1. Hove LM. Epidemiology of scaphoid fractures in Bergen, Norway. Scand J Plast Reconstr Surg Hand Surg. 1999; 33(4):423–426. PMID:
10614752.

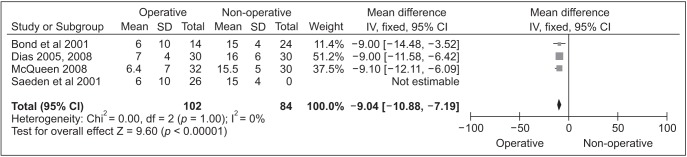
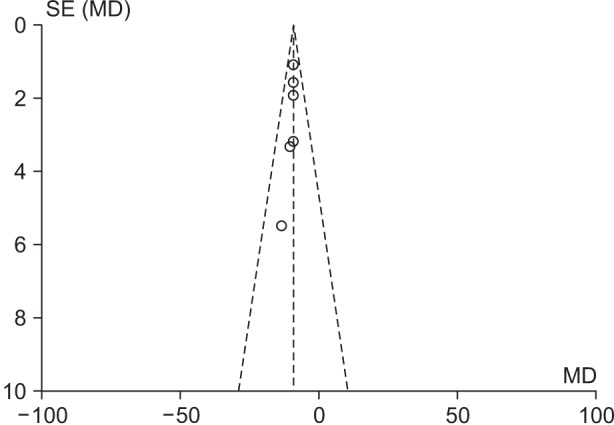
2. Buijze GA, Doornberg JN, Ham JS, Ring D, Bhandari M, Poolman RW. Surgical compared with conservative treatment for acute nondisplaced or minimally displaced scaphoid fractures: a systematic review and meta-analysis of randomized controlled trials. J Bone Joint Surg Am. 2010; 92(6):1534–1544. PMID:
20516332.
3. Paulus MC, Braunstein J, Merenstein D, et al. Variability in orthopedic surgeon treatment preferences for nondisplaced scaphoid fractures: a cross-sectional survey. J Orthop. 2016; 13(4):337–342. PMID:
27436923.

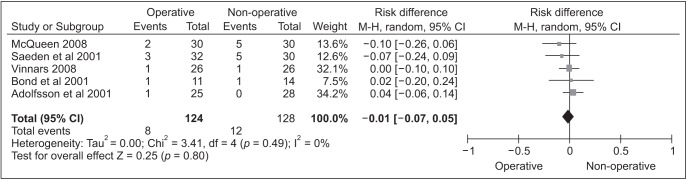
4. Bond CD, Shin AY, McBride MT, Dao KD. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg Am. 2001; 83(4):483–488. PMID:
11315775.

5. Clementson M, Jorgsholm P, Besjakov J, Thomsen N, Bjorkman A. Conservative treatment versus arthroscopic-assisted screw fixation of scaphoid waist fractures: a randomized trial with minimum 4-year follow-up. J Hand Surg Am. 2015; 40(7):1341–1348. PMID:
25913660.
6. McQueen MM, Gelbke MK, Wakefield A, Will EM, Gaebler C. Percutaneous screw fixation versus conservative treatment for fractures of the waist of the scaphoid: a prospective randomised study. J Bone Joint Surg Br. 2008; 90(1):66–71. PMID:
18160502.
7. Vinnars B, Pietreanu M, Bodestedt A, Ekenstam Fa, Gerdin B. Nonoperative compared with operative treatment of acute scaphoid fractures: a randomized clinical trial. J Bone Joint Surg Am. 2008; 90(6):1176–1185. PMID:
18519309.
8. Dias JJ, Dhukaram V, Abhinav A, Bhowal B, Wildin CJ. Clinical and radiological outcome of cast immobilisation versus surgical treatment of acute scaphoid fractures at a mean follow-up of 93 months. J Bone Joint Surg Br. 2008; 90(7):899–905. PMID:
18591600.

9. Adolfsson L, Lindau T, Arner M. Acutrak screw fixation versus cast immobilisation for undisplaced scaphoid waist fractures. J Hand Surg Br. 2001; 26(3):192–195. PMID:
11386765.

10. Dias JJ, Wildin CJ, Bhowal B, Thompson JR. Should acute scaphoid fractures be fixed? A randomized controlled trial. J Bone Joint Surg Am. 2005; 87(10):2160–2168. PMID:
16203878.
11. Saeden B, Tornkvist H, Ponzer S, Hoglund M. Fracture of the carpal scaphoid: a prospective, randomised 12-year follow-up comparing operative and conservative treatment. J Bone Joint Surg Br. 2001; 83(2):230–234. PMID:
11284571.
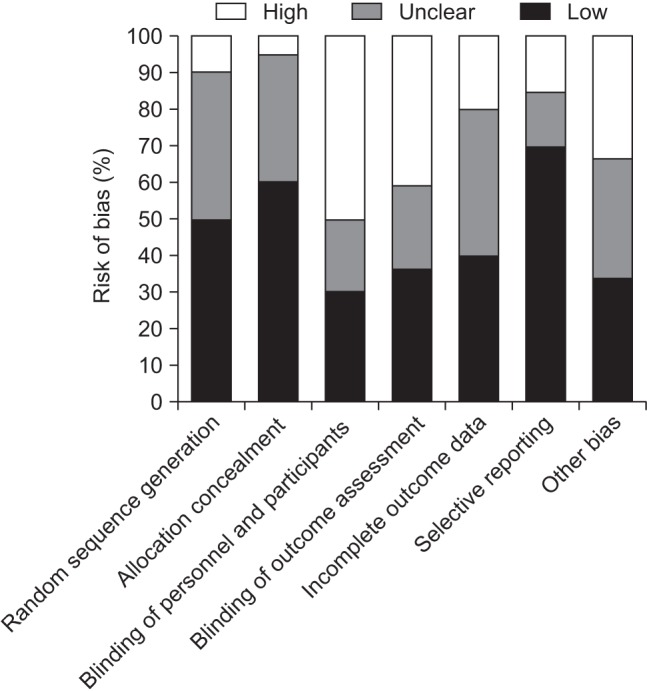
12. Higgins JP, Altman DG, editors. Cochrane handbook for systematic reviews of interventions. ver. 5.1.0. Chichester, UK: John Wiley & Sons;2011. p. 190–193.
13. Anz AW, Bushnell BD, Bynum DK, Chloros GD, Wiesler ER. Pediatric scaphoid fractures. J Am Acad Orthop Surg. 2009; 17(2):77–87. PMID:
19202121.

14. Ring D, Jupiter JB, Herndon JH. Acute fractures of the scaphoid. J Am Acad Orthop Surg. 2000; 8(4):225–231. PMID:
10951111.

15. Mack GR, Kelly JP, Lichtman DM. Scaphoid non-union. In : Lichtman DM, Alexander AH, editors. The wrist and its disorders. Philadelphia, PA: WB Saunders;1997. p. 234–267.
16. Markiewitz AD, Stern PJ. Current perspectives in the management of scaphoid nonunions. Instr Course Lect. 2005; 54:99–113. PMID:
15948438.
17. Mack GR, Bosse MJ, Gelberman RH, Yu E. The natural history of scaphoid non-union. J Bone Joint Surg Am. 1984; 66(4):504–509. PMID:
6707028.

18. Shen L, Tang J, Luo C, Xie X, An Z, Zhang C. Comparison of operative and non-operative treatment of acute undisplaced or minimally-displaced scaphoid fractures: a meta-analysis of randomized controlled trials. PLoS One. 2015; 10(5):e0125247. PMID:
25942316.

19. Armstrong CA, Oldham JA. A comparison of dominant and non-dominant hand strengths. J Hand Surg Br. 1999; 24(4):421–425. PMID:
10473148.

20. Bohannon RW. Grip strength: a summary of studies comparing dominant and nondominant limb measurements. Percept Mot Skills. 2003; 96(3 Pt 1):728–730. PMID:
12831245.

21. Incel NA, Ceceli E, Durukan PB, Erdem HR, Yorgancioglu ZR. Grip strength: effect of hand dominance. Singapore Med J. 2002; 43(5):234–237. PMID:
12188074.
22. Grewal R, Suh N, MacDermid JC. Is casting for non-displaced simple scaphoid waist fracture effective? A CT based assessment of union. Open Orthop J. 2016; 10:431–438. PMID:
27708739.

23. Dias JJ, Taylor M, Thompson J, Brenkel IJ, Gregg PJ. Radiographic signs of union of scaphoid fractures: an analysis of inter-observer agreement and reproducibility. J Bone Joint Surg Br. 1988; 70(2):299–301. PMID:
3346310.

24. Singh HP, Forward D, Davis TR, Dawson JS, Oni JA, Downing ND. Partial union of acute scaphoid fractures. J Hand Surg Br. 2005; 30(5):440–445. PMID:
16006021.

25. Dias JJ, Singh HP. Displaced fracture of the waist of the scaphoid. J Bone Joint Surg Br. 2011; 93(11):1433–1439. PMID:
22058291.

26. Yin ZG, Zhang JB, Kan SL, Wang P. Treatment of acute scaphoid fractures: systematic review and meta-analysis. Clin Orthop Relat Res. 2007; 460:142–151. PMID:
17310931.









 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download