This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Diffuse idiopathic skeletal hyperostosis (DISH) is characterized by ossification of the enthesis. The diagnosis has been mainly based on the chest or whole spine lateral plain film. Recently, chest or thoracolumbar computed tomography (CT) has been reported to be more reliable for the diagnosis of DISH. The purposes of this study were to investigate the prevalence and location of DISH and evaluate the prevalence of comorbidities, such as ossification of the posterior longitudinal ligament (OPLL) and ossification of the ligamentum flavum (OLF), using whole spine CT.
Methods
Whole spine CT scans of patients over 16 years of age who were examined at Cheju Halla General Hospital between February 2011 and December 2016 were reviewed for this study. The diagnosis of DISH was made according to the modified Resnick criteria. The prevalence of DISH in each age decade and its location were evaluated. Also, the prevalence of OPLL and OLF in DISH patients was investigated.
Results
The overall incidence of DISH was 24.4% (40 of 164 cases). There was no case of DISH in patients in their 40s and younger. The percentile incidences of DISH in patients in their fifth, sixth, seventh, eighth, and ninth decades were 20.0% (4 of 20 cases), 32.3% (10 of 31 cases), 40.0% (10 of 25 cases), 34.5% (10 of 29 cases), and 27.3% (6 of 22 cases), respectively. A strong positive correlation between the age decade and the incidence of DISH was noted (r = 0.853, p = 0.007). DISH patients had higher incidences of OLF (22.5%) and OPLL (37.5%). The most common location of DISH was the middle thoracic spine (90.0%) followed by the lower thoracic spine (87.5%). There was one case of DISH involving only the cervical spine.
Conclusions
The incidence of DISH diagnosed by CT was higher than we expected. Whole spine CT can be a valuable modality to evaluate the location of DISH in the cervical and lumbar spine and the comorbidity rates of OLF and OPLL.
Go to :

Keywords: Spine, Computed tomography, Hyperostosis, Diffuse idiopathic skeletal, Prevalence
Diffuse idiopathic skeletal hyperostosis (DISH), also known as Forestier-Rotes-Querol disease,
1) is a systemic noninflammatory disease of unknown etiology. It is characterized by progressive ossification of the anterior longitudinal ligament and bone proliferation at the enthesis. Although the diagnostic methodology for DISH has not been established, diagnostic criteria suggested by Resnick and Niwayama
2) in 1976 have been used most commonly: (1) flowing bridging ossification of at least four contiguous vertebrae without disc degeneration which is estimated from preservation of the intervertebral disc space and (2) absence of degeneration or fusion of sacroiliac joints and apophyseal joints.
Awareness of DISH is growing as related morbidities have been reported. There are several reports that described the relationships between metabolic or cardiovascular disease and DISH.
3) Various conditions related to atypical DISH of the cervical or lumbar spine have been recently reported. Dysphagia or dyspnea can occur in patients with DISH of the cervical spine.
45) Some types of lumbar spinal stenosis or changes in spinopelvic alignment can develop due to DISH of the lumbar spine.
6) There are several reports on spinal fractures in patients with ankylosing spinal disorders.
789) DISH was even considered as a less known cause of back pain or impaired physical function.
1011)
DISH has been traditionally evaluated by using a plain film of the chest or abdomen. Recently, chest and thoracolumbar computed tomography (CT) scans are used for evaluation of DISH. Diagnosis by these CT scan images has been reported more reliable.
121314) However, there is no report that evaluates epidemiology and etiology of DISH using whole spine CT scan images. Coprevalence of thoracic, cervical, and lumbar DISH can be evaluated by whole spine CT. Furthermore, whole spine CT can show ossification of the posterior longitudinal ligament (OPLL) of the cervical spine or ossification of the ligamentum flavum (OLF) with DISH simultaneously. In the present study, by using whole spine CT scan images, we evaluated the coprevalence of typical DISH (thoracic) and atypical DISH (lumbar and/or cervical) as well as epidemiology of DISH.
METHODS
This retrospective study was approved by the Institutional Review Board of Cheju Halla General Hospital (IRB No. 2017-L19-01) and all protocols were performed in accordance with the principles of the Declaration of Helsinki. Written informed consents were obtained.
Subjects
Whole spine CT scan images of patients over 16 years of age, examined at Cheju Halla General Hospital between February 2011 and December 2016, were reviewed for this study. Patients who had a spine surgery or traumatic spine fracture were excluded. Patients with ankylosing spondylodiscitis or metastatic spinal tumor were also excluded.
Evaluation of CT
A total of 164 whole spine CT scans were available for the analysis. A 64-slice multidirector CT scanner (iCT 128 scanner; Philips, Cleveland, OH, USA) was used for this study. Digital images of the whole spine were reconstructed and evaluated by software application of picture archiving and communication system (PACS; STARPACS5081, Infinitt Healthcare, Seoul, Korea).
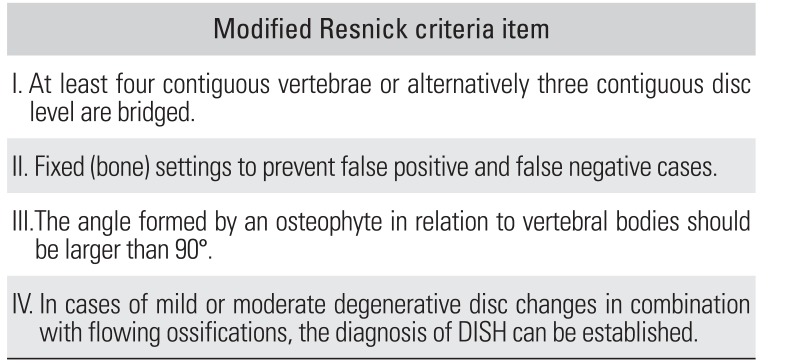
A definitive diagnosis of DISH was made according to the criteria by Resnick and Niwayama.
2) Some modifications of Resnick criteria presented by Oudkerk et al.
13) were applied in this study. One was the angle formed by an osteophyte in relation to vertebral bodies, which should be larger than 90° to differentiate flowing ossification from bridging degenerative osteophytes. In the case with only severe disc degenerative changes, diagnosis of DISH was not made. In the case of mild or moderate degenerative disc changes in combination with flowing ossifications, DISH could be diagnosed. We included incomplete bridge ossification between vertebral bodies in the criteria of DISH (
Table 1).
Table 1
Modified Resnick Criteria for Diagnosis of DISH Based on CT by Oudkerk et al.13)
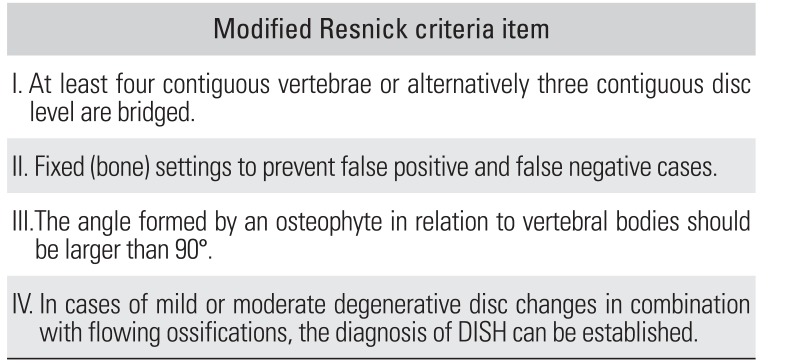
|
Modified Resnick criteria item |
|
I. At least four contiguous vertebrae or alternatively three contiguous disc level are bridged. |
|
II. Fixed (bone) settings to prevent false positive and false negative cases. |
|
III.The angle formed by an osteophyte in relation to vertebral bodies should be larger than 90°. |
|
IV. In cases of mild or moderate degenerative disc changes in combination with flowing ossifications, the diagnosis of DISH can be established. |

The incidences of typical DISH (thoracic) and atypical DISH (lumbar and/or cervical) were evaluated. Coexisting DISH of another spine region in typical DISH was investigated. The location of DISH was divided into five regions: cervical (C1–7), upper thoracic (T1–4), middle thoracic (T5–8), lower thoracic (T9–12), and lumbar spine (L1–5). Prevalence of each region was evaluated. Difference in the prevalence of OPLL or OLF between patients with and without DISH was evaluated. Clinical parameters such as age and sex were also reviewed. All whole spine CT scan images were analyzed twice by two orthopedic surgeons (MGY and SJK) with a 3-month interval. All images were presented to the observers in a randomized order.
Statistical Analysis
Data analysis was performed using IBM SPSS ver. 19.0 (IBM Corp., Armonk, NY, USA). Pearson correlation test was used to assess the prevalence of DISH in each age decade. Chi-square test was used to compare the prevalence of DISH between sex. An intraclass correlation coefficient (ICC) was calculated for assessment of the intra- and interobserver reliability. The reliability was determined by repeating measurement in 30 subjects with a 3-month interval after initial measurement on CT scans. A p-value less than 0.05 was considered statistically significant.
Go to :

RESULTS
Prevalence of DISH
The overall incidence of DISH was 24.4% (40 of 164 cases). There was no DISH in patients in their 30s and 40s. The percentile incidences of DISH in patients in their fifth, sixth, seventh, eighth, and ninth decades were 20.0% (4 of 20 cases), 32.3% (10 of 31 cases), 40.0% (10 of 25 cases), 34.5% (10 of 29 cases), and 27.3% (6 of 22 cases), respectively (
Fig. 1). A strong positive correlation between age divided by decade and prevalence of DISH was noted (r = 0.853,
p = 0.007). In males, 27 of 85 subjects (31.7%) were diagnosed with DISH by whole spine CT, whereas in females, 13 of 82 (15.8%) were diagnosed. The prevalence of DISH was about twice higher in males than in females, showing statistically significant difference between sex (
p < 0.019).
 | Fig. 1Prevalence of diffuse idiopathic skeletal hyperostosis (DISH) based on whole spine computed tomography in each decade.
|
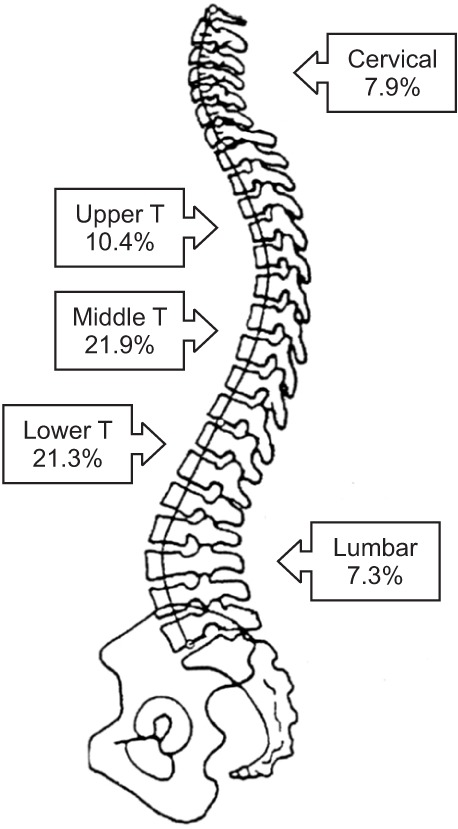
Location of DISH
The most common location of DISH was the middle thoracic spine (90.0%) followed by the lower thoracic spine (87.5%). There was one case of atypical DISH involving the cervical spine only (
Fig. 2) and one case of DISH involving only the upper thoracic region (
Fig. 3). The prevalence of DISH at each region was as follows: for the cervical, upper, middle, lower thoracic and lumbar spine, the prevalence was 7.9%, 10.4%, 21.9%, 21.3%, and 7.3%, respectively (
Fig. 4). When there was DISH in the middle or lower thoracic region, the rate of coexisting DISH in the cervical and lumbar region was 33.0% and 30.7%, respectively.
 | Fig. 2A case of diffuse idiopathic skeletal hyperostosis involving only cervical spine (C3–6). Flowing bridging ossification and partial ossification (arrows) of three contiguous disc levels (C3–6) are noted in consecutive sagittal images (A, B) of whole spine computed tomography.
|
 | Fig. 3A case of diffuse idiopathic skeletal hyperostosis involving only upper thoracic spine (T3–6). Flowing bridging ossification (arrows) of three contiguous disc levels (T3–6) is noted in a sagittal image of whole spine computed tomography.
|
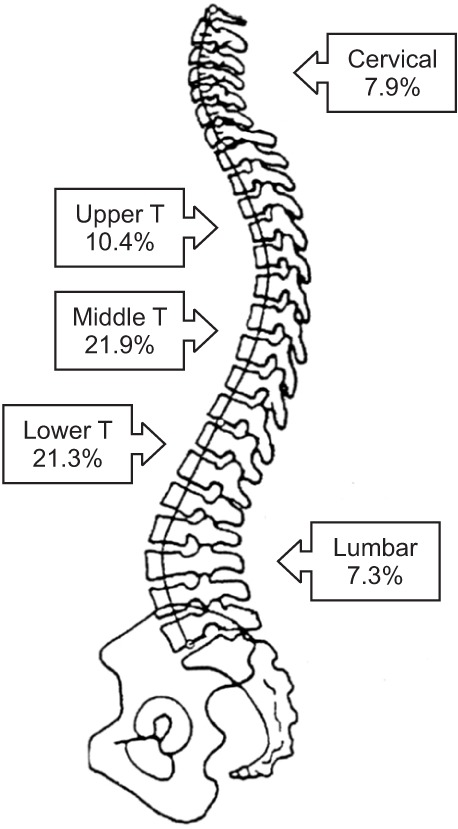 | Fig. 4Prevalence of diffuse idiopathic skeletal hyperostosis based on whole spine computed tomography in five divided spinal regions. T: thoracic.
|
Comorbidity with OPLL or OLF
In DISH patients, OLF was observed in 22.5% and OPLL was observed in 37.5%. The ICCs for intra- and interobserver reliability were 0.841 (p = 0.00) and 0.756 (p = 0.00), respectively for all quantitative measurements, indicating that the results had good repeatability and reproducibility.
Go to :

DISCUSSION
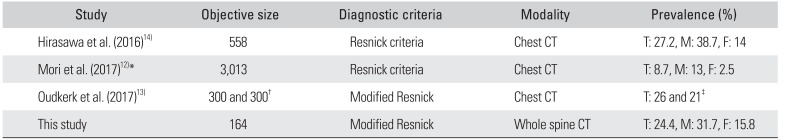
There are several previous studies that described and analyzed DISH by using plain films or CT scans.
12131415161718192021) Hirasawa et al.
14) first reported DISH evaluated by CT in 2016. Including this, there are three studies that used CT for evaluation of DISH in the literature (
Table 2).
121314) Oudkerk et al.
13) presented modified Resnick criteria for the diagnosis of DISH on chest CT (
Table 1). The authors reported that the modified Resnick criteria to identify DISH on CT led to moderate to excellent agreement between observers with different degrees of experience and expertise. In the present study, the modified Resnick criteria were used to diagnose DISH using whole spine CT. Bone setting of CT was used to prevent false positives and negatives. The angle formed by an osteophyte in relation to vertebral bodies was assessed to diagnose DISH; the angle should be larger than 90° to differentiate flowing ossification from bridging degenerative osteophytes. DISH with mild to moderate disc degenerative changes was also diagnosed as DISH. Hirasawa et al.
14) reported that CT was more reliable than the plain film in the diagnosis of DISH. In that report, the prevalence of DISH based on CT was 27.1%, which was surprisingly higher than that based on X-ray (17.6%). Although we did not compare CT with X-ray, the prevalence of DISH based on whole spine CT in the present study was as high as 24.4%, similar to that in the study of Hirasawa et al.
14) However, Mori et al.
12) presented the prevalence of thoracic DISH based on chest CT in a Japanese population as 8.7%, which is comparable to that in the study of Kagotani et al.
18) diagnosed by standard radiographs. Based on these studies, CT does not appear to have advantages over standard radiography in the diagnosis of DISH except for the evaluation of concomitant OLF, OPLL, and spine fractures.
12) The difference in the prevalence of DISH between the two previous CT-based studies could be due to the lack of established criteria. The authors
12) counted only the lesions with complete bony bridge, whereas the lesions with a spur-like incomplete bridge were excluded. However, Kuperus et al.
22) presented that there was lack of consensus on the diagnosis of (early) DISH and consecutive phases of new bone formation that characterize DISH should be considered as diagnosis criteria of DISH. Yaniv et al.
23) suggested the importance of early detection of DISH through the natural course of bridging osteophyte formation over 10 years. We also included cases with incomplete flowing bridge ossification in this study if the ossification corresponded to the modified Resnick criteria.
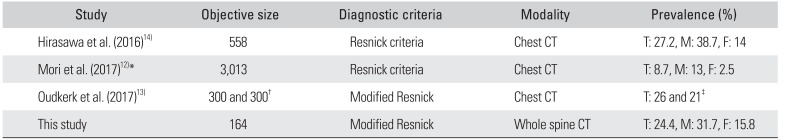
Table 2
Previous Reports of DISH Based on CT
|
Study |
Objective size |
Diagnostic criteria |
Modality |
Prevalence (%) |
|
Hirasawa et al. (2016)14)
|
558 |
Resnick criteria |
Chest CT |
T: 27.2, M: 38.7, F: 14 |
|
Mori et al. (2017)12)*
|
3,013 |
Resnick criteria |
Chest CT |
T: 8.7, M: 13, F: 2.5 |
|
Oudkerk et al. (2017)13)
|
300 and 300†
|
Modified Resnick |
Chest CT |
T: 26 and 21‡
|
|
This study |
164 |
Modified Resnick |
Whole spine CT |
T: 24.4, M: 31.7, F: 15.8 |

The prevalence of DISH in previous publications was quite variable ranging from 2.6% to 28%
12131415161718192021) due to unestablished criteria of DISH and various investigative modalities such as chest X-ray, whole spine X-ray, chest CT and thoracolumbar CT. With technological development, CT has become more available, and its use for the detection DISH is expected to grow in the near future. Therefore, consensus on the criteria of DISH based on CT should be established. The overall prevalence of DISH was higher over the age of 50 years and twice in males than females in the present study. These results are similar to those of most previous reports which documented a significant predisposition to DISH in male and elderly individuals.
71718) In this study, the prevalence of DISH in patients in their seventh, eighth, and ninth decades was lower than that in previous studies. Since this result was obtained from a small number of cases (< 30 per each age decade), we could not compare the prevalence of DISH among different age groups. However, we could observe a strong positive correlation between the age decade and prevalence of DISH.
DISH of the upper thoracic region and cervical thoracic junction could not be investigated by chest X-ray in the past. Mori et al.
12) reported that there was no thoracic DISH localized in only the higher thoracic region above T5 among 261 DISH cases. In the present study, however, there was one case of DISH localized only in the cervical region (
Fig. 2) and one case of DISH localized only in the upper thoracic region (
Fig. 3) among 40 cases of DISH. We could also identify comorbidities of typical DISH and atypical DISH (cervical or lumbar DISH) by using whole spine CT (
Fig. 4). Among typical DISH cases, the prevalence of cervical DISH was 43% (17 of 39 cases) and that of lumbar DISH was 31% (12 of 39 cases). Therefore, we believe whole spine CT could be useful for the diagnosis of DISH in these atypical regions.
Spinal ligament ossification syndrome, which includes OPLL, OLF and DISH, is a multifactorial disease with genetic and environmental factors. Previous studies reported on the association of OPLL/OLF and DISH. The prevalence of OPLL is higher in Asians than Caucasians. The prevalence of cervical OPLL is reported to range from 0.6% to 2.2% in the Korean population.
24) In the present study, the prevalence of OPLL and OLF in DISH patients was high, 37.5% and 22.5%, respectively. In the study of Mori et al.,
12) the prevalence of OLF in DISH was similar and that of OPLL was lower (38% and 7.7%, respectively). Because only thoracic OPLL was included in the study of Mori et al., the prevalence of OPLL in DISH was lower than that of the present study, which included not only thoracic but also cervical OPLL.
There were several limitations in the present study. First, the sample size (164 CT scan images) was relatively small. However, we could enroll at least over 20 subjects per each age decade evenly. Furthermore, we just investigated the overall prevalence and location of DISH without making comparison among age groups. A prospective study with a large number of whole body CT images would help estimate a more accurate incidence of DISH in the future. Second, we did not compare reliability of whole spine CT and whole spine X-ray. We could not get whole spine X-ray images in most of the subjects due to the nature of the retrospective study. Third, we could not evaluate the clinical correlations with metabolic syndrome, cardiovascular disease and low back pain in DISH. The last limitation is that this was a cross-sectional retrograde study and we could not assess progressive characteristics of DISH according to aging process.
In conclusion, the incidence of DISH diagnosed by using whole spine CT was higher than expected. DISH in the atypical region (cervical or lumbar spine) could occur without typical thoracic DISH. Whole spine CT can be a valuable modality to evaluate the prevalence and location of DISH in the whole spine level and comorbidity rates of OLF and OPLL.
Go to :

ACKNOWLEDGEMENTS
This study was presented in part at the Annual Meeting of the Korean Orthopaedic Association, Seoul, Korea, in October 19, 2017.
Go to :

Notes
Go to :

References
1. Forestier J, Rotes-Querol J. Senile ankylosing hyperostosis of the spine. Ann Rheum Dis. 1950; 9(4):321–330. PMID:
14800245.

2. Resnick D, Niwayama G. Radiographic and pathologic features of spinal involvement in diffuse idiopathic skeletal hyperostosis (DISH). Radiology. 1976; 119(3):559–568. PMID:
935390.

3. Mader R, Novofestovski I, Adawi M, Lavi I. Metabolic syndrome and cardiovascular risk in patients with diffuse idiopathic skeletal hyperostosis. Semin Arthritis Rheum. 2009; 38(5):361–365. PMID:
18304611.

4. Sinha R, Aggarwal N, Dutta S, Choudhury A, Ghosh SK, Guha D. Diffuse idiopathic skeletal hyperostosis involving cervical and lumbar spine presenting with dysphagia: a case report. Iran J Otorhinolaryngol. 2017; 29(93):233–236. PMID:
28819624.
5. Moriwaki M, Hase H, Fujioka S, et al. Prolonged dysphagia due to a combination of cerebral hemorrhage and diffuse idiopathic skeletal hyperostosis: a case report. NMC Case Rep J. 2016; 3(3):75–79. PMID:
28664003.

6. Yamada K, Toyoda H, Terai H, Takahashi S, Nakamura H. Spinopelvic alignment of diffuse idiopathic skeletal hyperostosis in lumbar spinal stenosis. Eur Spine J. 2014; 23(6):1302–1308. PMID:
24413742.

7. Mader R, Verlaan JJ, Buskila D. Diffuse idiopathic skeletal hyperostosis: clinical features and pathogenic mechanisms. Nat Rev Rheumatol. 2013; 9(12):741–750. PMID:
24189840.

8. Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J. 2009; 18(2):145–156. PMID:
18791749.

9. Kobayashi H, Otani K, Watanabe K, et al. Vertebral fracture at the caudal end of a surgical fusion for thoracic vertebral fracture in a patient with diffuse idiopathic skeletal hyperostosis (DISH). Fukushima J Med Sci. 2017; 63(2):112–115. PMID:
28680006.

10. Vaishya R, Vijay V, Nwagbara IC, Agarwal AK. Diffuse idiopathic skeletal hyperostosis (DISH): a common but less known cause of back pain. J Clin Orthop Trauma. 2017; 8(2):191–196. PMID:
28721001.
11. Katzman WB, Huang MH, Kritz-Silverstein D, Barrett-Connor E, Kado DM. Diffuse idiopathic skeletal hyperostosis (DISH) and impaired physical function: the Rancho Bernardo Study. J Am Geriatr Soc. 2017; 65(7):1476–1481. PMID:
28369706.
12. Mori K, Kasahara T, Mimura T, Nishizawa K, Nakamura A, Imai S. Prevalence of thoracic diffuse idiopathic skeletal hyperostosis (DISH) in Japanese: results of chest CT-based cross-sectional study. J Orthop Sci. 2017; 22(1):38–42. PMID:
27697426.

13. Oudkerk SF, de Jong PA, Attrach M, et al. Diagnosis of diffuse idiopathic skeletal hyperostosis with chest computed tomography: inter-observer agreement. Eur Radiol. 2017; 27(1):188–194. PMID:
27097788.

14. Hirasawa A, Wakao N, Kamiya M, et al. The prevalence of diffuse idiopathic skeletal hyperostosis in Japan: the first report of measurement by CT and review of the literature. J Orthop Sci. 2016; 21(3):287–290. PMID:
26948246.
15. Toyoda H, Terai H, Yamada K, et al. Prevalence of diffuse idiopathic skeletal hyperostosis in patients with spinal disorders. Asian Spine J. 2017; 11(1):63–70. PMID:
28243371.

16. Weinfeld RM, Olson PN, Maki DD, Griffiths HJ. The prevalence of diffuse idiopathic skeletal hyperostosis (DISH) in two large American Midwest metropolitan hospital populations. Skeletal Radiol. 1997; 26(4):222–225. PMID:
9151370.

17. Kim SK, Choi BR, Kim CG, et al. The prevalence of diffuse idiopathic skeletal hyperostosis in Korea. J Rheumatol. 2004; 31(10):2032–2035. PMID:
15468371.
18. Kagotani R, Yoshida M, Muraki S, et al. Prevalence of diffuse idiopathic skeletal hyperostosis (DISH) of the whole spine and its association with lumbar spondylosis and knee osteoarthritis: the ROAD study. J Bone Miner Metab. 2015; 33(2):221–229. PMID:
24623190.

19. Cassim B, Mody GM, Rubin DL. The prevalence of diffuse idiopathic skeletal hyperostosis in African blacks. Br J Rheumatol. 1990; 29(2):131–132. PMID:
2322769.
20. Kiss C, O'Neill TW, Mituszova M, Szilagyi M, Poor G. The prevalence of diffuse idiopathic skeletal hyperostosis in a population-based study in Hungary. Scand J Rheumatol. 2002; 31(4):226–229. PMID:
12369655.

21. Westerveld LA, van Ufford HM, Verlaan JJ, Oner FC. The prevalence of diffuse idiopathic skeletal hyperostosis in an outpatient population in The Netherlands. J Rheumatol. 2008; 35(8):1635–1638. PMID:
18528963.
22. Kuperus JS, de Gendt EE, Oner FC, et al. Classification criteria for diffuse idiopathic skeletal hyperostosis: a lack of consensus. Rheumatology (Oxford). 2017; 56(7):1123–1134. PMID:
28371859.

23. Yaniv G, Bader S, Lidar M, et al. The natural course of bridging osteophyte formation in diffuse idiopathic skeletal hyperostosis: retrospective analysis of consecutive CT examinations over 10 years. Rheumatology (Oxford). 2014; 53(11):1951–1957. PMID:
24158753.

24. Kang MS, Lee JW, Zhang HY, Cho YE, Park YM. Diagnosis of cervical OPLL in lateral radiograph and MRI: is it reliable. Korean J Spine. 2012; 9(3):205–208. PMID:
25983816.

Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download