Abstract
Background
Rosacea is a common dermatosis characterized by erythema, telangiectasia, papules and pustules.
Methods
We included 65 rosacea patients and 60 healthy volunteers in the study. The patient and control groups were patch tested with European baseline series and cosmetic series.
Results
A positive reaction to at least 1 allergen in the European standard series was found in 32.3% of rosacea patients and 20.0% of subjects in the control group while the relevant numbers were 30.8% of rosacea patients and 10% of controls with the cosmetic series (p=0.08). In total, we found a positive reaction to at least 1 allergen in 38.5% of patients and 25.0% of controls (p=0.15). We did not find a statistically significant relationship between a positive reaction to 1 allergen in total and the gender, skin type, rosacea type, ocular involvement, age and disease duration. There were more symptoms in patients with a positive reaction to allergens (p<0.001).
Rosacea is a common inflammatory dermatosis characterized by erythema, telangiectasia, papules and pustules that involve the central facial area. There are 4 types as erythematotelengiectatic, papulopustular, phymatous and ocular12. Rosacea is common between the ages of 30 and 40 years. The incidence in Europe and the United States has been reported as 1% to 22%13.
The cause of the disorder is unknown; but the various factors blamed in rosacea etiopathogenesis are innate immunity (antimicrobial peptides), vascular changes, excessive stimulation of the autonomous and sensory nervous system, reactive oxygen species released from neutrophils, ultraviolet radiation, epidermal proteases and microbial factors (Demodex folliculorum, Demodex brevis)124. A positive family history has been found in 30% of the patients. Alcohol, hot beverages, sun exposure, hot and cold weather, wind, moisturizers, cosmetics, physical and emotional stress are triggering factors. These factors play a role in the pathophysiology by activating peripheral sensory nerve endings. Activation of cutaneous nerves, dysfunction of the innate immune system and impairment of epidermal barrier function result in “hypersensitive skin.” Changes in epidermal proteases also play a role in the impairment of the skin barrier function24.
There are many case reports on allergic contact dermatitis against topical drugs in rosacea patients5678. However, there are only a few studies on contact sensitivity in these patients91011121314. In this study we aim to evaluate contact sensitivity against standard and cosmetic allergens in rosacea.
We included 65 rosacea patients aged 18 years of over who attended Department of Dermatology, Eskisehir Osmangazi University Training and Research Hospital and 60 healthy volunteers as a control group. We excluded pregnant or nursing patients, those who had used systemic antihistaminics or topical steroid treatment within 1 week of the test or during the test, those who had used systemic steroids or other immunosuppressive treatment in the last month. We obtained consent from the Eskişehir Osmangazi University Ethics Committee (IRB no. 80558721/154). The volunteers were informed of the study procedures and a signed consent form was obtained before the study.
We used the “European standard series” that contains 30 allergens and the “cosmetic series” that contains 57 allergens (Chemotechnique Diagnostics, Malmo, Sweden), on both the study and control groups using the IQ-Chamber test material (Chemotechnique IQ Chamber®; Chemotechnique Diagnostics). The test units were attached to both sides of the vertebral column (cosmetic series allergens) and to the outer aspect of both arms (European Standard series allergens). The units containing the test substances were removed after 48 hours and the evaluation was performed after waiting for 30 minutes to determine the substances that had caused a positive reaction. The patients were asked to come for follow-up visits after 72 and 96 hours and 7 days. The reactions were assessed as recommended by the “International Contact Dermatitis Research Group”.
Continuous data were presented as mean±standard deviation. Categorical data were presented as percentage (%). The Shapiro-Wilk test was used to determine whether the data conformed to a normal distribution. The Mann-Whitney U test was used to compare groups that did not conform to a normal distribution when there were two groups. We used the Pearson chi-square, Pearson exact chi-square, Yate's chi-square and Fisher exact chi-square analyses when assessing the cross-tables that we created. The IBM SPSS Statistics ver. 21.0 software (IBM Co., Armonk, NY, USA) was used for the analyses. A p-value <0.05 was accepted as the criterion for statistical significance.
We included 65 rosacea patients and 60 healthy volunteers in the study. There were 60 (92.3%) females and 5 (7.7%) males in the rosacea group and 55 (91.7%) females and 5 (8.3%) males in the control group. The mean age was 42.5±12 years in the rosacea group and 43.5±12.9 years in the control group. There was no statistically significant difference between the rosacea and control groups for age or gender.
The disease duration in the rosacea group was 1 to 45 (mean, 9.89) years. The Fitzpatrick's skin type was type I in 26 (40.0%), type II in 29 (44.6%) and type III in 10 (15.4%). Papulopustular rosacea was the most common rosacea type as seen in 42 (64.6%) patients. Erythematotelengiectasic rosacea was present in 21 (32.3%) and phymatous rosacea in 2 (3.1%) patients. Ocular involvement was found in 21 patients (32.3%). The symptoms were itching in 37 (29.6%), burning in 46 (36.8%), tingling in 21 (16.8%), pain in 17 (13.6%), and being unhappy with the appearance in 21 (16.8%) (Table 1).
A positive reaction to at least 1 allergen in the European standard series was found in 21 (32.3%) subjects in the patient group and 12 (20.0%) subjects in the control group while the relevant numbers were 20 (30.8%) and 6 (9.2%) respectively with the cosmetic series (p=0.08). In total, we found a positive reaction to at least 1 allergen in 25 (38.5%) patients in the patient group and 15 (25.0%) in the control group (p=0.15). However, these differences were not statistically significant.
The number of patients with a positive reaction against 1, 2, or 3 allergens in the standard series was significantly higher in the patient group than the control group (p=0.04). Similarly, the number of patients with a positive reaction against 1, 2, 3, or 4 allergens in the cosmetic series was significantly higher in the patient group than the control group (p=0.01). Overall evaluation of the number of allergens with a positive reaction revealed that a positive reaction to 1 allergen was more common in the control group while a positive reaction to 2, 3, and 4 allergens was statistically significantly higher in the patient group (p=0.003) (Table 2).
There was no statistically significant association with a positive reaction to at least 1 allergen in the standard series and gender, skin type, rosacea type, ocular involvement and disease duration in the rosacea patients, while such an association was present with age (p=0.039) and the presence of symptoms (p=0.008). We did not detect a statistically significant association between the presence of a positive reaction to at least 1 allergen in the cosmetic series and the gender, skin type, rosacea type, ocular involvement, age and disease duration in the rosacea patients (p>0.05 for all variables) while there were more symptoms in patients with a positive reaction to allergens (p<0.001).
There was also no statistically significant relationship between a positive reaction to 1 allergen in total (in the standard and cosmetic series) and the gender, skin type, rosacea type, ocular involvement, age and disease duration while there were more symptoms in patients with a positive reaction to allergens (p<0.001).
We found the presence of at least 1 irritant reaction in 18 patients in the rosacea group and 5 subjects in the control group. There was a statistically significantly higher number of irritant reactions in the rosacea patients (p=0.01). But no statistically significant relation was detected between the presence of an irritant reaction and gender, skin type, rosacea type, ocular involvement, the presence of symptoms, age, and disease duration in this group.
The patch test with allergens from the European standard series revealed that allergens with the most common positive reaction in rosacea patients were nickel sulfate (13 patients), textile dye mixture (3 patients), fragrance mixture 2 (2 patients), cobalt chloride (2 patients) and lyral (2 patients). Other allergens with a positive reaction in at least one patient were paraphenylendiamine, epoxy resin, mercaptobenzothiazole, fragrance mixture, quaternium 15, budesonide and thixocortol pivalate. Allergens with a positive reaction in the control group were nickel sulfate (9 patients), textile dye mixture (2 patients) and mercaptobenzothiazole (1 patient). Comparison of the allergens with a positive reaction in the two groups did not show a statistically significant difference (p>0.05) (Table 3).
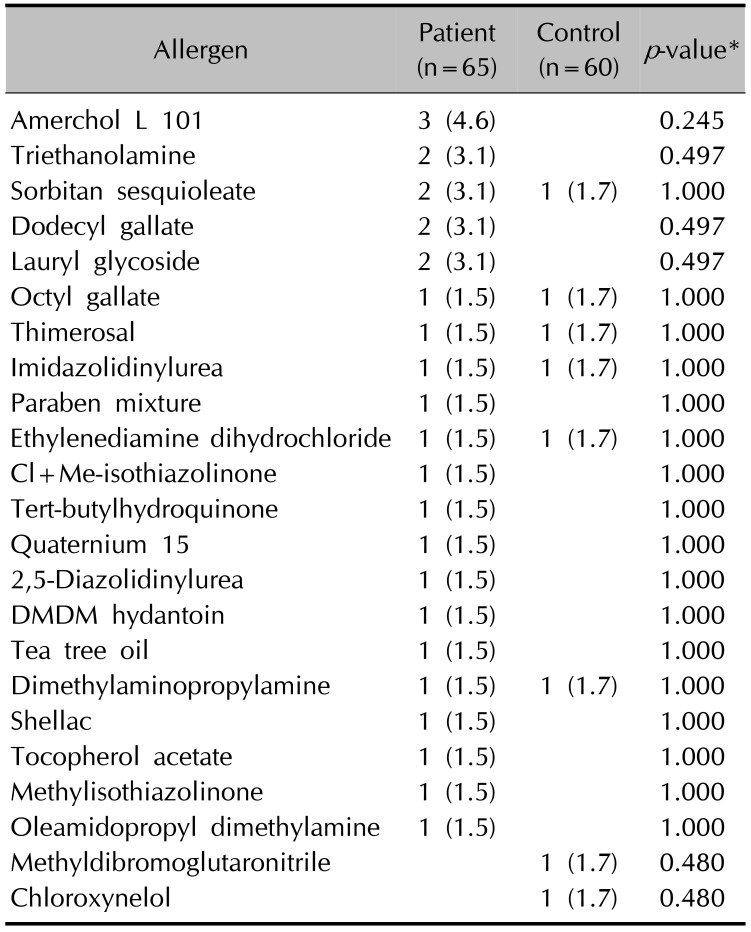
The patch test with the allergens in the cosmetic series revealed the most commonly positive allergens in the rosacea patients to be amerchol L 101 (3 patients), triethanolamine (2 patients), sorbitan sesquiolate (2 patients), dodecyl gallate (2 patients) and lauryl glycoside (2 patients). Allergens that were positive in the control group were sorbitan sesquiolate, octyl gallate, thimerosal, imidazolidinyl urea, ethylenediamine dihydrochloride, methyldibromo glutaronitrile and tetra-chloro 3,5 xylenol in one patient each. There was no statistically significant difference when the allergens with a positive reaction were compared one by one between the two groups (p>0.05) (Table 4).
Rosacea is one of the most common disorders in the general population and has a negative effect on the quality of life15. The etiopathogenesis is not clear but innate immune system and neurovascular dysregulation are thought to be initiating factors. The complex interaction of the innate and acquired immune system, neuroimmune communication, the effect of various cells in the skin and the blood and lymphatic vessels are being considered in later stages2.
Immunohistochemical studies have shown the active immune cells in rosacea to be CD4+T helper (Th1), macrophages and mast cells. Rosacea acts like a Th1-mediated inflammatory skin disorder, especially in the early stages2. Type 4 immunologic reaction and lymphocyte infiltration in the perivascular area have been reported around the follicles containing D. folliculorum. It is also believed that there is a defect in the immune reaction against D. folliculorum in the early stages and that the immune reaction and inflammation increase in the later stages16.
Our main objective was to determine contact sensitization in rosacea patients with the patch test in the study. There was a positive reaction to at least 1 allergen in 38.5% of the patients and 25.0% of the control group subjects. A positive reaction to multiple allergens on the patch test was statistically significantly more common in the rosacea patients. These results indicate that contact sensitization and type 4 reactions are more common in rosacea patients. Although the interaction between the innate immune system and the neuroimmune system is a current popular theory in rosacea pathogenesis, it is obvious that more advanced studies are needed on delayed type hypersensitivity reactions and T-cell mediated inflammation.
Corazza et al.10 evaluated the incidence of contact dermatitis in 29 rosacea patients and found a positive reaction to at least 1 allergen in 41% of the patients. They recommended patch test in patients with a history of exacerbation following the use of cosmetics and topical drugs. Çakmak et al.14 evaluated contact allergy using the patch test with the European standard series and cosmetic series allergens in 25 rosacea patients and 20 healthy control subjects and found a positive reaction to at least 1 allergen in 32% of the patients both with the European standard series and the cosmetic series. In their study, a positive reaction to at least one allergen in the European standard series was present in 30% of the patients while there was no positive reaction in any patient with the cosmetic series in the control group. They stated that contact allergy due to cosmetics could play a role in rosacea pathogenesis. Pónyai et al.13 found contact hypersensitivity in 35.4% of 82 rosacea patients. We found a positive reaction to at least 1 allergen in 32.3% of the patient group and 20% of the control group with the European standard series while these rates were 30.8% and 10% respectively with the cosmetic series. In total, there was a positive reaction to at least one allergen in 38.5% of the patient group and 25.0% of the control group. Our rates were similar to these other studies and our study is valuable due to the large number of subjects and the presence of a control group.
The most common positive allergens in the European standard series in our rosacea patients were nickel sulfate (20.0%), textile dye mixture (4.6%), fragrance mixture 2 (3.1%), cobalt chloride (3.1%) and lyral (3.1%). In the cosmetic series, the most common allergens were amerchol L 101 (4.6%), triethanolamine (3.1%), sorbitan sesquiolate (3.1%), dodecyl gallate (3.1%) and lauryl glycoside (3.1%) in rosacea patients. Jappe et al.11 retrospectively evaluated contact allergy in 361 rosacea patients and found positive reactions against nickel sulfate (9.3%), fragrance mixture (8.8%), thimerosal (6.9%), balsam of Peru (5.9%), potassium dichromate (4.6%), and propolis (2.8%).
Nickel, balsam of Peru, fragrance mixture I, paraphenylenediamine and lanolin were found the most common allergens with a positive reaction in rosacea patients in another study. They reported that contact hypersensitivity was mostly to cosmetics, wash products, facial creams and cosmetic material, lotions and gels. Contact hypersensitivity towards the ingredients of medical creams was positive at a rate of 27.8%. They concluded that the contact hypersensitivity in rosacea patients was mostly towards cosmetics13.
Jappe et al.12 evaluated contact allergy in 78 rosacea patients and found positive reactions against nickel sulfate (15.4%), fragrance mixture I (5.2%), balsam of Peru (10.4%), potassium dichromate (5.1%), and lyral (3.8%). There was no allergic reaction in the patch tests with the patients' own products but an irritant patch test reaction was seen against sodium lauryl sulfate. They also reported that reactions against irritants such as sodium lauryl sulfate are indicators of the skin hypersensitivity in rosacea patients.
In our study there are some common positive allergens such as nickel sulfate and fragrance mixture with other studies, but they are generally different. This difference could be explained by the different occupational and environmental exposure of the patients.
Alcohol, hot beverages, chocolate, dried nuts, spicy food, cheese, some medications, the sun, excessively hot and cold weather, wind, some cleaners, moisturizers, cosmetics, physical and emotional stress, menstruation and pregnancy are among factors that can trigger rosacea attacks1. Antimicrobial peptides (cathelicidin, LL-37), proteases (kallikrein serine proteases, matrix metalloproteinases) and toll-like receptors (TLRs) among the members of the natural immune system are blamed in recent studies. Most of the trigger factors in rosacea are effective through TLRs3.
The barrier function in rosacea patients is known to be compromised due to the effect of antimicrobial peptides and proteases2. Darlenski et al.9 have evaluated transepidermal water loss, stratum corneum hydration, epidermal barrier, skin irritation and contact sensitization in rosacea, atopic dermatitis patients and healthy subjects in their study. They stated that the disturbed skin barrier function facilitates allergen passage and contributes to contact hypersensitivity. Although they found that the irritant threshold value and contact sensitization did not differ in rosacea patients compared to controls, the skin barrier function and stratum corneum hydration had decreased.
It is thought that the cosmetic intolerance in rosacea patients could be related to the disturbed skin barrier function and vascular hyperreactivity117. We also found a higher incidence of irritant reactions in the rosacea group than the control group.
The use of cleaners that do not contain soap, preferring sunscreen with physical barriers, using cosmetics with protective silicone, and avoiding cosmetics containing astringent substances, menthol or sodium lauryl sulfate are currently the general recommendations used by physicians for their patients17. We found that a positive reaction to at least one allergen in patch tests was more common in patients with symptoms such as itching, burning, tingling or pain. We believe that a patch test should be performed in patients with marked symptoms to determine the “personal” trigger factors and prevent the attacks.
It has been reported that social anxiety, shyness, depression and decreased quality of life are more common in rosacea patients than in the general population. The appropriate treatment of the disease and recommendations to prevent attacks could therefore improve the quality of life15. We believe that determining contact sensitivity in rosacea patients is useful in their treatment and follow-up. In conclusion contact sensitivity and irritant reactions were detected more common in rosacea. We think that patch testing is useful in treatment and follow up of rosacea patients especially if symptoms such as itching, burning and stinging are present.
ACKNOWLEDGMENT
This study was supported by the Eskisehir Osmangazi University Scientific Research Projects Commission.
References
1. Tüzün Y, Wolf R, Kutlubay Z, Karakuş O, Engin B. Rosacea and rhinophyma. Clin Dermatol. 2014; 32:35–46. PMID: 24314376.

2. Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology: a review of recent findings. J Am Acad Dermatol. 2013; 69(6 Suppl 1):S15–S26. PMID: 24229632.

3. Dorschner RA, Williams MR, Gallo RL. Rosacea, the face of innate immunity. Br J Dermatol. 2014; 171:1282–1284. PMID: 25523247.

4. Meyer-Hoffert U, Schröder JM. Epidermal proteases in the pathogenesis of rosacea. J Investig Dermatol Symp Proc. 2011; 15:16–23.

5. Wolf R, Orion E, Matz H. Co-existing sensitivity to metronidazole and isothiazolinone. Clin Exp Dermatol. 2003; 28:506–507. PMID: 12950340.

6. Swanson LA, Warshaw EM. Allergic contact dermatitis to topical brimonidine tartrate gel 0.33% for treatment of rosacea. J Am Acad Dermatol. 2014; 71:832–833. PMID: 25219708.

7. Madsen JT, Thormann J, Kerre S, Andersen KE, Goossens A. Allergic contact dermatitis to topical metronidazole-3 cases. Contact Dermatitis. 2007; 56:364–366. PMID: 17577385.
8. Cookson H, McFadden J, White J, White IR. Allergic contact dermatitis caused by Mirvaso®, brimonidine tartrate gel 0.33%, a new topical treatment for rosaceal erythema. Contact Dermatitis. 2015; 73:366–367. PMID: 26768997.

9. Darlenski R, Kazandjieva J, Tsankov N, Fluhr JW. Acute irritant threshold correlates with barrier function, skin hydration and contact hypersensitivity in atopic dermatitis and rosacea. Exp Dermatol. 2013; 22:752–753. PMID: 24112695.

10. Corazza M, la Malfa W, Lombardi A, Maranini C, Virgili A. Role of allergic contact dermatitis in rosacea. Contact Dermatitis. 1997; 37:40–41. PMID: 9255491.
11. Jappe U, Schnuch A, Uter W. Rosacea and contact allergy to cosmetics and topical medicaments--retrospective analysis of multicentre surveillance data 1995-2002. Contact Dermatitis. 2005; 52:96–101. PMID: 15725288.
12. Jappe U, Schäfer T, Schnuch A, Uter W. Contact allergy in patients with rosacea: a clinic-based, prospective epidemiological study. J Eur Acad Dermatol Venereol. 2008; 22:1208–1214. PMID: 18452530.

13. Pónyai G, Kiss D, Németh I, Temesvári E. Contact hypersensitivity in rosacea--a study in 82 patients. J Eur Acad Dermatol Venereol. 2012; 26:1171–1172. PMID: 21929553.
14. Çakmak SK, Gönül MT, Kılıç A, Gül Ü. The role of contact allergy in rosacea. J Turk Acad Dermatol. 2007; 1:71201a.
15. Moustafa F, Lewallen RS, Feldman SR. The psychological impact of rosacea and the influence of current management options. J Am Acad Dermatol. 2014; 71:973–980. PMID: 24993600.

16. Forton FM. Papulopustular rosacea, skin immunity and Demodex: pityriasis folliculorum as a missing link. J Eur Acad Dermatol Venereol. 2012; 26:19–28.

17. Pelle MT, Crawford GH, James WD. Rosacea: II. Therapy. J Am Acad Dermatol. 2004; 51:499–512. PMID: 15389184.

Table 1
Clinical findings of rosacea patients (n=65)
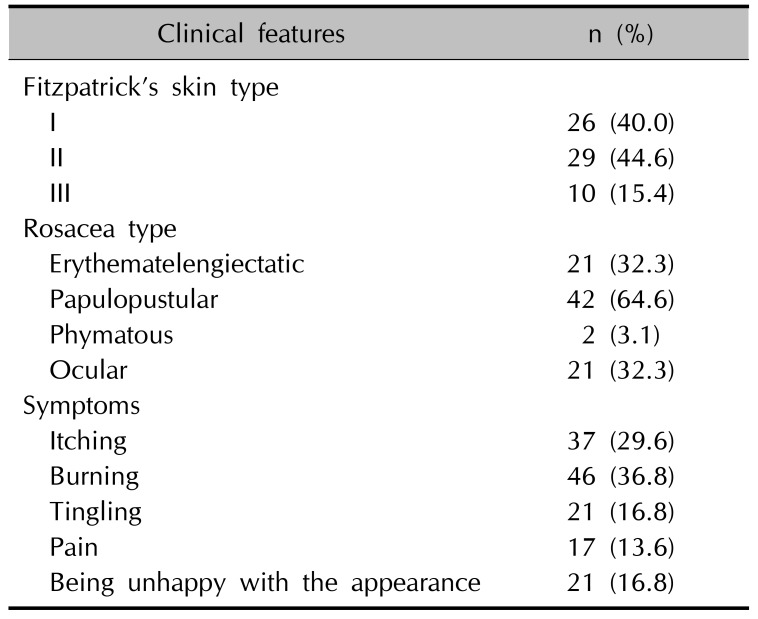
Table 2
Number of allergen positivities to European standard, cosmetic series and in total
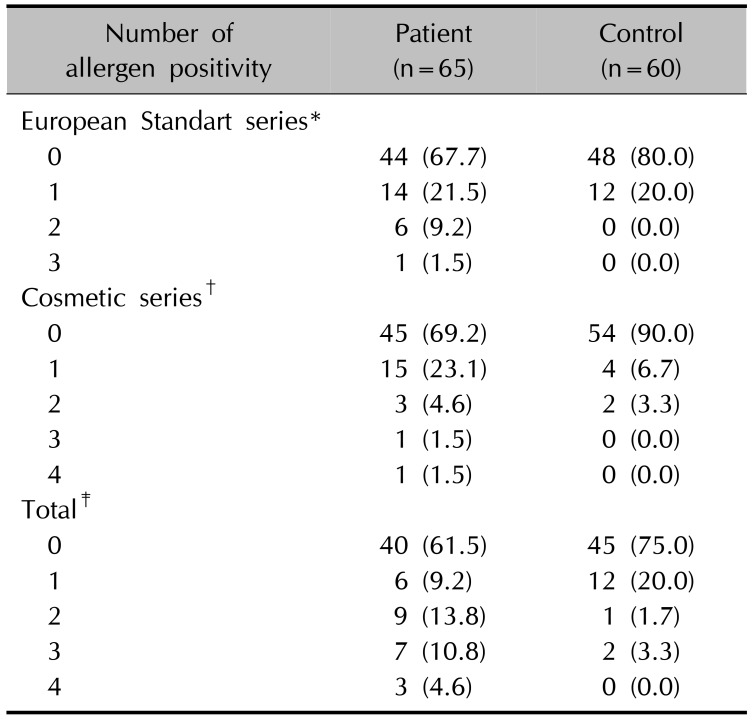
Table 3
Positive allergens in European standard series
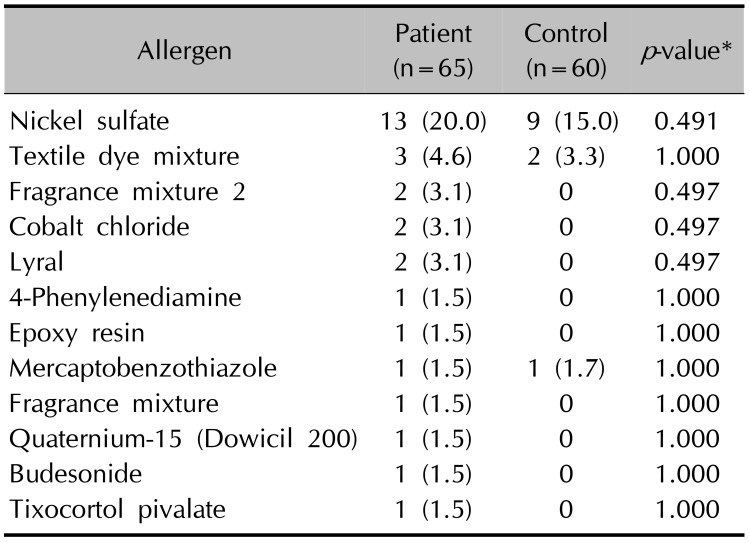
Table 4
Positive allergens in cosmetic series




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download