Dear Editor:
The classic presentation of acquired dermal melanocytosis (ADM) involves facial lesions in Asian women. However, extrafacial ADM can occur in rare cases, including a form confined to the hands. Here, we present a case of ADM confined to the hand and review previously published cases. A 40-year-old Korean woman presented with bluish pigmentation on the left hand. The lesion first started on the dorsum of the hand during her elementary school years, and gradually extended to the palm. She is ambidextrous, and denied any history of preceding trauma, inflammation, or occupational exposure to chemicals. Physical examination revealed a brown-to-blue pigmentation predominantly on the knuckle area of the left hand (Fig. 1A), and slate-gray spots mainly on the palmar creases of the same hand (Fig. 1B). No other pigmentation was evident on the skin or mucous membranes. Skin biopsy was done on the palm. It revealed scattered spindle-shaped cells with melanin granules and melanophages in the upper-to-middle dermis, especially around superficial blood vessels (Fig. 1C). Based on these findings, the case was diagnosed as ADM. Other differential diagnosis includes ectopic Mongolian spots and plaque-type blue nevi. They are both congenital dermal melanocytosis that may present as bluish macules of a hand. However, these lesions show deeper and more widely scattered distribution of the melanocytes. Postinflammatory hyperpigmentation may also show dermal melanosis, but it accompanies epidermal melanosis which is not the feature of our case.
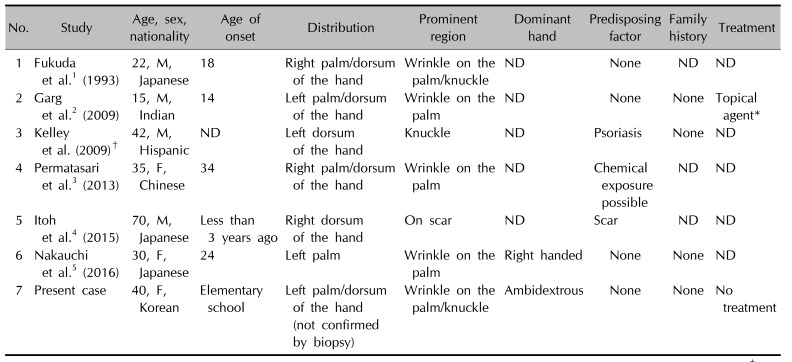
This case is the seventh reported case of ADM confined to the hand (Table 1)12345. Previous cases comprised Asians, a Hispanic and an Indian, all with a skin color of Fitzpatrick skin type 3 or more. Sex predilection was not evident. Interestingly, the pigmentation occurred on only one hand, predominantly on the palmar creases and/or knuckle area in all reported cases of ADM confined to the hand. Although, we couldn't confirm the diagnosis of ADM for dorsum lesion, it was clinically very similar to other ADM cases affecting dorsum area. Three patients had predisposing factors: previous chemical exposure3, a history of psoriasis, and a surgical scar4. No family history was noted in any of the cases. The pathophysiology of ADM remains unclear. Reactivation of preexisting dormant dermal melanocytes by triggering factors such as local trauma, inflammation, or exposure to chemicals is one hypothesis3. Although four cases including our patient did not have obvious triggering factors, the affected area supports this hypothesis. The knuckle area is prone to trauma. Palmar creases are an intertriginous area where chemical-dissolved-sweat can easily accumulate and be absorbed with an occlusive effect. One puzzling fact is that the affected hand was not the dominant hand in one case5. This may imply that the cause of ADM of the hand is multifactorial.
In conclusion, ADM confined to hand may be a new form of ADM that predominantly occurs in patients with darker skin without sex predilection, and has a similar distribution of the lesion. Further case reports on ADM confined to the hand may help elucidate the etiology of this rare condition.
References
1. Fukuda M, Kitajima J, Fushida H, Hamada T. Acquired dermal melanocytosis of the hand: a new clinical type of dermal melanocytosis. J Dermatol. 1993; 20:561–565. PMID: 8227712.

2. Garg T, Ramchander , Srihar R, Gupta TP. Acquired dermal melanocytosis involving the hand. Australas J Dermatol. 2009; 50:72–73. PMID: 19178500.
3. Permatasari F, Zhou BR, Luo D. Late-onset acquired dermal melanocytosis on the hand of a Chinese woman. Indian J Dermatol Venereol Leprol. 2013; 79:269.

4. Itoh E, Nakahara T, Furue M. Injury-induced acquired dermal melanocytosis arising on an operation scar. J Dermatol. 2015; 42:434–435. PMID: 25703067.

5. Nakauchi E, Oka M, Fukumoto T, Sakaguchi M, Nishigori C. Acquired dermal melanocytosis confined to the palm with a review of published cases of acquired dermal melanocytosis on the hands. J Dermatol. 2016; 43:701–705. PMID: 26703756.

Fig. 1
(A) Dorsum of the patient's left hand. Brown-to-blue pigmentation predominantly appears on the third to fifth metacarpophalangeal joint area. (B) The palm of the patient's left hand. Slate-gray spots predominantly appear on the palmar creases (black arrow) and the wrinkles of the fourth and fifth fingers. (C) A biopsy specimen from the pigmented palmar crease. Spindle-shaped cells with melanin granules and macrophages are shown around small blood vessels (H&E, ×100).
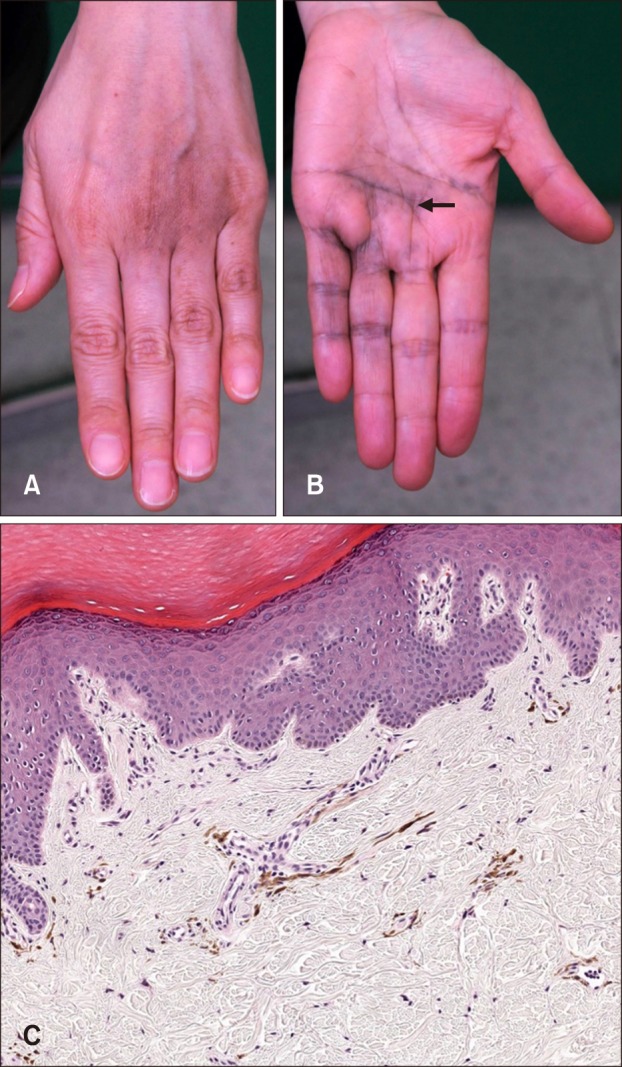
Table 1
Summary of reported cases of acquired dermal melanocytosis restricted to the hand
| No. | Study | Age, sex, nationality | Age of onset | Distribution | Prominent region | Dominant hand | Predisposing factor | Family history | Treatment |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Fukuda et al.1 (1993) | 22, M, Japanese | 18 | Right palm/dorsum of the hand | Wrinkle on the palm/knuckle | ND | None | ND | ND |
| 2 | Garg et al.2 (2009) | 15, M, Indian | 14 | Left palm/dorsum of the hand | Wrinkle on the palm | ND | None | None | Topical agent* |
| 3 | Kelley et al. (2009)† | 42, M, Hispanic | ND | Left dorsum of the hand | Knuckle | ND | Psoriasis | None | ND |
| 4 | Permatasari et al.3 (2013) | 35, F, Chinese | 34 | Right palm/dorsum of the hand | Wrinkle on the palm | ND | Chemical exposure possible | ND | ND |
| 5 | Itoh et al.4 (2015) | 70, M, Japanese | Less than 3 years ago | Right dorsum of the hand | On scar | ND | Scar | ND | ND |
| 6 | Nakauchi et al.5 (2016) | 30, F, Japanese | 24 | Left palm | Wrinkle on the palm | Right handed | None | None | ND |
| 7 | Present case | 40, F, Korean | Elementary school | Left palm/dorsum of the hand (not confirmed by biopsy) | Wrinkle on the palm/knuckle | Ambidextrous | None | None | No treatment |




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download