MRI.
Radiological evaluation included the location of the ganglion cysts around the hallux and effusion in the FHL tendon sheath, effusion in the IP or MTP joint of the hallux, and identification of a communication stalk between the ganglion cysts around the hallux, the synovial cyst of FHL tendon sheath, and effusion in the IP and MTP joints. Effusion of the joint was defined as relatively larger amount of fluid compared to the other joints of the same foot on MRI.
Follow-up period was defined as the interval from the final surgery to the last follow-up. Functional outcomes were evaluated by the American Orthopaedic Foot and Ankle Society (AOFAS) Hallux Metatarsophalangeal-Interphalangeal Scale. Patients were scored 0 to 100 according to patient-specific outcomes and classified as excellent, good, fair, and poor final outcome groups.
Operation
For surgical treatment, a pneumatic tourniquet was applied to the proximal thigh in all cases in order to control bleeding. Loupe magnification was used for better dissection of adherent cutaneous nerve branches from the lesions and identification of communication stalks. A longitudinal skin incision was made over the plantar aspect of the hallux and forefoot around the IP and MTP joints. Once the FHL tendon sheath was open, synovial fluid gushed out from the cyst of the FHL tendon sheath. The A2 pulley in the hallux was protected as much as possible. When a pulley was released, it was repaired. When synovial proliferation was found, partial synovectomy was done from the inner layer of the FHL tendon sheath. It was not necessary to remove the ganglion cyst of the hallux completely. Next, if communication stalks between the tendon sheath of the FHL and the IP or MTP joint were identified, they were widened. Patients were allowed partial weight-bearing for 1 week after the surgery, with activities increased as tolerated thereafter.
Go to :

RESULTS
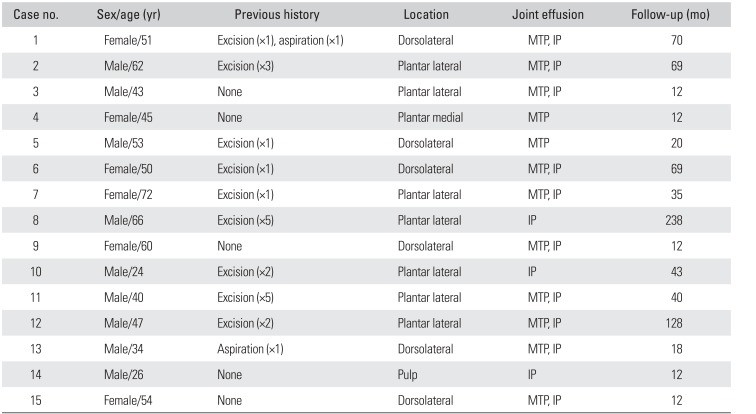
In all, 15 patients were identified (
Table 1). There were nine males and six females. Patients' ages ranged from 24 to 72 years, with a median age of 52.5 years. The median period of follow-up was 35 months (range, 1 to 12 years). The chief complaints were a painful mass in five patients and a recurrent mass in 10. The time interval between symptom onset and the excision varied from 1 month to 18 years with a median of 18 months. For preceding treatments, nine patients underwent surgical excision and two underwent aspiration. The median number of previous surgical treatments in recurrent cases was one, and two patients had more than five previous surgical treatments for recurrence of painful masses. Drainage sinuses from ganglion cysts were placed in three patients preoperatively, but no skin problems occurred postoperatively.
Table 1
Patient Information
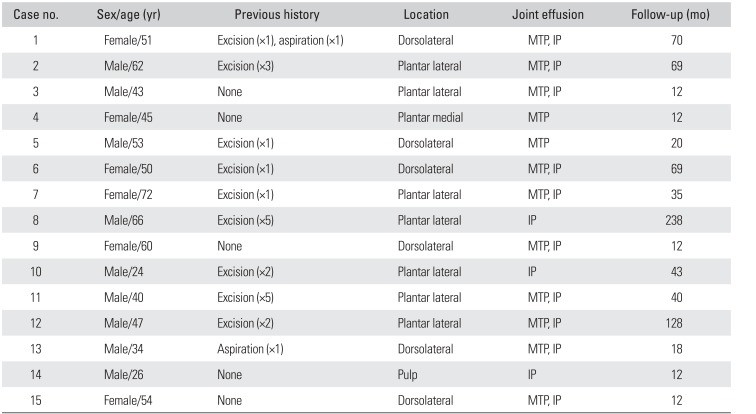
|
Case no. |
Sex/age (yr) |
Previous history |
Location |
Joint effusion |
Follow-up (mo) |
|
1 |
Female/51 |
Excision (×1), aspiration (×1) |
Dorsolateral |
MTP, IP |
70 |
|
2 |
Male/62 |
Excision (×3) |
Plantar lateral |
MTP, IP |
69 |
|
3 |
Male/43 |
None |
Plantar lateral |
MTP, IP |
12 |
|
4 |
Female/45 |
None |
Plantar medial |
MTP |
12 |
|
5 |
Male/53 |
Excision (×1) |
Dorsolateral |
MTP |
20 |
|
6 |
Female/50 |
Excision (×1) |
Dorsolateral |
MTP, IP |
69 |
|
7 |
Female/72 |
Excision (×1) |
Plantar lateral |
MTP, IP |
35 |
|
8 |
Male/66 |
Excision (×5) |
Plantar lateral |
IP |
238 |
|
9 |
Female/60 |
None |
Dorsolateral |
MTP, IP |
12 |
|
10 |
Male/24 |
Excision (×2) |
Plantar lateral |
IP |
43 |
|
11 |
Male/40 |
Excision (×5) |
Plantar lateral |
MTP, IP |
40 |
|
12 |
Male/47 |
Excision (×2) |
Plantar lateral |
MTP, IP |
128 |
|
13 |
Male/34 |
Aspiration (×1) |
Dorsolateral |
MTP, IP |
18 |
|
14 |
Male/26 |
None |
Pulp |
IP |
12 |
|
15 |
Female/54 |
None |
Dorsolateral |
MTP, IP |
12 |

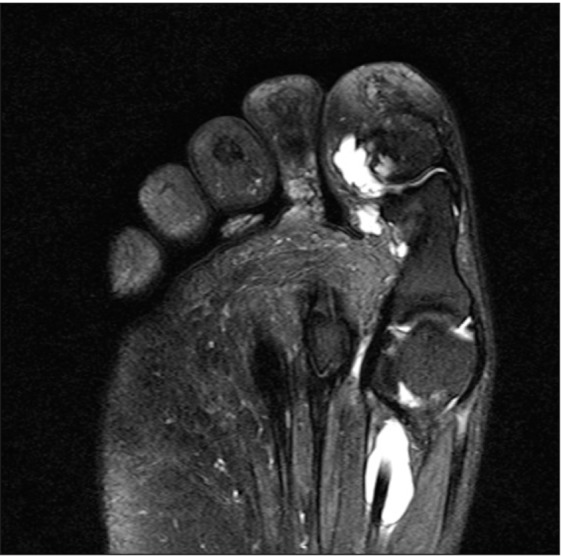
Six lesions were primarily on the dorsolateral aspect, seven on the plantar lateral aspect, one on the planter medial aspect, and one in the toe pulp. On MRI, multilobulated ganglion cysts were found around the hallux, and there was a large fluid accumulation within the synovial sheath of the FHL in all patients (
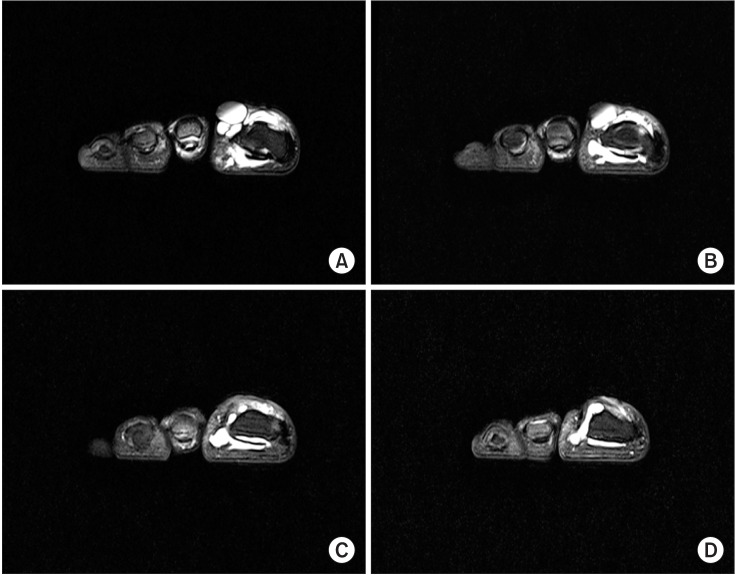
Fig. 1). No patients showed effusion in the extensor hallucis longus tendon sheath. Ten patients showed joint effusions in both the MTP and IP joints, two only in the MTP joint, and three only in the IP joint. There were communication stalks between the cyst of the FHL tendon sheath and the surrounding joints with effusion in all patients (
Fig. 2).
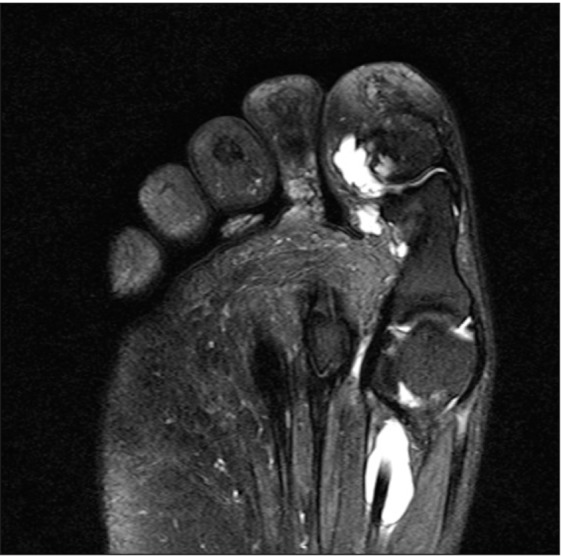 | Fig. 1A 62-year-old male with ganglion cyst around the hallux. On axial view magnetic resonance imaging, ganglion cysts around the hallux had communicating stalks with the interphalangeal joint, and there was a large fluid accumulation within the synovial sheath of the flexor hallucis longus. This patient also had a joint effusion in both the metatarsophalangeal and interphalangeal joints.
|
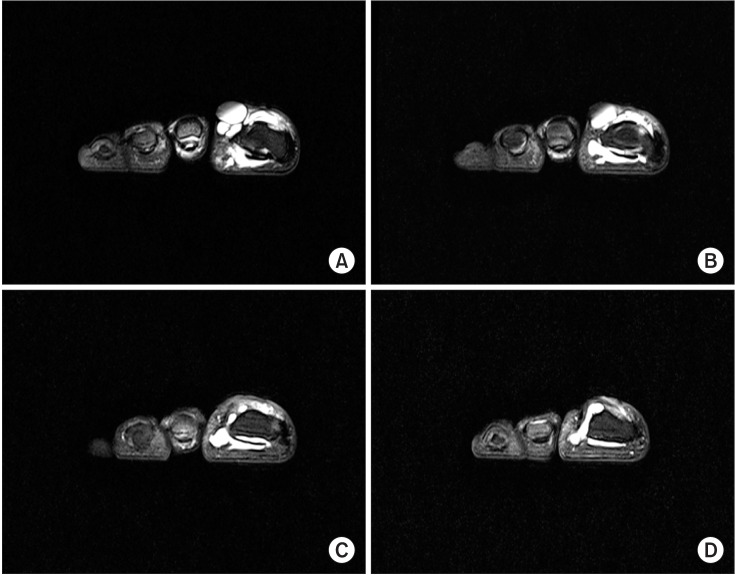 | Fig. 2A 50-year-old female with ganglion cyst around the hallux. (A) On coronal view magnetic resonance imaging, multiple ganglion cysts were seen around the hallux, and the flexor hallucis longus (FHL) tendon sheath was connected to the surrounding metatarsophalangeal joint. (B) A large fluid accumulation was seen within the synovial sheath of the FHL. (C) There were communication stalks between the cyst of the FHL tendon sheath and the surrounding interphalangeal joint. (D) A large fluid accumulation was seen around the hallux.
|
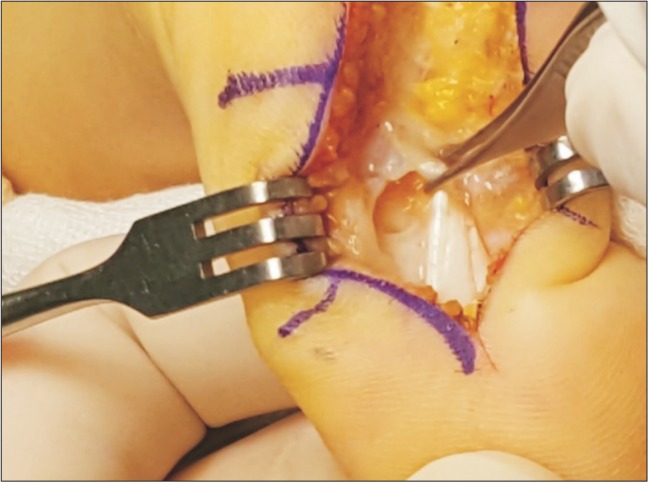
Intraoperatively, there were large effusions within the tendon sheath of the FHL in all patients.
11) In all cases, the ganglion cysts around the hallux were connected to the synovial cyst in the FHL tendon sheath. Because we had made this assumption, we squeezed the ganglion cyst of the hallux, which enhanced the complete evacuation of fluid from the ganglion cysts into the synovial sheath of FHL. Because the FHL tendon sheath was also connected to the surrounding MTP or IP joint in all cases, the stalk was enlarged to drain the cystic fluid completely (
Fig. 3). No recurrence developed in all patients. The median postoperative AOFAS score was 87 points (good; range, 70 to 100 points).
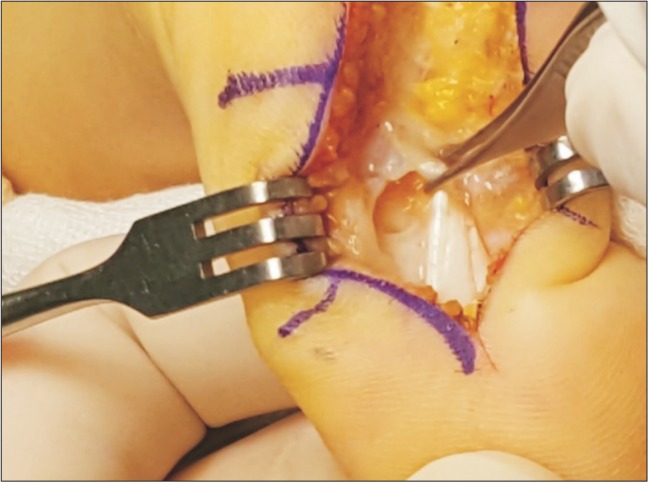 | Fig. 3A 54-year-old female with ganglion cyst around the hallux. Intraoperatively, there were communication stalks between the cyst of the flexor hallucis longus tendon sheath and the surrounding joints.
|
Go to :

DISCUSSION
There are a limited number of articles dealing specifically with ganglion cysts of the hallux
910121314) and even fewer addressing the management of recurrent ganglia.
5151617) Some authors have proposed that recurrence may occur because the cystic structure has been incorporated into the surrounding tissue in a complex manner and resecting it
en bloc may be difficult.
810) In particular, the main body of the pulp ganglia is often found at the side of the distal end of the FHL tendon sheath, and it is not easy to establish an adequate drainage for it, which could lead to a high recurrence rate.
18) Some authors have also suggested that the recurrence rate may be underestimated because recurrence of small deep-seated ganglion may be missed.
18) However, there are no reports regarding a connection between cysts of tendon sheaths and surrounding joints. High rates of recurrence have been reported to be attributable to incomplete operative excision.
219) One study suggested that the joint capsule or tendon sheath adjacent to the ganglion sac should be resected to allow adequate internal drainage,
18) but a ganglion stalk was identified in 6% of cases in their study.
We focused on ganglion cysts around the hallux with synovial cysts of the FHL tendon sheath. Two reports described a high T2 curvilinear channel or “tail” that may extend between the ganglion cyst and surrounding joint on MRI.
2021) On careful evaluation of the MRI, synovial effusion in the MTP or IP joint can be observed as well as a communicating stalk. In the previous literature, the development of a synovial cyst of the FHL tendon sheath was thought to be preceded by mucoid degeneration of the tendon's collagen fibers and cellular hyperplasia associated with active mucin secretion.
11) In our study, ganglion cysts around the hallux were connected to synovial cysts in the FHL tendon sheath originating from the IP or MTP joint. We believe this clinical finding suggests that ganglion cysts around the hallux do not originate by degeneration or hyperplasia but by fluid from surrounding joints. Considering their source of origin, we named the ganglion cysts around the hallux as satellite ganglion cysts.
Possible causes of these connections are increased intra-articular pressure secondary to joint injury or increased pressure due to repetitive trauma.
10) The hallux is constantly under pressure because of weight bearing it is exposed to, and the communication opening acts as a check-valve.
10) Thus, the intracystic fluid cannot return to the intra-articular space or tendon sheath.
10) In this study, the bases of the ganglion cysts were located on the plantar aspect in most cases. Moreover, a communication stalk between the FHL tendon sheath and the surrounding joint was found on the plantar aspect in all cases. It is possible these are the results of a plantar pressure mechanism, which can make satellite ganglion cysts migrate in various directions. As a result, aspiration or excision of only the satellite lesion of the hallux does not appear to be adequate to prevent recurrence. In clinical practice, the surgeon should carefully check surrounding joints with tendon sheaths to prevent recurrence of the ganglion cysts around the hallux.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download