This article has been
cited by other articles in ScienceCentral.
Abstract
Background
The purpose of this study was to determine whether there is a learning curve for internal fixation for nondisplaced femoral neck fractures using the cumulative sum (CUSUM) technique. We applied the CUSUM technique in monitoring performance of a single surgeon in internal fixation for nondisplaced femoral neck fractures.
Methods
Fifty consecutive patients who underwent internal fixation for nondisplaced femoral neck fractures were evaluated retrospectively. Loss of fixation within 6 months postoperatively was considered as failure of treatment. Patients were stratified into the early experience group (cases 1 to 25) and the late experience group (cases 26 to 50). The CUSUM method was used to analyze the learning curve.
Results
There was no failure of treatment during study period. The operation time became shorter with experience. Using the CUSUM analysis to plot the learning curve, there was no significant learning curve observed for multiple pinning for nondisplaced femoral neck fractures.
Conclusions
The CUSUM analysis revealed there was no obvious learning curve to become proficient at internal fixation for nondisplaced femoral neck fractures, if technical principles were followed during the procedure.
Go to :

Keywords: Femur neck, Femoral neck fractures, Fracture fixation, Learning curve
Although internal fixation has been the treatment of choice for nondisplaced femoral neck fractures, there have been concerns, mainly regarding reoperation due to nonunion or osteonecrosis of the femoral head. The reported incidence of nonunion was about 5%, and that of avascular necrosis was about 3%.
12) Bone quality and age have been known as risk factors associated with reoperation for these complications.
3) However, the impact of surgeon's technical skills on the outcome of internal fixation of nondisplaced femoral neck fractures has been rarely known in terms of learning curve.
Evaluation of a learning curve for a surgical procedure has been conventionally based on the measurement of operation time, hospital stay or proportion of procedure-related complications.
4) However, this method involves arbitrary selection of such parameters and is based on the number of procedures performed rather than surgical outcomes. The cumulative sum (CUSUM) analysis, which has been used for quality control in industry, is a more robust and objective method to evaluate whether there is a learning curve for a surgical procedure based on the outcome of consecutive performances with standard reference.
56)
Therefore, the purpose of this study was to determine (1) the proportion of fixation failure within 6 months after internal fixation for nondisplaced femoral neck fractures and (2) the presence of a learning curve for this procedure in one surgeon using the CUSUM analysis.
METHODS
We conducted this study in compliance with the principle of the Declaration of Helsinki. The design and protocol of this retrospective study were approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. B-1111/140-111), and informed consent was waived. Fifty consecutive internal fixations were performed for nondisplaced femoral neck fractures by a single surgeon (YKL) at our institution between September 2009 and November 2011. The surgeon had fellowship experience of 1 year for hip surgery in a tertiary teaching hospital.
All internal fixations using multiple cannulated screws were performed via a standard basic technique. The patients were placed in a supine position on a fracture table. Screw fixation was performed in situ without reduction in all patients. All procedures were performed by the surgeon using the lateral approach. Guide pins were inserted under an image intensifier through the lateral cortex in an inverted triangle shape. The distal guide pin was placed parallel to the femoral neck, resting against the femoral calcar, and the proximal posterior and anterior guide pins parallel to it and just within the cortical bone of the femoral neck. Then, three cannulated screws (6.5 mm stainless steel AO screw; Synthes, Solothurn, Switzerland) were sequentially inserted, and the screw tip was placed into the subchondral area of the femoral head. Immediately postoperatively, range of motion of the hip was permitted as tolerated, and wheelchair ambulation was started from 2 or 3 days postoperatively. Weight bearing was not allowed till 6 weeks postoperatively.
Follow-up evaluations were performed at 6 weeks and 3, 6, 9, and 12 months postoperatively, and every year thereafter. Some patients who were unable to return for a follow-up evaluation were asked to complete a telephone questionnaire and send recent follow-up radiographs. Radiographic evaluation was done by two independent observers who did not participate in the operation. The serial radiographic evaluation included an assessment of loss of fixation, which was defined as a change in fracture position by > 10 mm or in screw position by > 5%, backing of the screws by > 20 mm, or perforation of the femoral head by the screw at the 6-month follow-up.
7)
Statistical Analysis
Data are reported as mean ± standard deviation. Patients were stratified into the early experience group (cases 1 to 25) and the late experience group (cases 26 to 50) to determine whether the level of experience affected the failure rate. A two-tailed chi-square test was used to determine whether there was a statistically significant difference in the failure rate between these two groups. A p-value < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA).
CUSUM Analysis
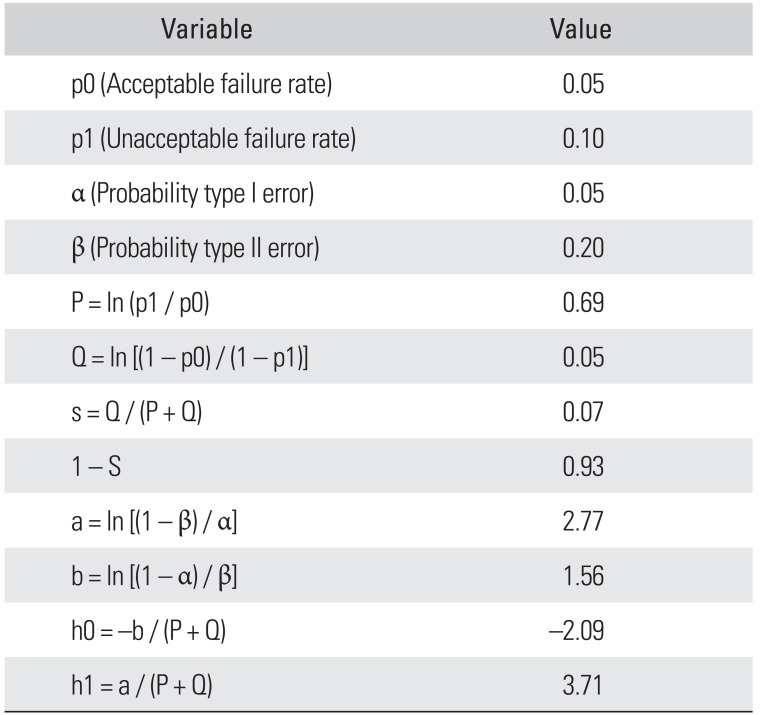
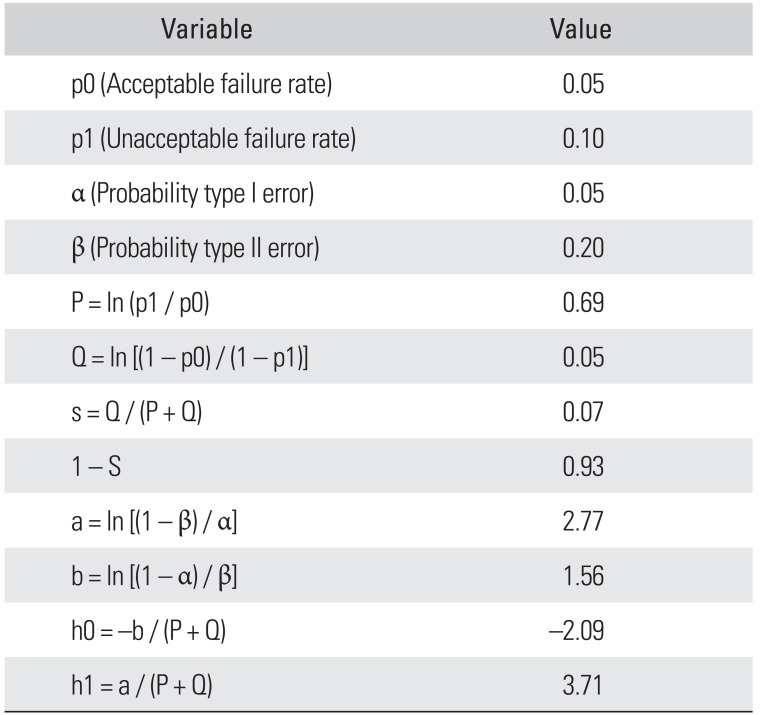
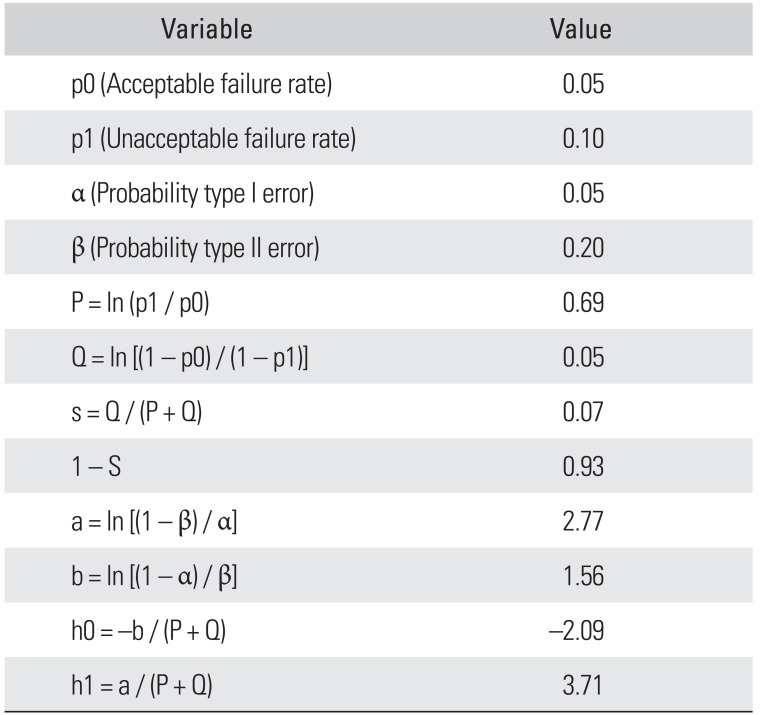
To perform a CUSUM analysis, four parameters were defined: acceptable failure rate, unacceptable failure rate, type I error rate, and type II error rate. Based on the available literature,
8) the acceptable failure rate after internal fixation for femoral neck fractures was determined as 5% and the unacceptable failure rate as 10%. The probabilities of type I and type II (α and β) errors were set at 0.05 and 0.20, respectively. From these, two decision limits (h0 and h1) and the constant s were calculated using the formulas presented in
Table 1.
Table 1
CUSUM Equations and Variables Used to Construct a CUSUM Chart
|
Variable |
Value |
|
p0 (Acceptable failure rate) |
0.05 |
|
p1 (Unacceptable failure rate) |
0.10 |
|
α (Probability type I error) |
0.05 |
|
β (Probability type II error) |
0.20 |
|
P = ln (p1 / p0) |
0.69 |
|
Q = ln [(1 – p0) / (1 – p1)] |
0.05 |
|
s = Q / (P + Q) |
0.07 |
|
1 – S |
0.93 |
|
a = ln [(1 – β) / α] |
2.77 |
|
b = ln [(1 – α) / β] |
1.56 |
|
h0 = −b / (P + Q) |
−2.09 |
|
h1 = a / (P + Q) |
3.71 |

In a CUSUM curve, each case is plotted in sequence along the X-axis. When a failure occurs, 1 − s is added to the CUSUM. When a success occurs (no failure), the constant s is subtracted from the cumulative score. Thus, an ascending trend in the CUSUM line indicates failure, whereas a descending trend indicates success. If the line crosses the upper decision limit (h1) from below, this indicates that the actual failure rate is equal to the unacceptable recurrence rate with the probability of type I error of 0.05. If the line crosses the lower decision limit (h0) from above, this indicates that the actual failure rate does not differ from the acceptable failure rate with the probability of type II error of 0.20. When the line is between h1 and h0, no statistical inference can be made.
9)
Go to :

RESULTS
A total of 50 internal fixations were performed by the same surgeon in the study period. There were 43 Garden type I incomplete fractures, and 7 type II complete fractures without displacement.
10) One patient had died during hospitalization, and the other 49 patients were followed for more than 6 months postoperatively.
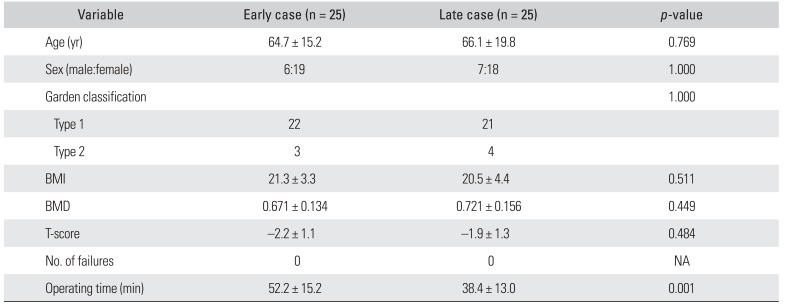
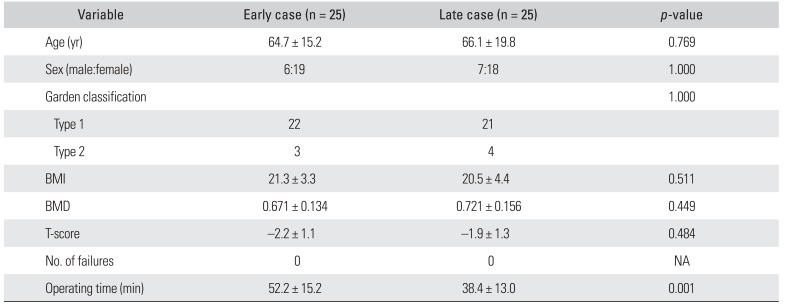
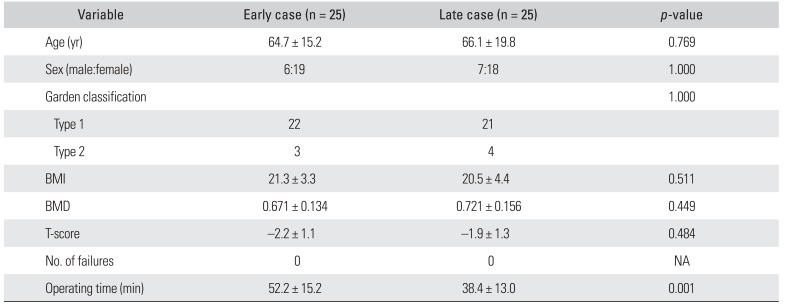
There was no loss of fixation within 6 postoperative months. Patient demographics are listed in
Table 2. There were no statistically significant differences in demographics between the early experience group (first 25 cases) and the late experience group (
Table 2). But, the operation time was shorter in the late experience group (
p = 0.001).
Table 2
Patient Characteristics
|
Variable |
Early case (n = 25) |
Late case (n = 25) |
p-value |
|
Age (yr) |
64.7 ± 15.2 |
66.1 ± 19.8 |
0.769 |
|
Sex (male:female) |
6:19 |
7:18 |
1.000 |
|
Garden classification |
|
|
1.000 |
|
Type 1 |
22 |
21 |
|
|
Type 2 |
3 |
4 |
|
|
BMI |
21.3 ± 3.3 |
20.5 ± 4.4 |
0.511 |
|
BMD |
0.671 ± 0.134 |
0.721 ± 0.156 |
0.449 |
|
T-score |
−2.2 ± 1.1 |
−1.9 ± 1.3 |
0.484 |
|
No. of failures |
0 |
0 |
NA |
|
Operating time (min) |
52.2 ± 15.2 |
38.4 ± 13.0 |
0.001 |

Fig. 1 shows the CUSUM chart indicating that there is no significant learning curve for internal fixation for nondisplaced femoral neck fractures. At point A (case 30), the line crosses the lower decision limit and the failure rate is equal to the defined acceptable failure rate (5%) with a probability of type II error of 0.20. Also, the failure rate does not reach the unacceptable threshold at any time.
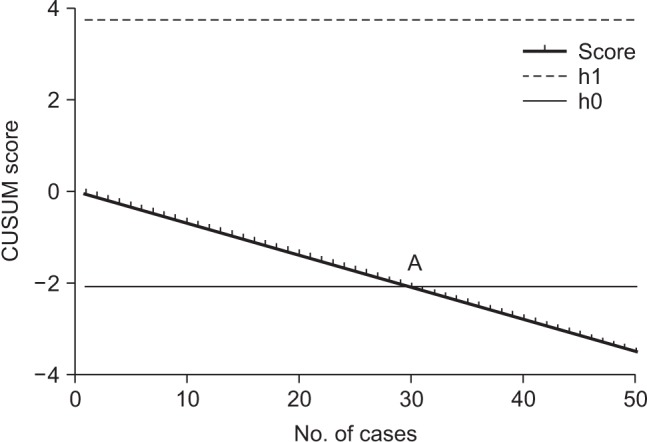 | Fig. 1Cumulative sum (CUSUM) chart for internal fixation for nondisplaced femoral neck fractures. Point A (case 30) represents the point where the failure rate is not significantly different from the acceptable recurrence rate. At no point does the line cross the upper decision limit (h1).
|
Go to :

DISCUSSION
The purpose of this study was to assess the learning curve for performing multiple pinning for nondisplaced femoral neck fractures, using radiological loss of fixation at 6 months postoperatively as the main outcome measure. Using the CUSUM analysis to plot the learning curve, we found a steady improvement without loss of fixation from case 1. At case 30, the actual failure rate was not statistically different from the acceptable failure rate (5%).
To our knowledge, our study is the first to demonstrate whether there is a learning curve for internal fixation for nondisplaced femoral neck fractures. On the basis of the experience of the single surgeon, we think there is no significant learning curve for the procedure and the operation time decreases with experience.
CUSUM analysis has been applied to medical procedures, such as laparoscopic surgery,
1112) organ transplantation,
13) ophthalmologic surgery,
9) and anesthetic procedures.
14) CUSUM analysis is a useful tool that allows surgeons to monitor any type of surgical performance with a binary outcome. Furthermore, the graphic display of a CUSUM chart is simple and easy to understand. An upward trend indicates unacceptable performance; when it happens, careful review and intervention of the performed procedure are advised.
56)
There are several limitations in this study. First, our analysis presents the learning curve of a single surgeon with a relatively small sample size of 50 patients. However, CUSUM analysis is a sensitive method that allows one to work with an unknown and increasing sample size. Second, we did not include displaced femoral neck fractures, in which reduction is technically more demanding. However, arthroplasty has been usually favored in patients with displaced femoral neck fractures because results of internal fixation has been worse than arthroplasty,
1516) and our purpose was to determine whether there would be a learning curve for internal fixation for nondisplaced femoral neck fractures. Third, our analysis did not include long-term results after surgery.
In spite of these limitations, our findings suggest that there is no obvious learning curve to become proficient at multiple pinning, if surgical principles are followed during the procedure.
Go to :