Dear Editor:
In clinical dermatology, abscesses are generally caused by secondary impetiginization of a previous furuncle or a ruptured epidermal cyst. We encountered a rare case of cutaneous abscess in the maxillo-mandibular region, complicated by bisphosphonate-related osteonecrosis of the jaw.
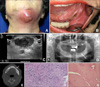
A 76-year-old woman presented with an erythematous swollen mass in the submental area (Fig. 1A), which had appeared 5 days prior. The patient complained of dull pain and lesional heat. She had been taking 70 mg alendronic acid (Fosamax®; Merck, Kenilworth, NJ, USA), once weekly, for osteoporosis for approximately 10 years. Suspecting a cutaneous abscess, we performed a radiologic evaluation using an ultrasonic approach and incision biopsy with drainage. A relatively well-defined heterogeneous hypoechoic mass was evidenced by the ultrasound (Fig. 1C), and the histopathological findings showed a deep dermal abscess and necrotic debris infiltrated by inflammatory cells mainly composed of neutrophils (Fig. 1F). Microbiologic evaluation done by skin tissue showed gram positive cocci (Streptococcus constellatus) in bacterial culture, and negative results in fungal and mycobacterial culture. As the anatomical location of the lesion suggested a dental origin, the patient consulted the oral and maxillofacial surgery department. The oral examination showed exposed necrotic bone in the left molar area of the mandible (Fig. 1B). On radiologic evaluation, a radiolucent area on the conventional radiograph and a low-density lesion corresponding to the clinically-evidenced exposed necrotic bone on dental computed tomography (CT) were observed (Fig. 1D, E).
The patient was diagnosed with a cutaneous abscess arising as a complication of bisphosphonate-related osteonecrosis of the jaw. We initiated treatment with surgical sequestrectomy combined with systemic antibiotics comprising first-generation cephalosporin and metronidazole and adjuvant chlorhexidine oral antiseptics. Necrotic osteocytes with inflammatory infiltration were observed on the sequestrectomy's pathologic specimen (Fig. 1G).
Bisphophonates are the most commonly prescribed medication for osteoporosis. Malignant bony metastasis and Paget's disease are also candidates for bisphophonate indication. Bisphophonates reduce bony resorption by influencing overall osteoclast activity, inhibiting the maturation of osteoclast precursors, promoting the conversion of active osteoclasts into inactive ones, and inducing apoptosis of the inactive osteoclasts1. As the medication use increases, osteonecrosis of the jaw has been reported as a side-effect. The pathomechanisms are explained by the bisphosphonates' anti-angiogenic effect, which causes avascular state of the bone, and its anti-osteoclastic effect, which disturbs the homeostasis of bone cell turnover2. Diagnosis is made when necrotic bone exposures persistent for >8 weeks are observed in the maxillofacial region without a history of jaw irritation, such as head or neck radiation therapy, or in the presence of current or previous treatment with bisphosphonates3. Radiologic evaluations including conventional radiographs, CT, bone scans, and magnetic resonance imaging can provide relatively specific findings4.
Although bisphosphonate-related osteonecrosis of the jaw is unfamiliar to dermatologists, given the prevalence of osteoporosis and the relevance of bisphosphonates, the present case demonstrates possible cutaneous manifestations of the disease. Dermatologists encountering an exposed cutaneous abscess in the maxillo-mandibular region should consider oral examination for the identification of potentially progressive processes behind the abscess5.
Figures and Tables
Fig. 1
Bisphosphonate-related osteonecrosis of the jaw. (A) Physical examination exihibited an erythematous bulging mass from left submental area to upper neck. (B) Exposed necrotic bone was observed in left molar area of the mandible on oral examination. (C) Relatively well-defined heterogenous hypoechoic mass was assessed by ultrasound. (D, E) Radiolucent area (white arrow) in conventional radiograph, and low density lesion (white arrow) in dental computed tomography were observed. (F) Deep dermal abscess and necrotic debris infiltrated by inflammatory cells mainly composed of neutrophils were observed in tissue of cutaneous abscess (H&E, ×200). (G) Necrotic osteocytes with inflammatory infiltration were observed in bony specimen of sequestrectomy (H&E, ×200).
References
1. Rogers MJ, Gordon S, Benford HL, Coxon FP, Luckman SP, Monkkonen J, et al. Cellular and molecular mechanisms of action of bisphosphonates. Cancer. 2000; 88:12 Suppl. 2961–2978.

2. Marx RE, Sawatari Y, Fortin M, Broumand V. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg. 2005; 63:1567–1575.

3. Sigua-Rodriguez EA, da Costa Ribeiro R, de Brito AC, Alvarez-Pinzon N, de Albergaria-Barbosa JR. Bisphosphonaterelated osteonecrosis of the jaw: a review of the literature. Int J Dent. 2014; 2014:192320.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download