This article has been
cited by other articles in ScienceCentral.
Abstract
Background
A skin defect of the hand and wrist is a common manifestation in industrial crushing injuries, traffic accidents or after excision of tumors. We reconstructed a skin defect in the ulnar aspect of the hand and wrist with a perforator-based propeller flap from the ulnar artery. The aims of our study are to evaluate the utility and effectiveness of this flap and to discuss the advantages and disadvantages of the flap in hand and wrist reconstruction with a review of the literature.
Methods
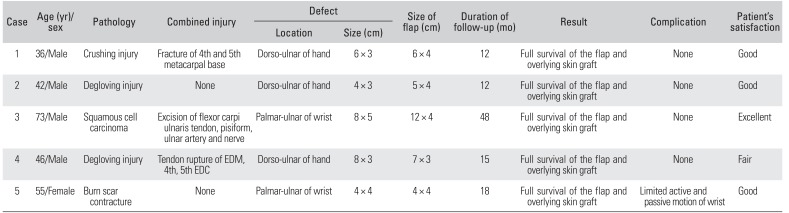
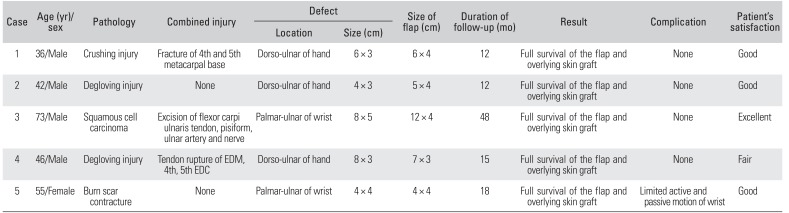
Between April 2011 and November 2016, five cases of skin defect were reconstructed with a perforator-based propeller flap from the ulnar artery. There were four males and one female. The age of patients ranged from 36 to 73 years. Skin defect sites were on the dorso-ulnar side of the hand in three cases and palmar-ulnar side of the wrist in two cases. The size of the skin defect ranged from 4 × 3 cm to 8 × 5 cm. We evaluated the viability of the flap, postoperative complication and patient's satisfaction.
Results
There was no failure of flap in all cases. The size of the flap ranged from 4 × 4 cm to 12 × 4 cm. One patient, who had a burn scar contracture, presented with limited active and passive motion of the wrist after the operation. The other patients had no complications postoperatively. Cosmetic results of the surgery were excellent in one patient, good in three patients, and fair in one patient.
Conclusions
The fasciocutaneous propeller flap based on a perforating branch of the ulnar artery is a reliable treatment option for the ulnar side skin defect of the hand and wrist.
Go to :

Keywords: Ulnar artery, Perforator flap, Wrist
Soft tissue defects of the hand and wrist occasionally present difficult reconstructive problems. Many surgical techniques including forearm flaps are available for the skin defect around the hand.
12) Among the forearm flaps, the radial artery perforator flap is most commonly used. Accordingly, there is a vast amount of literature on the radial artery perforator flap, whereas reports on the ulnar artery perforator flap are rare. Becker and Gilbert
3) initially described the ulnar artery perforator flap and Teo
4) introduced the propeller flap concept. A propeller flap is a uniquely designed transposition-type perforator flap in which flap movement is achieved by rotation around the vascular axis.
45)
Since reconstruction using adjacent tissues is preferable, the ulnar artery perforator propeller flap is more acceptable for the ulnar side soft tissue defect of the hand and wrist than that of the radial artery.
6) Moreover, the ulnar forearm fasciocutaneous flap provides thin, pliable, and sensate skin.
78) The aims of this study are to describe the results of using a fasciocutaneous propeller flap based on a perforating branch of the ulnar artery for soft tissue reconstruction around the hand and wrist and to discuss its advantages and disadvantages with a review of literature.
METHODS
We conducted this study in compliance with the principles of the Declaration of Helsinki. The protocol of this study was reviewed and approved by the Institutional Review Board of Seoul National University Hospital (IRB No. 1709-008-881). Informed consent was obtained from all patients for being included in the study.
Between April 2011 and November 2016, five ulnar artery perforator propeller flaps were performed for ulnar side skin defects of the hand and wrist. Four males and one female with a mean age of 50.4 years (range, 36 to 73 years) were enrolled. The locations of skin defects were the dorso-ulnar side of the hand in three and the palmarulnar side of the wrist in two. Of these skin defects, one patient had a crushing injury and two patients had a degloving injury in a traffic accident. One case of skin defect was due to removal of recurrent squamous cell carcinoma, and the other case was a burn scar contracture. Of the five patients, three patients had combined injuries: one patient had fractures of the base of the fourth and fifth metacarpal bones; one patient had tendon ruptures of the extensor digiti minimi and the fourth and fifth extensor digitorum tendons; and the other patient received excision of the flexor carpi ulnaris tendon, pisiform bone, ulnar artery and nerve due to wide resection of recurrent squamous cell carcinoma. The size of skin defects ranged from 4 × 3 cm to 8 × 5 cm. We evaluated the viability of the flap, postoperative complication and patient's satisfaction. Cosmetic satisfaction was assessed
via a 4-grade questionnaire as excellent, good, fair and bad in outpatient visits at 1 year after operation (
Table 1).
Table 1
Clinical Data of Patients
|
Case |
Age (yr)/ sex |
Pathology |
Combined injury |
Defect |
Size of flap (cm) |
Duration of follow-up (mo) |
Result |
Complication |
Patient's satisfaction |
|
Location |
Size (cm) |
|
1 |
36/Male |
Crushing injury |
Fracture of 4th and 5th metacarpal base |
Dorso-ulnar of hand |
6 × 3 |
6 × 4 |
12 |
Full survival of the flap and overlying skin graft |
None |
Good |
|
2 |
42/Male |
Degloving injury |
None |
Dorso-ulnar of hand |
4 × 3 |
5 × 4 |
12 |
Full survival of the flap and overlying skin graft |
None |
Good |
|
3 |
73/Male |
Squamous cell carcinoma |
Excision of flexor carpi ulnaris tendon, pisiform, ulnar artery and nerve |
Palmar-ulnar of wrist |
8 × 5 |
12 × 4 |
48 |
Full survival of the flap and overlying skin graft |
None |
Excellent |
|
4 |
46/Male |
Degloving injury |
Tendon rupture of EDM, 4th, 5th EDC |
Dorso-ulnar of hand |
8 × 3 |
7 × 3 |
15 |
Full survival of the flap and overlying skin graft |
None |
Fair |
|
5 |
55/Female |
Burn scar contracture |
None |
Palmar-ulnar of wrist |
4 × 4 |
4 × 4 |
18 |
Full survival of the flap and overlying skin graft |
Limited active and passive motion of wrist |
Good |

Surgical Technique
Before the operation, the donor region was mapped for audible Doppler signals that are pulsatile, loud, and high pitched.
9) When a perforating branch was consistently detected by the probe, marking of point was made. Allen's test was used to confirm the patency of the palmar arch preoperatively. All flap operations were performed by a single orthopedic surgeon (YHL) under general anesthesia. A line was drawn between the pisiform and the medial epicondyle of the elbow, which reflects the intermuscular septum between the flexor carpi ulnaris and flexor digitorum superficialis. The flap size was determined according to the size of skin defect, which composed of two asymmetric limbs with an eccentric pivot point. The distance from the perforator to the distal edge of the wound was similar or slightly less than the length of the proximal, longer limb. The upper extremity was elevated and a sterile upper arm tourniquet was inflated without prior exsanguination. In the first step, debridement of dirty wound was done and the necessary flap dimensions were rechecked. The incision and dissection were done in radial to ulnar and distal to proximal directions with the incorporation of the basilic vein. After the flexor carpi ulnaris tendon was exposed, careful retraction of the tendon was performed to the radial side during dissection and elevation of the flap. After the ulnar neurovascular bundle was identified, tracing along the ulnar artery was done to find a perforating branch. After the perforator was identified, it was dissected to allow 180° rotation of the flap. When the flap was rotated 180°, the longer limb was rotated to cover the defect.
Key suture was done to prevent ischemic damage of the remnant skin and compression of the perforating branch. Soft bulky dressing was done with a long arm splint. After 5 to 7 days, donor sites of the flaps were closed with a full or partial thickness skin graft from the anterolateral aspect of the thigh. Range of motion exercises were performed from 2 weeks postoperatively.
Go to :

RESULTS
All flaps survived completely without vascular crisis, flap necrosis, or infection. One patient who had a burn scar contracture showed mild limitation of active and passive motion of the wrist; however, there was an improvement compared with the preoperative range of motion. The size of the flap ranged from 4 × 4 cm to 12 × 4 cm. The mean period of follow-up was 21 months (range, 12 to 48 months) after the operation. The cosmetic results of the operation were excellent in one patient, good in three patients, and fair in one patient.
Case Reports
A 73-year-old male presented with skin and tissue defects on the ulnar side of the wrist due to removal of recurrent squamous cell carcinoma (
Fig. 1A). The flexor carpi ulnaris tendon, pisiform bone and ulnar artery and nerve were resected due to wide excision of the tumor. The size of defect was about 8 × 5 cm. The defect was covered with a 12 × 4 cm fasciocutaneous propeller flap based on a perforating branch of the ulnar artery, harvested under general anesthesia (
Fig. 1B-H). Before the flap key suture, nerve grafting to the injured ulnar sensory and motor nerves was done with the sural nerve (
Fig. 1I and J). On the seventh day after the surgery, full thickness skin grafting was done from the anterolateral aspect of the thigh. The patient was satisfied with the function of the hand and the cosmetic appearance at the 12-month follow-up (
Fig. 1K and L).
 | Fig. 1A 73-year-old male presenting with recurrent squamous cell carcinoma at the wrist. (A) Photograph showing the full-thickness skin defect and exposure of the flexor digitorum superficialis tendon after wide excision of the carcinoma by a tumor surgeon. The flexor carpi ulnaris tendon and pisiform bone are removed and the ulnar artery and nerve are segmentally resected. (B) Design of the perforator-based fasciocutaneous flap with its vascular supply from a perforating branch of the ulnar artery. (C) The flap is dissected carefully and two perforating branches of ulnar artery are identified. (D) The flap is dissected totally and elevated from muscle fascia. (E) Of the two perforating branches, the proximal perforator is ligated and the fasciocutaneous flap is elevated carefully. (F) After 180° of flap rotation in clockwise direction, the flap size is matched to the skin defect. (G) Kinking or compression of the perforating branch is checked to allow 180° of rotation of the flap. (H) The site of perforator is confirmed to allow suture of the flap before nerve grafting. (I) After sural nerve harvesting, nerve grafting is performed to each site of sensory and motor branches of the ulnar nerve. (J) Key suture is performed to prevent ischemic damage of the remnant skin and compression of the perforator. (K, L) At 12 months after surgical treatment with full-thickness skin grafting of the donor site, no functional impairment of the hand motion is observed.
|
Go to :

DISCUSSION
Many surgical techniques are available for soft tissue reconstruction of skin defects of the upper extremity. These include pedicled local, regional and distant flaps. The propeller flap is a local island fasciocutaneous flap based on a single dissected perforator. It is designed as a propeller with two blades of unequal length with the perforator forming the pivot point so that when the blades are switched, the longer arm comfortably fills in the defect.
4) The propeller flap has been used mainly in posttraumatic reconstruction of the lower limb.
10) A perforator-based propeller flap can be designed on any perforator, and many articles have reported the utility and effectiveness of perforator flaps for soft tissue reconstruction of the upper extremity.
111213) The main advantage of a perforator flap is that it does not require division of the underlying main vessel. Although dissection of a perforator can be difficult especially if the course is intramuscular, a perforator-based propeller flap for the upper limb has a good tissue match, 180° arc of rotation and reliability.
14) The propeller flap allows coverage of a wide defect, and it can be raised with a relatively simple surgical technique. Furthermore, it has a high success rate and good cosmetic results without functional impairment.
15)
Ono et al.
14) recommended two perforator-based propeller flaps for wrist and hand reconstruction: the ulnar artery perforator and radial artery perforator. They simply chose an appropriate flap between the two flaps according to the location of the defect. A defect on the radial side of the hand and wrist is covered with a radial artery perforator flap, whereas an ulnar defect is covered by an ulnar artery perforator flap. The radial forearm perforator flap is a large, thin, versatile, well-vascularized flap commonly used to cover moderate-sized hand and wrist defects.
13) The ulnar forearm fasciocutaneous flap is generally suitable for small- to medium-sized defects and is a favorable alterative to the radial forearm flap when thin, pliable and sensate skin is desired.
716) If needed, it may be raised as a fasciocutaneous, functional myocutaneous or osteomyocutaneous flap.
14) In terms of donor site morbidity and cosmesis, a free flap can be a good option. However, it involves a much more technically demanding microsurgical procedure and some literature
617) reported that the ulnar side flap is more aesthetically pleasing due to absence of hair and well-hidden donor site. Therefore, we planned the ulnar artery perforator-based flap for soft tissue defects on the dorso- and palmar-ulnar sides of the hand and wrist.
The upper limb has more than 100 cutaneous perforators with a diameter larger than 0.5 mm.
18) Mathy et al.
8) reviewed 52 consecutive free ulnar forearm fasciocutaneous flaps and reported that the ulnar artery perforator could be found within 3 cm diameter of the ulnar midpoint in 94% of the cases. They also found that all had at least one perforator within 6 cm of the midpoint of the forearm. They reported that this study allowed to elucidate the cutaneous perforator anatomy of the ulnar forearm fasciocutaneous flap. Most perforators were found within the fascial septum between the flexor carpi ulnaris and the flexor digitorum superficialis muscles.
819) In our series, audible Doppler sonogram and Allen's test were used preoperatively to confirm the exact location of perforating branches and a patent palmar arch.
Early propeller flaps were not based on any specific vessel but relied on a thick, subcutaneous pedicle to maintain the flap vascularity. Therefore, rotation of flaps was limited to 90° due to the thickness of flap.
5) Although a two perforator-based flap is safer than a single perforatorbased flap, two vessels can kink each other, posing a potential hazard.
4) The two perforator-based flap is also more challenging to rotate more than 90°. In addition, the major problem of a perforator propeller flap is that the perforating branch has to be twisted for flap rotation. This can lead to flap failure because of kinking and occlusion of the perforator. Many studies on the anatomy of vascularity have been reported recently.
818) It is now possible to elevate propeller flaps that rely on a single perforator.
414) Moreover, experimental studies have reported on the effect of pedicle twisting on flap survival.
202122) In many studies and reports, perforator-based propeller flaps with a rotation up to 180° have been presented to be viable and versatile.
48131423) In our cases, the results of the operation showed that all flaps survived completely without vascular crisis. To prevent perforator kinking and occlusion, we dissected around the perforator and checked the perforating branch cautiously after flap rotation. Actual rotation and key sutures were performed with low-pressure after release of the tourniquet. We also believe that an empty vessel is more susceptible to kinking compared to a vessel with flow as described by Ono et al.
14) We performed full thickness skin grafting for the donor site 5–7 days postoperatively in all cases. This was because if we had immediately sutured the donor site even with low tension, it could have jeopardized the flap vascularity. Limitations of our study include the small case number and relatively short duration of follow-up. We also did not compare with other methods of flap operation.
In conclusion, although there are some difficulties such as dissection around the perforator and rotation of the flap, the fasciocutaneous propeller flap based on a perforating branch of the ulnar artery is a reliable treatment option for the ulnar side skin defect of the hand and wrist in both functional and cosmetic aspects.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download