Abstract
Orbitofacial angioedema is one of the common contrast-induced adverse reactions. The symptoms are recognized, based on the patient's clinical complaints. Based on prior research findings, there were no reports about contrast-induced orbitofacial angioedema that was confirmed on image findings. The researchers herein report on contrast-induced orbitofacial angioedema presented on enhanced computed tomography, following intravenous administration of iodine contrast media.
Contrast-induced localized orbitofacial edema is one of the moderate contrast-induced adverse reactions. Adverse reaction occurs in less than 1% of patients, as low as 0.35%, according to a recent study based on domestic data. The systems range from mild to severe cardiopulmonary collapse (1). Mostly, there are mild symptoms such as skin rashes, flushing, or mild urticaria (2). These mild symptoms generally do not require treatment with self-limiting features (2), but proper management must be done should the symptoms worsen (2).
The researchers experienced a rare case of contrast-induced localized orbitofacial edema appearring on enhanced computed tomography (CT). The orbitofacial swelling on an enhanced CT image was the result of a contrast-induced adverse reaction, because the findings had not manifested before intravenous administration of contrast agent, and it was naturally resolved without treatment.
This study was approved by the Institutional Review Board, and the requirement for informed consent was waived.
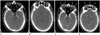
A 25-year-old man underwent a neck CT examination for an annual follow-up, after total thyroidectomy for papillary thyroid cancer 3 years ago. The patient did not experience any other abnormal complications, after contrast-enhanced neck CT examination 19 months ago. He had no predisposing factors for the adverse effects, caused by the contrast agents and he did not experience any contrast-induced adverse reactions in previous contrast agent injections. A 70 mL of low-osmolar iodinated contrast media (ICM) was intravenously injected at a rate of 2 mL/sec. A post-contrast CT examination was performed 60 seconds, after the start of the intravenous ICM injection. The post-contrast images were obtained after 60 seconds of contrast injection. On the pre-contrast images, there were no demonstrable abnormal findings in the scanned area (Fig. 1A, B). On the contrary to pre-contrast images, however, enhancing soft tissue lesions with swelling appeared at both forehead, eyelids, and preseptal space of both orbits on post-contrast images (Fig. 1C, D).
Despite the orbitofacial swelling found on CT images, the patient did not complain of any clinical symptoms after CT scan, and the edema around the eyes and forehead improved the following day.
Eventually, it was found that the abnormal findings were caused by the contrast-induced adverse reactions, because of their immediate appearance just after the intravenous administration of contrast agent and its self-limited course.
In the department of radiology, iodine-based contrast agents are important medicines, that are widely used in radiography and CT imaging for better monitoring of internal organs, blood vessels, abnormal tissues, and for therapeutic purposes in interventional procedures. They are usually safe and adverse effects are generally mild and self-limited, but can be life-threatening (2).
Most acute adverse reactions are mild symptoms and usually do not need treatment (3). Mild angioedema presents as localized facial swelling but rarely, severe respiratory distress and cardiopulmonary arrest can occur, when angioedema involves the upper respiratory systems (3). In one study about acute allergic reactions related to intravenously administered nonionic ICM, mild localized facial edema occurred in 15 of 418 mild reactions (3.5%), and moderate facial or laryngeal edema occurred in 52 of 116 moderate adverse reactions (44.8%) (4).
Angioedema is abrupt swelling of the skin, mucous membranes, or both. The swelling is non-pitting, erythematous, or skin-colored. It may affect any part of the body and the most commonly affected sites are the periorbital area and lips (5). In most cases, contrast-induced angioedema presents as mild symptoms like localized facial or periorbital edema, and is usually self-limited. It normally subsides around 24 hours, without staining or discoloration of the skin, unless vigorous rubbing and scratching occurs. Relapses are common and unpredictable with repetitive exposures or exposures to cross-reactive substances (5). Diagnosis of acute facial or periorbital angioedema depends on the patient's history, principally on contrast-induced angioedema. Swelling after the administration of an iodine contrast agent compared with the precontrast scan, strongly suggests contrast-induced angioedema. Other factors associated with angioedema should be considered including foods, drugs especially nonsteroidal anti-inflammatory drugs and angiotensin-converting-enzyme inhibitors, infection, and exercise (56).
Rarely, life-threatening respiratory failure, due to contrast-induced angioedema occurs when the upper airway is involved. Facial or neck swelling with subcutaneous fat stranding with narrowing of the upper airway and tongue swelling is recognized on CT images. The swelling is usually diffuse, but can be focal or asymmetric. As mentioned above, clinical history is important in diagnosing the iodine contrast media induced angioedema, imaging findings, laboratory data, clinical course, and laryngoscopy should also be considered to exclude other causes of obstruction (7).
When a contrast-induced adverse reaction occurs, the contrast should be discontinued and intravenous assessment must be maintained in all cases. The priority must be to secure the airway, if the upper respiratory tract is involved. Other treatments include subcutaneous or intramuscular administration of adrenaline, intramuscular or intravenous administration of diphenhydramine that is helpful for reducing the edema, and hydrocortisone or solumedrol given intravenously, which may reduce the possibility of relapse (5).
Several articles reported that orbital edema is caused by adverse events of ICM (5689). In these articles, the orbital edema was first recognized by clinical symptoms, not by images, like in this study. From the researchers' knowledge, there were no prior reports of contrast-induced orbital and facial edema, that were identified by images. In most cases, patients complain of specific symptoms such as pulsating sensation of the involved area, swelling, or even blindness due to compressive optic neuropathy, when severe orbital edema occurs. Clinicians recognize the adverse reactions and an imaging study follows. In this case, the patient did not complain of any symptoms associated with orbitofacial edema, and the adverse reactions was diagnosed only by the CT images. It is very important for future follow ups to find out whether the contrast-induced adverse reaction that occurred in this study, because the history of previous adverse reaction is one of the risk factors of adverse reactions caused by intravenous administration of nonionic ICM (1).
It is very important to recognize the image findings of the contrast-induced orbitofacial angioedema, especially in case the patients do not exhibit any symptoms, because there are many factors associated with it. Cutaneous swelling and enhancement after administration of contrast media compared with precontrast CT is an important finding of contrast-induced angioedema. Imaging findings, clinical presentations, patients' past history, and laboratory findings should be all carefully considered for exact diagnosis and appropriate management.
Figures and Tables
 | Fig. 1CT findings of orbitofacial angioedema during enhanced CT scanning in a 25-year-old female.
A, B. No evidence of soft tissue lesion in both eyelid and both orbital preseptal space is noted in precontrast CT image.
C, D. Marked soft swelling with enhancement (arrows) is observed in the both the eyelid, orbital preseptal space (C) and the forehead (D) in postcontrast enhanced CT image, taken 60 seconds after administration of contrast media.
CT = computed tomography
|
References
1. Bae K, Lee SM, Ha JY, Jeon KN, Moon JI, Choi BH, et al. Adverse drug reactions to CT contrast media in South Korea: incidence and risk factors. J Korean Soc Radiol. 2016; 75:41–48.

2. Andreucci M, Solomon R, Tasanarong A. Side effects of radiographic contrast media: pathogenesis, risk factors, and prevention. Biomed Res Int. 2014; 2014:741018.

3. Morcos SK, Thomsen HS. Adverse reactions to iodinated contrast media. Eur Radiol. 2001; 11:1267–1275.

4. Wang CL, Cohan RH, Ellis JH, Caoili EM, Wang G, Francis IR. Frequency, outcome, and appropriateness of treatment of nonionic iodinated contrast media reactions. AJR Am J Roentgenol. 2008; 191:409–415.

5. Kulthanan K, Jiamton S, Boochangkool K, Jongjarearnprasert K. Angioedema: clinical and etiological aspects. Clin Dev Immunol. 2007; 2007:26438.

6. Kaplan AP, Greaves MW. Angioedema. J Am Acad Dermatol. 2005; 53:373–388. quiz 389-392.
7. Ishigami K, Averill SL, Pollard JH, McDonald JM, Sato Y. Radiologic manifestations of angioedema. Insights Imaging. 2014; 5:365–374.

8. Sharma S, Aggarwal S. Unilateral orbital edema following the intravascular injection of contrast medium. Clin Radiol. 1989; 40:108.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download