Abstract
Background
Labial melanotic macules (LMMs) are benign pigmented lesions that usually take the shape of flat asymmetrical macules with tan-brown to black color and variable size. Whereas the dermoscopic features of other pigmented skin lesions have been relatively well described, little is known about LMMs.
Objective
To describe the dermoscopic features and find typical and schematic dermoscopic patterns in LMMs.
Methods
A retrospective dermoscopic study was conducted on 80 lesions with histopathologically proved LMMs.
Results
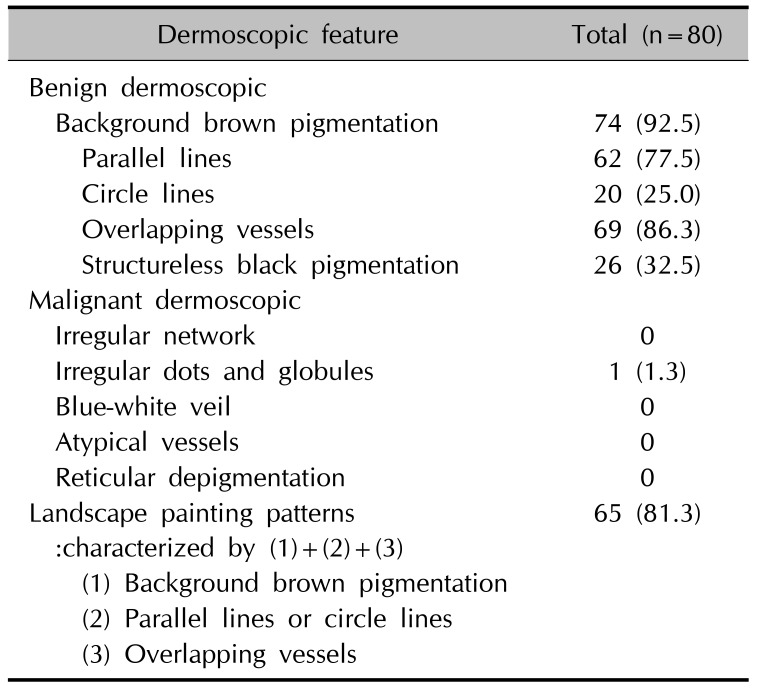
We described and defined, for the first time to our knowledge, landscape painting patterns found in 65 of 80 melanotic lesions (81.3%), characterized by parallel lines or circle lines, overlapping vessels with background brown pigmentation. The background brown pigmentations were observed in 74 of 80 lesions (92.5%), the parallel lines in 62 (77.5%), the circle lines in 20 (25.0%), and overlapping vessels in 69 (86.3%). The structureless black pigmentations were only presented in 26 of 80 (32.5%).
Labial melanotic macules (LMMs) are benign pigmented lesions that are commonly encountered in daily practice. LMMs are asymptomatic, discrete, tan-brown to black lesions, which usually less than 1 cm in maximum dimension12. Histopathologically, LMM represent increased levels of melanin pigments in the basal epidermal layer with normal or slightly more than normal melanocyte numbers12.
The diagnostic accuracy of dermoscopy for pigmented skin lesions has been widely demonstrated, but despite this, its merits for the diagnosis of LMM have not been well investigated3456. Furthermore, these reports did not well characterize the unique dermoscopic features of LMM, because it had encompassed entire pigmented lesions on mucocutaneous junction and mucous membrane356. The aim of this retrospective study was to describe and characterize the dermoscopic patterns exhibited by LMM.
The medical records, clinicodermoscopic photographs, and histopathologic slides of 60 patients (80 lesions) treated at the outpatient clinics of two Korean tertiary teaching hospitals (Pusan National University Hospital and Pusan National University Yangsan Hospital) from 2007 to 2015 were retrospectively reviewed. All 80 patients were diagnosed as having LMM based on clinicopathologic findings. Patient genders, ages, and lesion dermoscopic pattern types were retrieved. The following exclusion criteria were applied: 1) Laugier-Hunziker syndrome, neurofibromatosis, McCune-Albright syndrome, Peutz-Jeghers syndrome, LAMB (lentigines, atrial myxomas, mucocutaneous myxomas, and blue nevi) syndrome, and the associated Carney syndrome; 2) Addison diseases; 3) postinflammatory conditions, such as, lichen planus or smoker's melanosis125. Digital dermoscopic images of selected lesions were acquired using a dermoscope (Dermlite II Pro HR equipment, 10×magnification; 3Gen, LLC, Dana Point, CA, USA) attached to a digital camera (Sony Cybershot DSC-W290, 5×optical zoom, 12.1 megapixels; Sony Corporation, Tokyo, Japan). The study was exempted from the requirement for approval by the ethics committee of Pusan National University Hospital (IRB no. H-1703-012-053), and informed consent was obtained from patients included in our study. All the lesions were determined by two independent dermatologists that were experts in dermoscopy and specific patterns were considered present when both observers agreed.
Ten dermoscopic features were described using the terms previously reported for mucocutaneous lesions, but some of these terms were revised; 5 benign features (background brown pigmentation, parallel lines, circular lines, overlapping vessels, and structureless black pigmentation) and 5 malignant features (irregular network, irregular dots and globules, blue-white veil, atypical vessels, and reticular depigmentation)3456.
Eighty LMM lesions of 60 patients (13 males and 47 females; mean age, 49.8 years; range, 12 to 81 years) were included in the present study. Background brown pigmentation was observed by dermoscopy in 74 of these lesions (92.5%). Parallel lines, which appeared as linear or curved streaks running parallel to the skin surface, were observed in 62 (77.5%). Circular lines appearing as round to oval structures were also observed in 20 lesions (25.0%). Overlapping vessels characterized by duplicating erythematous vessels to parallel or circle lines were observed in 69 (86.3%). Structureless black pigmentations appeared as diffuse homogenous black pigmentation or variegated dark brown to black pigmentation (without dots, globules, a pigment network, or streaks) were observed in 26 (32.5%) (Fig. 1, Table 1).
We described the co-presence of three features, that is, background brown pigmentation, parallel lines or circular lines, and overlapping vessels (Fig. 2) were described as ‘landscape painting patterns’ (derived from the Korean landscape masterpiece called ‘A General view of Mt. Geumgangsan’ painted by Jeong Seon in the 18th century). This unique pattern was identified in 65 of the 80 lesions (81.3%). However, only 1 of the 80 lesions exhibited irregular dots and globules suggestive of malignancy. No lesion presented as an irregular network, blue-white veil, atypical vessels, or reticular depigmentation (Table 1).
LMM is a benign pigmented lesions of the mucosa characterized by hyperpigmented basal keratinocytes1. Despite its benign behavior, on clinical grounds the differentiation of LMM may be frequently required from malignant melanoma possibly being characterized by asymmetry, variegated pigmentation from light to dark brown, irregular borders, and large size56. Dermosocpy is an emgerging technique that allows for noninvasive imaging of the skin and mucosa.
However, as far as we know, most of the literature on dermoscopy related to LMM has primarily been focused on integrated analysis of the mucocutaneous lesions including lips, oral cavity, and vulva (not confined to only lips)356. Mannone et al.3 identified three major dermoscopic patterns in benign mucosal melanotic macule, known as parallel pattern, structureless pattern and reticular-like pattern3. Lin et al.5 reported ring-like pattern and its variant (fish scale-like pattern and hyphal pattern) in 20 labial and 4 penile lesions of mucosal melanotic macules. In addition, the previous largest scale study was done by Blum et al.6, which included 60 lesions of LMM. In a total of 140 pigmented mucosal lesions, they found 5 patterns including 67 structureless, 64 lines, 26 circles, 8 globules/clods, and 10 dots. Remarkably, they had presented very simple descriptions that can cause diagnostic confusion6.
Therefore, we performed this study to confirm dermoscopic accuracy in the diagnosis of LMM, and so to obviate the need for biopsies in the lip which is a sensitive part of the body. In comparison with the findings of previous reports356, the unique aspects of our study are larger sample size than before and confined to one disease entity as LMM to achieve detailed observation. In addition, we investigated more diverse dermoscopic features of the pigmentations and vasculature using uniform terminology for delineating these features3456.
In our study, the peculiar dermoscopic features of LMM, that is, landscape painting patterns was presented, and need to be considered as the key diagnostic criteria for LMM. This important feature is supposed to enable correct diagnosis of benign labial lesions and help to allow earlier diagnosis of malignant changes (Fig. 2). In addition, our results indicate a close correlation between dermoscopic patterns and underlying histologic features. The parallel or circle lines represent the melanin pigmentation within basal layer, and the characteristic histologic features of LMM. The overlapping vessels indicated markedly dilated capillaries in rete ridges and the background brown pigmentations can be explained by melanins and melanophages at all levels of the epidermis or the dermis12.
Our study had several limitations. It was an uncontrolled, non-double-blind study. The study did not reflect the variables of age, sex, and the locations and activity of the lesions. In particular, we did not compare the features between LMM and melanoma.
In conclusion, this study clearly shows that dermoscopy can be useful tool for diagnosing LMM, and landscape painting patterns may represent a new dermoscopic clue for the diagnosis of the lesions.
References
1. Ho KK, Dervan P, O'Loughlin S, Powell FC. Labial melanotic macule: a clinical, histopathologic, and ultrastructural study. J Am Acad Dermatol. 1993; 28:33–39. PMID: 8425968.

2. Gupta G, Williams RE, Mackie RM. The labial melanotic macule: a review of 79 cases. Br J Dermatol. 1997; 136:772–775. PMID: 9205516.

3. Mannone F, De Giorgi V, Cattaneo A, Massi D, De Magnis A, Carli P. Dermoscopic features of mucosal melanosis. Dermatol Surg. 2004; 30:1118–1123. PMID: 15274702.

4. Tsunemi Y, Saeki H, Tamaki K. Labial melanotic macule diagnosed by dermoscopy. Acta Derm Venereol. 2008; 88:524–525. PMID: 18779902.

5. Lin J, Koga H, Takata M, Saida T. Dermoscopy of pigmented lesions on mucocutaneous junction and mucous membrane. Br J Dermatol. 2009; 161:1255–1261. PMID: 19673880.

6. Blum A, Simionescu O, Argenziano G, Braun R, Cabo H, Eichhorn A, et al. Dermoscopy of pigmented lesions of the mucosa and the mucocutaneous junction: results of a multicenter study by the International Dermoscopy Society (IDS). Arch Dermatol. 2011; 147:1181–1187. PMID: 21680757.
Fig. 1
(A~C) Pigmented cutaneous lesions located on lip in labial melanotic macules patients (inset). Dermoscopy revealed background brown pigmentation (indicated by red arrow), parallel lines (by purple arrows), circular lines (by blue arrows), and overlapping vessels (by orange arrows).
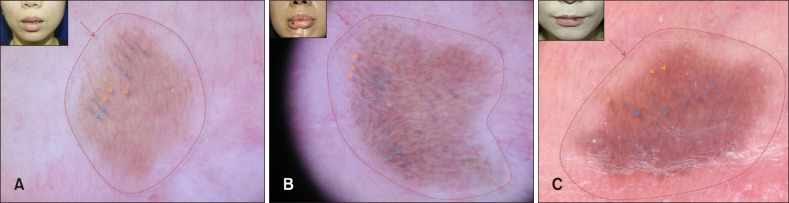
Fig. 2
(A~C) Schematic representations of dermoscopic patterns in patient with labial melanotic macules. (C) The ‘landscape painting pattern’ was derived from the 18th century Korean masterpiece, ‘General view of Mt. Geumgangsan’ by Jeong Seon. (B) The pattern was deemed to be present if the lesion satisfied all three of the following features; background brown pigmentation, parallel lines or circular lines, and overlapping vessels.
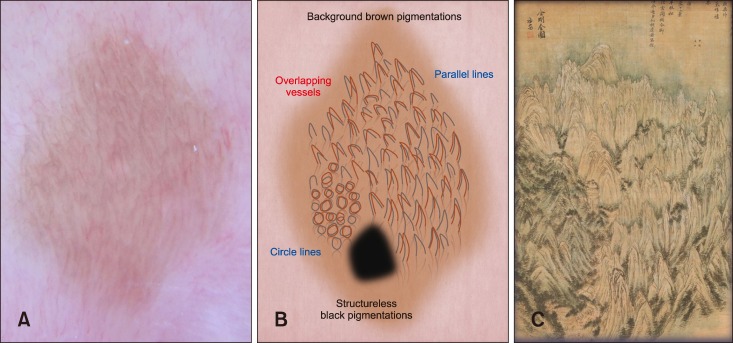
Table 1
Dermoscopic features in the 80 labial melanotic macules lesions




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download