Dear Editor:
Nevus sebaceous (NS) is a common congenital hamartoma which presents as a well-demarcated skin-colored to yellowish alopecic patch. Numerous secondary tumors can arise within NS, including trichoblastoma, syringocystadenoma papilliferum (SCAP), trichilemmoma, and such malignant tumors as squamous cell carcinoma (SCC)1.
A 47-year-old male patient complained of a congenital flesh-colored plaque on the vertex of the scalp (Fig. 1A). On physical examination, the lesion showed a verrucous surface and measured 2.0 cm and 1.5 cm in the long and short diameter, respectively. Partial incisional biopsy was performed under the impression of NS. Histopathologic studies revealed typical features of NS including papillomatosis and increased number of sebaceous glands (Fig. 1B). We also observed the typical features of SCAP such as opening to the surface, apocrine decapitation secretion, and surrounding plasma cell infiltration (Fig. 1C, D). We also noticed a group of atypical squamous cells with peripheral palisading pattern (Fig. 1E) which were strongly stained with p63 and cytokeratin. As SCC was suspected, the residual tumor was completely removed by Mohs micrographic surgery. In addition to the previously observed features (Fig. 2A, B), lesions suspicious for malignancy showed abrupt keratinization with no recognizable granular layer (Fig. 2C). Ki-67 index was increased and staining with epithelial membrane antigen (EMA) showed a negative result. Furthermore, collagens were stained positive with periodic acid–Schiff (PAS) and were diastase labile (Fig. 2D, E). Taking these findings into account, we concluded this malignancy as trichilemmal carcinoma (TC). The patient has shown no signs of local recurrence for 4 months.
TC is a rare malignant tumor of adnexal tissue origin accompanied by outer root sheath (ORS) differentiation. Notable histologic features are neoplastic cells with atypical nuclei, high mitotic index, trichilemmal keratinization, pushing lower border, and peripheral palisading of columnar clear cells2. Trichilemmal keratinization is defined as presence of abrupt keratinization without keratohyaline granules as seen in the ORS of a normal hair follicle. The clear cells in TC have glycogens which are stained positive with PAS and are diastase sensitive. Diverse cytokeratin stains show positive results, although no single cytokeratin is solely specific to TC. Other helpful immunohistochemical studies are p53, Ki-67, c-erb-B2, and p6323.
TC should be distinguished from tumors composed of clear cells. It can be difficult to differentiate clear cell SCC from TC, especially without a immunohistochemical marker specific for ORS differentiation2. Nonetheless, EMA stain can be attempted as SCCs often show positive results. When distinguishing from clear cell porocarcinoma and hidradenocarcinoma, accentuation with diastase-PAS, EMA, and carcinoembryonic antigen stain can help rule out TC.
In contrast to TC, whose coexistence with other tumors is unusual, there are countless reports on NS with secondary neoplasms1. Upon review of the previous literature, we could not identify an article on concurrent presentation of TC and SCAP without underlying NS. For this reason we assumed that TC in our case originated from NS, which were seldom reported before45. Our report implies that TC and SCAP can arise simultaneously within the preexisting NS.
Figures and Tables
Fig. 1
(A) Flesh-colored plaque with mildly verrucous surface on the scalp. (B) Papillomatosis is accompanied by many sebaceous glands (H&E, ×40). (C, D) More prominent papillomatosis is seen on the left. On the right are opening to the epidermis layer and several cystic invaginations extending into the dermis. Close-up view of the lower portion reveals features of decapitation secretion including cellular debris in the lumina (H&E; C: ×40, D: ×200). (E) A group of atypical squamous cells with peripheral palisading pattern within epidermis (H&E, ×100).
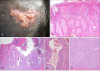
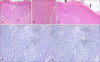
Fig. 2
(A) Although the tumor is mainly intraepidermal, invasion with pushing border is seen at the lower portion (H&E, ×40). (B) Close-up view of the tumor cells reveals cells with pleomorphic nuclei (H&E, ×200). (C) The normal epidermis on the right (thin arrow) shows keratinization with an intact granular layer. The tumor on the left (thick arrow) shows trichillemmal keratinization, or abrupt keratinization without recognizable granular layer (H&E, ×100). (D) The cytoplasm of the tumor cells is stained positive with periodic acid–Schiff (PAS) stain (×400). (E) These tumor cells were diastase labile, resulting in diminished degree of staining after PAS diastase application (×400).
References
1. Idriss MH, Elston DM. Secondary neoplasms associated with nevus sebaceus of Jadassohn: a study of 707 cases. J Am Acad Dermatol. 2014; 70:332–337.

2. Hamman MS, Brian Jiang SI. Management of trichilemmal carcinoma: an update and comprehensive review of the literature. Dermatol Surg. 2014; 40:711–717.
3. Kim YH, Lee YK, Choi KW, Lee CY, Kim KH. A case of trichilemmal carcinoma treated with mohs micrographic surgery. Ann Dermatol. 2008; 20:157–161.

4. Noh Y, Yoon TY. Nevus sebaceus associated with trichilemmoma, trichilemmal carcinoma and trichoblastoma. Korean J Dermatol. 2004; 42:443–446.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download