This article has been
cited by other articles in ScienceCentral.
Abstract
Background
A variety of treatment options suggest that the optimal treatment strategy for lateral elbow tendinopathy (LET) is not known, and further research is needed to discover the most effective treatment for LET. The purpose of the present study was to verify the most effective position of eccentric stretching for the extensor carpi radialis brevis (ECRB) in vivo using ultrasonic shear wave elastography.
Methods
A total of 20 healthy males participated in this study. Resting position was defined as 90° elbow flexion and neutral position of the forearm and wrist. Elongation of the ECRB was measured for four stretching maneuvers (forearm supination/pronation and wrist extension/flexion) at two elbow angles (90° flexion and full extension). The shear elastic modulus, used as the index of muscle elongation, was computed using ultrasonic shear wave elastography for the eight aforementioned stretching maneuverangle combinations.
Results
The shear elastic modulus was the highest in elbow extension, forearm pronation, and wrist flexion. The shear elastic moduli of wrist flexion with any forearm and elbow position were significantly higher than the resting position. There was no significant difference associated with elbow and forearm positions except for elbow extension, forearm pronation, and wrist flexion positions.
Conclusions
This study determined that elbow extension, forearm pronation, and wrist flexion was the most effective eccentric stretching for the ECRB in vivo.
Go to :

Keywords: Stretching, Extensor carpi radialis brevis, Lateral elbow tendinopathy, Ultrasonic shear wave elastography, Shear elastic modulus
Lateral elbow tendinopathy (LET) is a painful musculoskeletal condition caused by overuse and the injury of the common extensor tendon originating from the lateral epicondyle is better known as tennis elbow.
1) LET is one of the most common lesions of the arm work-related or sportrelated pain disorder.
2) The condition is usually defined as a syndrome of pain in the area of the lateral epicondyle, which may be degenerative rather than inflammatory.
3)
Many clinicians advocate a conservative approach as the treatment of choice for LET.
3) Physiotherapy is a conservative treatment usually recommended for the LET patients.
34) A wide array of physiotherapy treatments have been recommended for the management of LET.
56) While these treatments have different theoretical mechanisms of action, they all have the same aim of reducing pain and improving the function. Such a variety of treatment options suggest that the optimal treatment strategy is not known, and more research is needed to discover the most effective treatment in patients with LET.
56)
One of the most common physiotherapy treatments for LET is an exercise program.
34) One such program consisting of eccentric exercises has shown good clinical results in LET and in conditions similar to LET in clinical behavior and histopathologic appearance, such as patellar and Achilles tendinopathy.
7) Such an exercise program is used as the first treatment option for our patients with LET.
8)
A new ultrasound-based technology called ultrasonic shear wave elastography (SWE) has been developed, allowing for a reliable and noninvasive measurement of soft-tissue viscoelastic properties.
9) SWE monitors the propagation of shear waves generated in tissue using acoustic radiation forces and is able to evaluate the shear elastic modulus of individual muscles.
10) Due to the strong linear relationship, identified by prior studies, between passive muscle tension calculated by traditional methods and the shear elastic modulus measured by SWE
in vitro,
1112) SWE has been used in many studies of skeletal muscle stretching.
1112) In addition, our previous studies indicated an increase in the shear elastic modulus with muscle elongation during stretching.
1314) Therefore, SWE has proven to be a valid technology for noninvasively investigating muscle elongation
in vivo.
Therefore, in the present study, we hypothesized that elbow extension, forearm pronation, and wrist flexion is the most effective eccentric stretching of the extensor carpi radialis brevis (ECRB). The objective of this study was to quantitatively verify the most effective position of eccentric stretching for the ECRB using the shear elastic modulus measured by SWE in vivo.
METHODS
Participants
With Institutional Review Board of Dankook University Hospital exempt approval (IRB No. DKUH IRB 2017-06-004), a total of 20 males (age, 28.75 ± 3.74 years; height, 177.70 ± 5.30 cm; weight, 77.55 ± 6.35 kg) with no orthopedic or nervous system abnormalities in the upper limbs participated in this study. Informed consents were obtained from all participants. The participants were recruited from the students at our institution. The participants orally confirmed that they complied with the following exclusion criteria: women, athletes or persons who perform any extensive exercise, and persons having a history of orthopedic disease or neuropathy in the upper limbs. The sample size was calculated by use of G*Power software ver. 3.1 (Heinrich-Heine-University, Dusseldorf, Germany) for a one-way analysis of variance (ANOVA) with repeated measures (effect size, 0.25; α error, 0.05; power, 0.8), which showed that 17 participants were required. The study protocol conformed to the principles of the Declaration of Helsinki.
Experimental Procedures
This study was an experimental study. After the aim and procedures were explained to all participants, the participants underwent eight stretching maneuvers performed by one researcher (JKK). The outcome was measured and analyzed by other orthopedic surgeon researchers (JYL and JSY). All procedures were performed by the two orthopedic surgeons (JYL and JSY), who have 6 and 9 years of post-training experience in ultrasound. They measured the shear elastic modulus using SWE, whereas the other (JKK) performed the stretching maneuver. The nondominant upper limbs (2 right and 18 left limbs) were chosen for intervention.
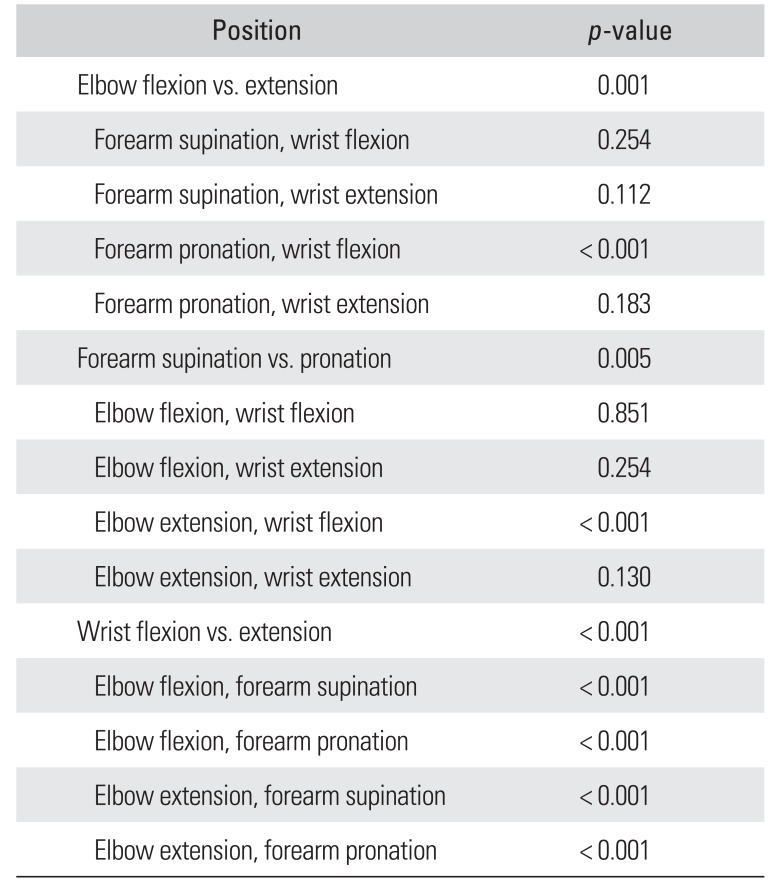
Each participant lay on the bed with 30° abduction of the shoulder. The resting position is defined as 90° elbow flexion and neutral position of the forearm and wrist. Two forearm positions (supination and pronation), two stretching maneuvers (wrist flexion and extension) were investigated at two elbow positions (90° flexion and full extension) for a total of eight stretching positions (
Fig. 1).
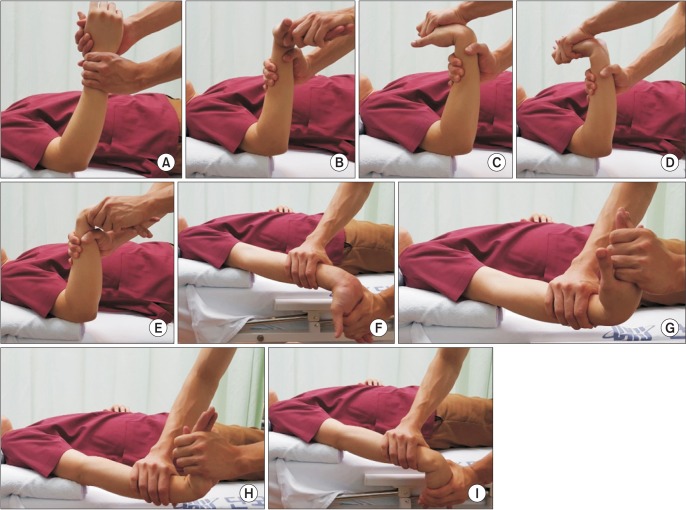 | Fig. 1Passive stretching position. (A) Resting. (B) Elbow flexion, forearm supination, and wrist extension. (C) Elbow flexion, forearm supination, and wrist flexion. (D) Elbow extension, forearm pronation, and wrist extension. (E) Elbow flexion, forearm pronation, and wrist flexion. (F) Elbow extension, forearm supination, and wrist extension. (G) Elbow extension, forearm supination, and wrist flexion. (H) Elbow extension, forearm pronation, and wrist extension. (I) Elbow extension, forearm pronation, and wrist flexion.
|
The participants underwent stretching until reaching a point of discomfort without pain, as verbally acknowledged by the participants. During all stretching maneuvers and measurement acquisitions, the participants were instructed to relax as much as possible.
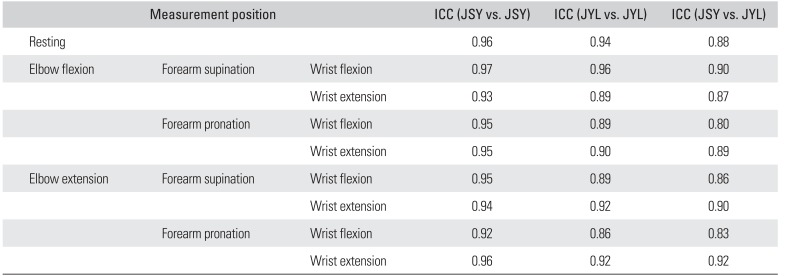
Elastography
All volunteers were examined with an Acuson S2000 Helx (Siemens, Mountain View, CA, USA) used for SWE. The linear array probe (9L4, Siemens) was used. The SWE measurements were reported in m/sec. The measurement place was defined as 2 inches distal from the lateral epicondyle to obtain equal measuring points. The probe was placed parallel to the muscle fascicle of the ECRB after the detection of the ECRB with axial ultrasonography (
Fig. 2).
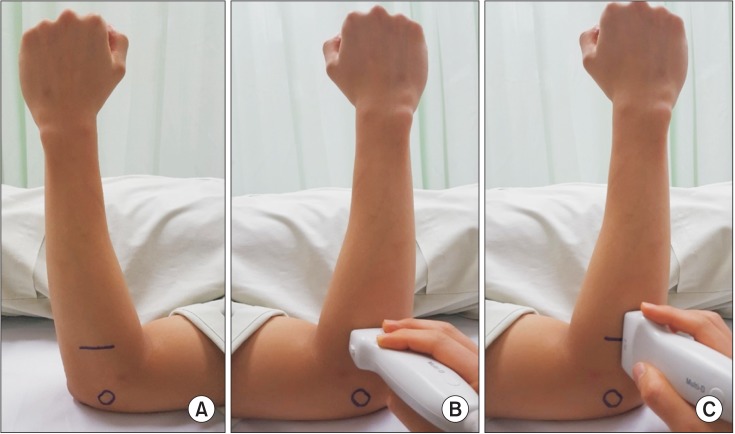 | Fig. 2Location of probe. (A) A line is drawn 2 inches apart from the lateral epicondyle indicated by the circular mark. (B) The extensor carpi radialis brevis is detected with axial sonography. (C) The shear elastic modulus is examined with the probe positioned along the extensor carpi radialis brevis musculature.
|
The elastography was performed with acoustic radiation force impulse, which does not require compression of the transducer and is thus less operator-dependent than the conventional ultrasonic elasticity imaging methods. After acoustic radiation force impulse of the ECRB, the elastography was set to measure a shear wave speed between 0.5 and 6.5 m/sec.
The shear elastic modulus was measured in all measurement positions using SWE. The region of interest (ROI) was established near the center point of the muscle belly on the ultrasound image (
Fig. 3). The shear elastic modulus was measured two times by each investigator and the mean value was used for further analysis. The ROI size and shape were fixed by the U.S. system. The means for each muscle in m/sec were converted to kPa by using the conversion factor E = V
2 × 3, where E is the elasticity in kPa and V is shear wave speed in m/sec. This conversion factor is applicable in isotropic incompressible tissues and has been used for measurements in the liver.
15) Muscle tissue is incompressible, but not necessarily isotropic. Especially profound SWE measurements were difficult to obtain, and the US system in some cases reported a value of X.XX m/sec, for which the measurements were then repeated until a valid measurement was achieved. No recordings of the number of invalid measurements were stored.
 | Fig. 3Ultrasonography of shear elastic modulus. (A) Axial view of ultrasonography. (B) Longitudinal view of ultrasonography. ECRL: extensor carpi radialis longus, ECRB: extensor carpi radialis brevis, EDC: extensor digitorum communis, ROI: region of interest.
|
Statistics
Statistical analyses were performed with IBM SPSS ver. 20.0 (IBM Corp., Armonk, NY, USA). To find whether the ECRB was elongated in the eight stretching positions, the differences in the shear elastic modulus between the resting position (elbow flexion and neutral forearm and wrist) and each stretching position were assessed with the paired Student t-test with Bonferroni correction.
When the shear elastic modulus was found to be significantly different from that at rest, a one-way ANOVA with repeated measures was used to determine the effect of eccentric stretching on the shear elastic moduli among them. In addition, independent Student t-test was used to evaluate the effect of each joint position if a significant main effect was found. The confidence level of 0.05 was used in all statistical tests.
The reliability of the shear elastic modulus measurements was confirmed using the κ coefficients, which represent intra- and interobserver reliability: “slight agreement,” 0.00–0.20; “fair agreement,” 0.21–0.40; “moderate agreement,” 0.41–0.60; “substantial agreement,” 0.61–0.80; and “almost perfect agreement,” 0.81–1.00.
Go to :

RESULTS
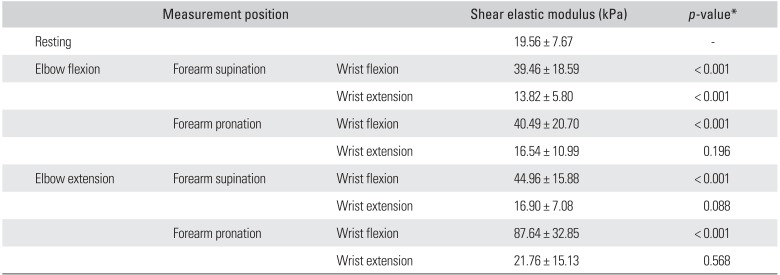
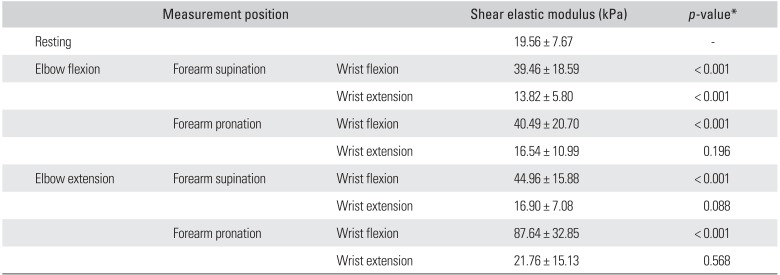
The shear elastic modulus for each measurement is shown in
Table 1. The shear elastic modulus was the highest at elbow extension, forearm pronation, and wrist flexion. The shear elastic moduli of all wrist flexion positions with any elbow and forearm positions were significantly higher than the elastic modulus at rest (
p < 0.001) (
Table 1).
Table 1
Shear Elastic Modulus of Extensor Carpi Radialis Brevis in Each Measurement Position
|
Measurement position |
|
Shear elastic modulus (kPa) |
p-value*
|
|
Resting |
|
|
19.56 ± 7.67 |
- |
|
Elbow flexion |
Forearm supination |
Wrist flexion |
39.46 ± 18.59 |
< 0.001 |
|
|
Wrist extension |
13.82 ± 5.80 |
< 0.001 |
|
Forearm pronation |
Wrist flexion |
40.49 ± 20.70 |
< 0.001 |
|
|
Wrist extension |
16.54 ± 10.99 |
0.196 |
|
Elbow extension |
Forearm supination |
Wrist flexion |
44.96 ± 15.88 |
< 0.001 |
|
|
Wrist extension |
16.90 ± 7.08 |
0.088 |
|
Forearm pronation |
Wrist flexion |
87.64 ± 32.85 |
< 0.001 |
|
|
Wrist extension |
21.76 ± 15.13 |
0.568 |

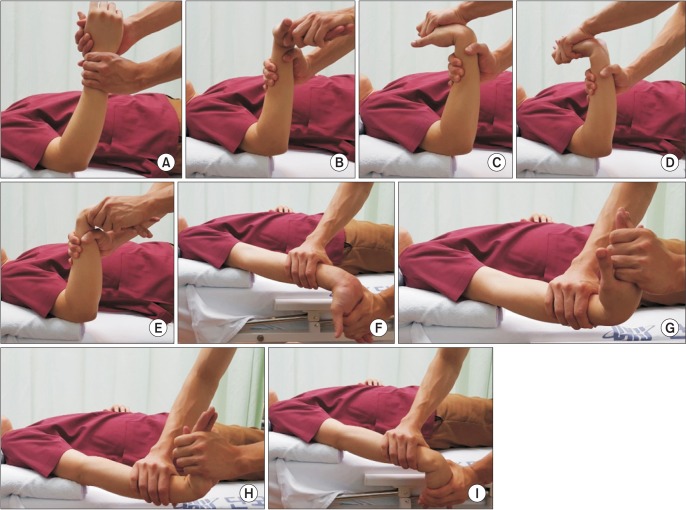
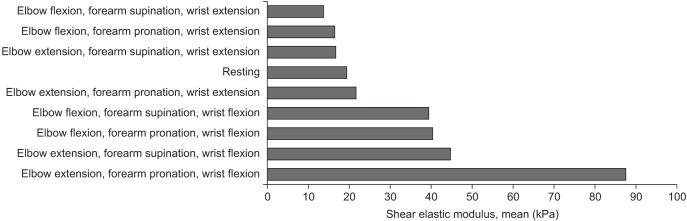
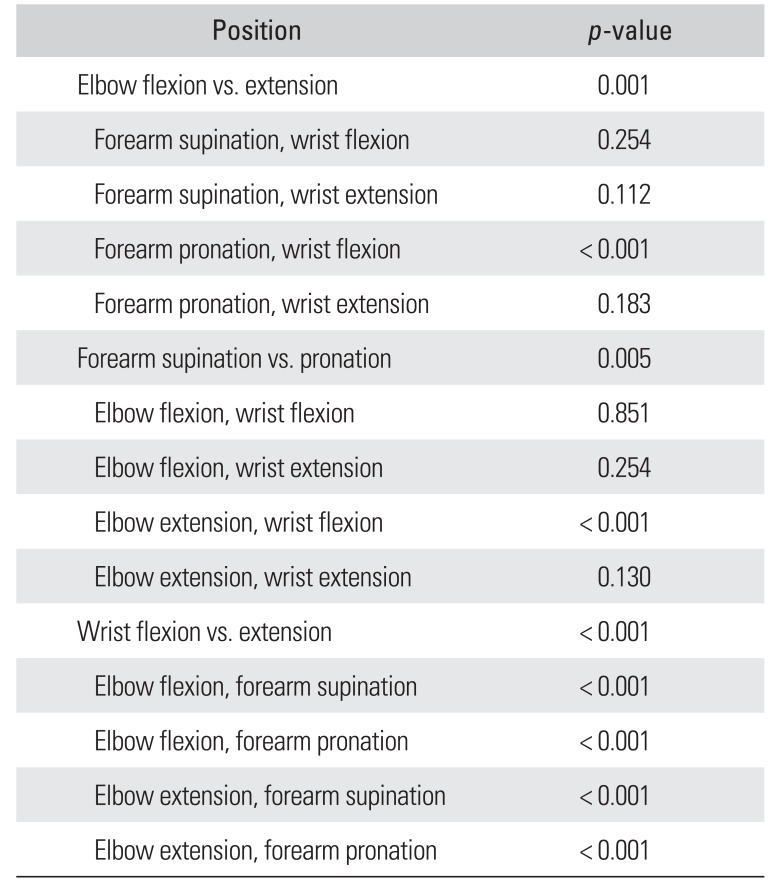
For the measurement positions in which the shear elastic modulus were significantly higher than those at rest, a one-way ANOVA with repeated measures was used to indicate a significant main effect. For the positions showing significantly higher shear elastic moduli than the elastic modulus at rest, a Bonferroni multiple comparison procedure for the post hoc test was performed, indicating that the shear elastic moduli of elbow extension, forearm pronation, and wrist flexion were significantly higher than those of the other positions. There were significant differences among each joint position. The
p-value of elbow joint position was 0.001, forearm was 0.005, and wrist was < 0.001. Moreover, every eccentric stretching positions show significant differences between wrist flexion and extension (
p < 0.001). However, no significant differences between elbow and forearm positions were observed, except for elbow extension, forearm pronation and wrist flexion (
Table 2 and
Fig. 4).
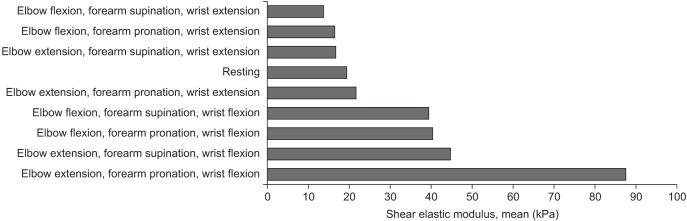 | Fig. 4Multiple comparisons of shear elastic modulus. The shear elastic modulus in elbow extension, forearm pronation, and wrist flexion is significantly higher (p < 0.001) than that in all the other positions. The shear elastic moduli for all wrist flexion positions are significantly higher (p < 0.001) than in the resting position.
|
Table 2
Comparison of Shear Elastic Modulus in Separate Motion of Joint
|
Position |
p-value |
|
Elbow flexion vs. extension |
0.001 |
|
Forearm supination, wrist flexion |
0.254 |
|
Forearm supination, wrist extension |
0.112 |
|
Forearm pronation, wrist flexion |
< 0.001 |
|
Forearm pronation, wrist extension |
0.183 |
|
Forearm supination vs. pronation |
0.005 |
|
Elbow flexion, wrist flexion |
0.851 |
|
Elbow flexion, wrist extension |
0.254 |
|
Elbow extension, wrist flexion |
< 0.001 |
|
Elbow extension, wrist extension |
0.130 |
|
Wrist flexion vs. extension |
< 0.001 |
|
Elbow flexion, forearm supination |
< 0.001 |
|
Elbow flexion, forearm pronation |
< 0.001 |
|
Elbow extension, forearm supination |
< 0.001 |
|
Elbow extension, forearm pronation |
< 0.001 |

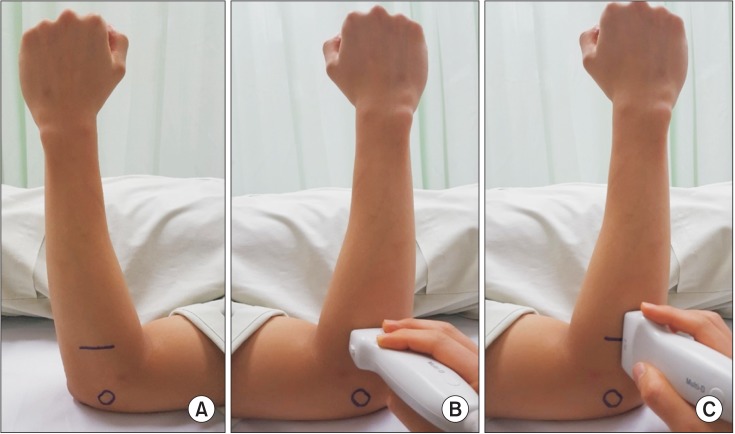
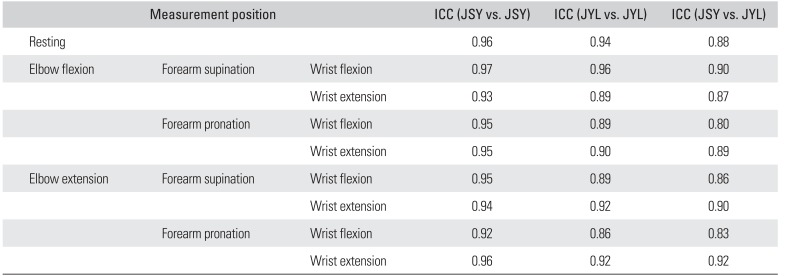
Interobserver reliability (JYL and JSY) of SWE was in almost perfect agreement with a weighted κ coefficient of 0.80–0.92 and intraobserver reliabilities of SWE also were in almost perfect agreement with a weighted κ coefficient of 0.86–0.96 (JYL) and 0.92–0.97 (JSY) (
Table 3).
Table 3
Reliability of Shear Elastic Modulus
|
Measurement position |
|
ICC (JSY vs. JSY) |
ICC (JYL vs. JYL) |
ICC (JSY vs. JYL) |
|
Resting |
|
|
0.96 |
0.94 |
0.88 |
|
Elbow flexion |
Forearm supination |
Wrist flexion |
0.97 |
0.96 |
0.90 |
|
|
Wrist extension |
0.93 |
0.89 |
0.87 |
|
Forearm pronation |
Wrist flexion |
0.95 |
0.89 |
0.80 |
|
|
Wrist extension |
0.95 |
0.90 |
0.89 |
|
Elbow extension |
Forearm supination |
Wrist flexion |
0.95 |
0.89 |
0.86 |
|
|
Wrist extension |
0.94 |
0.92 |
0.90 |
|
Forearm pronation |
Wrist flexion |
0.92 |
0.86 |
0.83 |
|
|
Wrist extension |
0.96 |
0.92 |
0.92 |

Go to :

DISCUSSION
This is the first study to determine the effectiveness of eccentric stretching for the ECRB using shear elastic modulus values measured by SWE, which quantitatively reflects the grade of muscle elongation during stretching in vivo. The main finding of this study is that elbow extension, forearm pronation, and wrist flexion is most effective eccentric stretching position of the ECRB.
The study by Alfredson et al.
16) was the first to propose the eccentric training of the injured tendon. It is the most commonly used conservative approach in the treatment of tendinopathy. Eccentric exercises appear to reduce the pain and improve function, reversing the pathology of LET
1718) as supported by experimental studies on animals.
19)
The conservative, therapy-based treatment that has been suggested to be the first-line of treatment for tennis elbow is eccentric exercise, which involves lengthening the musculotendinous unit while a load is applied to it.
2021) In clinical trials, a program of eccentric exercises has demonstrated superior efficacy in the treatment of LET, as compared to therapeutic ultrasound, bracing, transcutaneous electrical nerve stimulation, friction massage, heat and ice.
2223) Although eccentric exercise has demonstrated encouraging results, eccentric exercises are various and the optimal position has not yet been defined.
10) Therefore, in the present study, we try to figure out the most effective eccentric stretching position with SWE evaluation.
Few investigators have attempted to understand the relationship between muscle elasticity and passive muscle force.
2425) For example, Nordez et al.
24) used transient elastography to measure shear elastic modulus of human gastrocnemius muscle and reported a fairly strong linear relationship. Furthermore, Umehara et al.
25) evaluated the effective stretching position of the pectoralis minor with shear elastic modulus measurements.
Young's modulus is defined simply as the ratio between the applied stress and the induced strain.
9) It quantifies tissue stiffness; hard tissues have a higher Young's modulus than soft ones.
9) The shear wave has a bipolar directivity pattern and mainly propagates along the transverse direction. Its velocity, typically a few meters per second in soft tissues, is directly linked to shear elasticity if the medium is assumed to be purely elastic: µ = ρc
2 where c is the speed of the shear wave and ρ is the density of the medium. As dealing with soft tissues, Young's modulus of the medium can be quantitatively estimated by measuring the shear-wave speed: elasticity (E) = 3µ = 3ρc
2, where ρ is the density of tissue expressed in kg/m
3.
9) Given that the density of tissues is well known (1,000 kg/m
3), if the shear wave propagation velocity c can be measured, the elasticity of the tissue can be determined.
926)
A more detailed interpretation of shear modulus results from SWE is difficult to provide. It is clear that the shear moduli values obtained from off-axis ultrasound trials are only minimally related to Young's modulus during physiologically-relevant axial loading. As skeletal muscle may be considered transversely isotropic, it is perhaps only accurate to report shear modulus, as calculated from shear wave speed, when the ultrasound transducer and subsequent shear wave propagation are aligned longitudinally with the underlying muscle fibers.
27) In this study, the shear elastic modulus were also measured when the probe was located along the muscle fiber of ECRB.
We hypothesized that the ECRB could be elongated by elbow, forearm, and wrist position. This study showed that the all wrist flexion positions were higher than the resting position. Furthermore, elbow extension, forearm pronation and wrist flexion was significantly higher than those of all measurement positions whose shear elastic moduli were higher than that at rest. These results suggest that the most effective eccentric stretching position for the ECRB is elbow extension, forearm pronation, and wrist flexion (
Fig. 5).
 | Fig. 5Photographs showing the most effective eccentric stretching position of the extensor carpi radialis brevis.
|
However, this study has several limitations. First, the participants were healthy young males as prescribed by the exclusion criteria. Therefore, it is unknown whether similar effects can always be expected in the patients with LET. Second, the ROI was located at the center of ECRB without the measurement of the distance to bone in this study. Few studies have directly evaluated the effect of bone tissue or other hard tissue components using ultrasonography or SWE.
2829) SWE depicts relative strain, and the elastography is influenced by the presence of bone.
30) Third, the investigator of SWE could not be blinded from the stretching position of the arm. Therefore, the observer bias could have occurred. Furthermore, SWE is a highly operator-dependent technique in terms of the application of the pressure to the probe and the differentiation of the artifacts from the diagnostic image information. Although the operator dependency is a known challenge in U.S., we tried to obtain appropriate images by marking on the skin and double checking the ECRB with axial images.
This study determined that elbow extension, forearm pronation, and wrist flexion was the most stretched position for the ECRB in vivo. This position can be recommended for the eccentric exercise treatment in LET.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download