Abstract
Background
The purpose of the current study is to investigate anatomical relationships between the muscle overlying the distal transverse carpal ligament (TCL) and the thenar motor branch of the median nerve.
Methods
Of the 192 wrists that underwent open carpal tunnel release, a muscle belly overlying the TCL was observed on the distal margin of TCL in 25 wrists and ligament exposure could not be achieved without transection of it. We recorded surgical findings of these 25 wrists. The origin of the recurrent motor branch arising from the major median nerve was marked on the axial and coronal section diagrams of the wrist.
Results
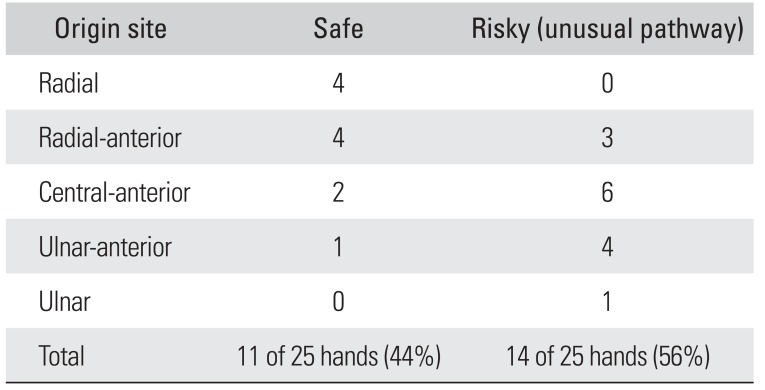
The presence of muscle overlying the TCL was seen in 25 wrists (21 patients, 13%). The locations of origin were distributed not only on the radial side but anterior or ulnar side of the major median nerve. Abnormal branches originated from the unusual side in 14 cases (56% of those with a muscle overlying the TCL): central-anterior side in eight cases, ulnar-anterior side in five cases, and ulnar side in one case. These anomalous branches were frequently associated with the muscle belly overlying the TCL in our study regardless of the origin site. The branches were prone to cut if careless midline incision along the third web space was performed. Unusual origin and aberrant pathway of the recurrent thenar motor branch were associated with the presence of a muscle overlying the TCL.
Carpal tunnel syndrome is one of the most common compressive neuropathies encountered in the hand clinic. For carpal tunnel release, it is often necessary to incise the transverse carpal ligament (TCL) above the median nerve. During the procedure, it is not rare to observe the entire span of the distal TCL covered by a muscle. The muscle belly should be divided along the incision line of the TCL to complete the carpal tunnel release. Few studies have addressed the relationship between the distal muscle belly overlying the TCL and the pathway of the recurrent motor branch12) that has been reported to exhibit various anomalies.3456) Hurwitz1) reported an anomalous course of the thenar motor branch was associated with a hypertrophic muscle overlying the distal TCL. Green and Morgan2) also reported that an anomalous motor branch was found in 93% of the cases with the muscle overlying TCL.
We have observed that the pathway of the recurrent motor branch is not consistent when a muscle belly covering the distal TCL exists. A detailed knowledge on the aberrant pathway of the recurrent motor branch associated with the muscle belly overlying the TCL is very important to avoid an inadvertent injury to the motor branch. We presumed that the muscle belly overlying the distal TCL might serve as a caution for hand surgeons to reduce the risk of recurrent motor branch injury. The purpose of the current study was to investigate the anatomical relationship between the muscle overlying the distal TCL and the thenar motor branch of the median nerve.
We conducted this study in compliance with the principles of the Declaration of Helsinki. The study was an intraoperative anatomical study approved by Institutional Review Board of Samsung Medical Center (IRB No. 2015-12-131-001) and the informed consent was waived. We performed open carpal tunnel release on 192 hands from November 2012 to October 2014. All operations were performed electively by a senior hand surgeon (MJP) using a miniopen method. A 2.0-cm longitudinal incision was made on the ulnar side to the thenar crease. After division of the skin and palmar aponeurosis, we identified the presence of muscle overlying TCL defined as a muscle belly covering the distal TCL from radial to the ulnar end in 25 hands (21 patients). We enrolled these 21 patients into our study and recorded surgical findings. The ligamentous margin was not able to be exposed without dividing the muscle belly in them. So, we traced the recurrent motor branch carefully by incising layer by layer in the order of muscle fascia, muscle belly, and TCL using Metzenbaum scissors to avoid injury of the branch. We dissected the ulnar side of the aberrant muscle belly in order not to injure the recurrent motor branch since the motor branch may be deviated in the ulnar direction towards the muscle belly overlying the TCL (Figs. 1 and 2). When the TCL was incised, the incision was made as far as to the ulnar side. However, a midline incision, which was placed on the median nerve, was often made due to the limited field of the mini-open approach and the risk of ulnar side injury.
The origin of the recurrent motor branch arising from the median nerve was marked on axial and coronal section diagrams of the wrist (Fig. 3). According to subtypes of Lanz classification (group 0 or 1), proximal or distal location of the recurrent motor branch from the origin was distinguished.3) The pathway of the recurrent motor branch into the muscle overlying the TCL was also drawn with description of the variation.
The presence of a muscle overlying the TCL was seen in 25 hands (21 patients, 13%). Among the 21 patients, four patients underwent bilateral carpal tunnel release and presented the same type of origin and anomalous pathway of the recurrent motor branch bilaterally. Multiple motor branches were seen in two hands. One had a double branch and another had a triple branch from the major median nerve. We documented the findings observed in these hands on the main motor branch, which was distinguished from accessory branches by its size and distribution to the muscles.
Of the 25 hands, the type of thenar motor branch was extraligamentous in 11 (44%), transligamentous in seven (28%), and subligamentous in the remaining seven (28%). The locations of the origin were distributed not only on the radial side but on the anterior or ulnar side of the major median nerve. Abnormal branches originating from the unusual side were observed in 14 patients: central-anterior side in eight cases, ulnar-anterior side in five cases, and ulnar side in one case (Figs. 3 and 4).
We also identified unusual pathways of recurrent thenar motor branches, which turned to the ulnar side and coursed into the muscle overlying the TCL in 14 of 25 hands. In particular, there were three motor branches that turned extremely to the ulnar side despite the radial-anterior side origin. These branches were prone to cut if midline incision was performed (Table 1, Figs. 5 and 6).
During carpal tunnel release, routine dissection of the recurrent motor branch is unnecessary. We usually divide the pure ligamentous structure to open the tunnel. However, we sometimes encounter the muscles covering the ligament, which need to be cut. Previous anatomic studies showed no agreement concerning these anomalous muscle bellies. The palmaris brevis, abductor pollicis brevis, flexor pollicis brevis, and flexor digiti quinti are probable candidates of this anomalous muscle.478) Shrewsbury et al.7) reported that the muscle is not palmaris brevis, which never extends past the ulnar margin of the palmar aponeurosis. Hurwitz1) described that this muscle, which lies deeper and directly over the TCL, is the thenar muscle. Green and Morgan2) described that the muscle has anomalous origin of thenar or hypothenar muscles. A recent cadaveric study showed that the anomalous muscle is an extension of the thenar muscles in 85% of cases.9) We performed this study on the assumption that the anomalous muscle fiber is the extension of hypertrophied thenar muscle origins.
The anatomical variations of recurrent motor branch of the median nerve have been described by several authors.134569101112) However, there are few studies highlighting the relationship between the muscle belly overlying the TCL and the pathway of recurrent motor branch.1210) Hurwitz1) described a rare preligamentous course of the motor branch, which was always buried within a muscle overlying the distal TCL. They found this anomaly in 9% of patients, and warned against the risk of injury during release. Mannerfelt and Hybbinette4) first reported an abnormal pathway, in which the motor branch arises from the anterior aspect of the median nerve, turns ulnarly-distally, and passes to the muscles in the buried state. They suggested careful muscle dissection to look for an anomalous branch of the median nerve. Lanz3) reported a similar variation, interpreting the muscle as abductor pollicis brevis pushing the branch far ulnarly. Al-Qattan10) reported that this muscle overlying the TCL always presents in patients with transligamentous or preligamentous type, in which the thenar motor branch runs within the muscle. Henry et al.12) suggested that the presence of a muscle over or interposed within the TCL, prevalent in 18.2% of hands, should serve as a warning sign for potential thenar motor branch variants. They proposed the pooled prevalence of the transligamentous course was 23.4% in patients with a muscle overlying the TCL, as compared to 1.7% without it.
The major concern when dividing the muscle overlying the TCL is the risk of inadvertent cutting of motor branch. Green and Morgan2) recommended that transection of the TCL should not proceed until the motor branch is identified, considering the 90% likelihood of anomalous motor branch associated with the muscles overlying the TCL. However, the motor branch is not seen until the ligament is completely released particularly with a small incision. In patients with the muscle fibers confined to the middle portion of the ligament not covering the distal edge, a risk of motor branch injury should be very low if we cut the muscle fibers keeping ulnar to the midline.10) However, careful attention must be paid when approaching the distal margin because of the variations of branch distribution. If the ligamentous portion of the distal margin can be divided while avoiding the muscle fibers, it should be safe without seeing the motor branch. We noted that a risk of motor branch injury is only present when there is a muscle spanning the distal margin of the ligament, which should be divided to complete the release. Therefore, we focused on patients who had a muscle covering the entire span of the distal margin of the TCL during operation.
In our study, we found many cases with the anomalous branches going within the muscle overlying the TCL, as previously reported.1210) Our results demonstrated that 56% of the motor branch was originated from the central-anterior or ulnar side of the median nerve. It might be noted that the muscle overlying the TCL drives the branch to turn to the ulnar side across the center of the median nerve to reach the muscle in about half of the patients. These branches are most vulnerable to injury regardless of origin site, indicating that careful dissection of the muscle fibers is required to avoid the injury.
We did not dissect all branches from the median nerve because of the additional risk of injury under the limited field. Some patients may have multiple motor branches, indicating the presence of one or more motor branches except the one we found. After dissection of fresh cadavers, Kozin6) reported 4% had more than one motor branch. We observed multiple branches in two hands. In these hands, main motor branch could be distinguished from accessory branches by their small caliber and limited distribution. Although no attempt was made to identify all distal branches, we ascertained that there was no extra motor nerve as a main branch from the median nerve.
A thorough knowledge of the standard and variant anatomy of the muscle belly and accompanying recurrent motor branch in the carpal tunnel is fundamental to prevention of complications during carpal tunnel release. The incidence of aberrant course of motor branch is very low. However, when it comes to the patients with a hypertrophic muscle spanning the distal margin, a considerable number of patients may be at risk of iatrogenic motor branch injury unless careful muscle dissection is carried out during release and thus TCL incision should be made at the ulnar side to avoid motor branch injury.
References
1. Hurwitz PJ. Variations in the course of the thenar motor branch of the median nerve. J Hand Surg Br. 1996; 21(3):344–346. PMID: 8771472.

2. Green DP, Morgan JP. Correlation between muscle morphology of the transverse carpal ligament and branching pattern of the motor branch of median nerve. J Hand Surg Am. 2008; 33(9):1505–1511. PMID: 18984331.

3. Lanz U. Anatomical variations of the median nerve in the carpal tunnel. J Hand Surg Am. 1977; 2(1):44–53. PMID: 839054.

4. Mannerfelt L, Hybbinette CH. Important anomaly of the thenar motor branch of the median nerve: a clinical and anatomical report. Bull Hosp Joint Dis. 1972; 33(1):15–21. PMID: 5025917.
5. Tountas CP, Bihrle DM, MacDonald CJ, Bergman RA. Variations of the median nerve in the carpal canal. J Hand Surg Am. 1987; 12(5 Pt 1):708–712. PMID: 3655229.

6. Kozin SH. The anatomy of the recurrent branch of the median nerve. J Hand Surg Am. 1998; 23(5):852–858. PMID: 9763261.
7. Shrewsbury MM, Johnson RK, Ousterhout DK. The palmaris brevis: a reconsideration of its anatomy and possible function. J Bone Joint Surg Am. 1972; 54(2):344–348. PMID: 4651265.
8. Johnson RK, Shrewsbury MM. Anatomical course of the thenar branch of the median nerve: usually in a separate tunnel through the transverse carpal ligament. J Bone Joint Surg Am. 1970; 52(2):269–273. PMID: 5440004.
9. Hollevoet N, Barbaix E, D'herde K, Vanhove W, Verdonk R. Muscle fibres crossing the line of incision used in carpal tunnel decompression. J Hand Surg Eur Vol. 2010; 35(2):115–119. PMID: 19828566.

10. Al-Qattan MM. Variations in the course of the thenar motor branch of the median nerve and their relationship to the hypertrophic muscle overlying the transverse carpal ligament. J Hand Surg Am. 2010; 35(11):1820–1824. PMID: 20934817.

11. Siverhus SW, Kremchek TE, Smith WR, Basch TM, Drake RL. A cadaveric study of the anatomic variations of the recurrent motor branch of the median nerve. Orthop Rev. 1989; 18(3):315–320. PMID: 2652047.
12. Henry BM, Zwinczewska H, Roy J, et al. The prevalence of anatomical variations of the median nerve in the carpal tunnel: a systematic review and meta-analysis. PLoS One. 2015; 10(8):e0136477. PMID: 26305098.

Fig. 1
Muscle overlying the transverse carpal ligament (arrowhead) and thenar motor branch in a patient. The motor branch arising from the median nerve (arrow) was identified during careful dissection. The right side in the figure is the radial side of the right hand.

Fig. 2
The ulnar side of the aberrant muscle belly was dissected not to injure the recurrent motor branch. The motor branch arising from the ulnar-anterior side of the median nerve (arrow) was identified. The right side in the figure is the radial side of the right hand. Arrowhead: dissected aberrant muscle.

Fig. 3
Diagrams of the TCL with muscle overlying the ligament and motor branch. The right side in each diagram is the radial side. (A) Anterior view. (B) Axial view. TCL: transverse carpal ligament, RB: recurrent motor branch, OM: overlying muscle, MN: median nerve.
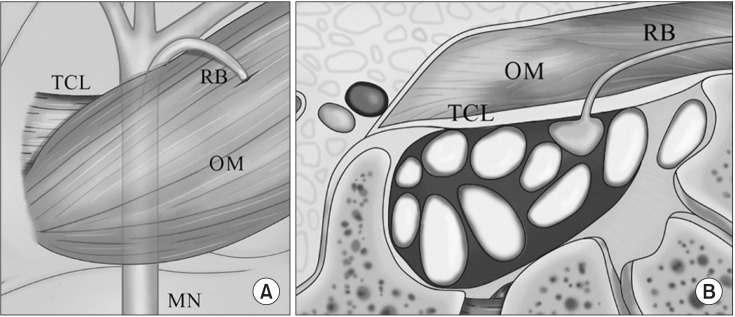
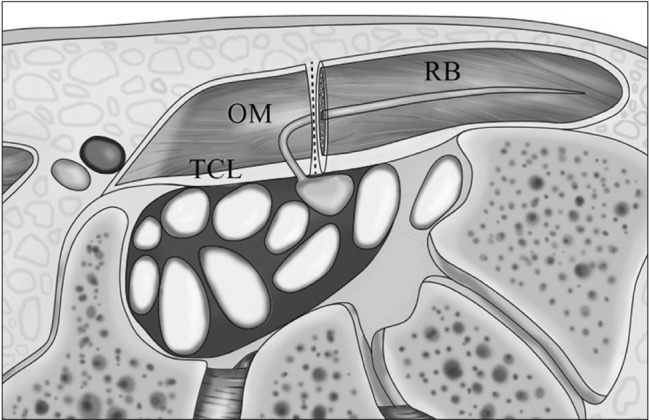
Fig. 5
Pathways of recurrent motor branches (RBs) that are relatively safe in midline incision. The right side is the radial side. TCL: transverse carpal ligament, OM: overlying muscle.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download