Dear Editor:
Angiomatoid fibrous histiocytoma (AFH) is a rare soft tissue tumor that demonstrates intermediate malignant potential. It typically arises in superficial soft tissues of the extremities, head, neck and trunk in children or young adults1.
A 4-year-old girl presented with an ill-circumscribed asymptomatic mass on her right shoulder which developed 8 months ago. On physical examination, the lesion was 4.5 cm in its greatest dimension with no sign of erythema or induration (Fig. 1A). She underwent punch biopsy of the lesion, which revealed an inflamed pseudocyst with organizing hematoma (Fig. 1B). Magnetic resonance finding showed soft tissue tumor with multiple chambers with fluid level suggesting hemorrhage (Fig. 1C) and ultrasonography showed hypervascular lesion (Fig. 1D), which indicated a hemangioma. Under the diagnosis of hemangioma, she was referred to a pediatric surgeon for complete excision. On pathologic examination, an un-encapsulated irregular mass was found with focal areas of hemorrhage, pseudocyst, and diffuse hemosiderin deposit. Tumor consists of various cells such as round cells or spindle cells with sheet-like or fascicular architecture. In the periphery of the tumor, multiple aggregates of inflammatory cells are composed mainly of lymphocytes (Fig. 1E, F). According to immunohistochemical studies, tumor cells revealed positive results for CD68 (Fig. 1G), epithelial membrane antigen (EMA) (Fig. 1H), CD99 (Fig. 1I), and desmin focally, whereas negative results for CD31, HHV-8, CK AE1/3, CD35, CD21. Based on the histopathologic study, the final diagnosis of AFH was made. Metastatic work up was carried out, which was all negative. She remains healthy without local recurrence or metastasis during 3-month follow-up.
First described by Enzinger2 in 1979, AFH is a tumor of low-grade malignancy with distinctive histopathologic features. AFH usually presents with a peak incidence during the first 2 decades of life1. Clinically, the patient usually presents with asymptomatic nodule or mass. There are a few cases reported by dermatologists in English (Table 1)3. Tumors of these cases are smaller than in our case.
Diagnosis of AFH is based on the pathologic examination; tumors are well-circumscribed and surrounded by a fibrous pseudocapsule. AFH shows a wide morphologic spectrum, but it consistently demonstrates the multilobular growth of round cells, spindle cells or histiocyte-like cells with low mitotic activity1. It is also characteristically surrounded at the periphery by inflammatory infiltrates consisting mainly of lymphocytes and plasma cells.
AFH lacks specific immunohistochemical markers, which give supportive rather than diagnostic information. Tumor cells of AFH are reported variably positive for CD68, EMA, desmin, and CD99. Majority are negative for S-100, CD21, CD35, cytokeratins, and vascular endothelial markers such as CD31 and CD344.
Most cases of AFH have an excellent prognosis, but the correct diagnosis is essential due to the risk of local recurrence and a small risk of metastasis4. Either with X-ray or magnetic resonance imaging, AFH demonstrates inconsistent and nonspecific findings5.
Dermatologists should aware of this disease entity so that can diagnosis it early and properly. This unusual disease entity raises the concern that complete excision of the tumor is essential to diagnose precisely especially when suspicious of a vascular tumor.
References
1. Justin Wong SB, Wee A, Puhaindran ME, Pang B, Lee VK. Angiomatoid fibrous histiocytoma with prominent myxoid stroma: a case report and review of the literature. Am J Dermatopathol. 2015; 37:623–631. PMID: 25406850.
2. Enzinger FM. Angiomatoid malignant fibrous histiocytoma: a distinct fibrohistiocytic tumor of children and young adults simulating a vascular neoplasm. Cancer. 1979; 44:2147–2157. PMID: 228836.
3. Wilk M, Zelger BG, Debiec-Rychter M, Sciot R, Zelger B. Angiomatoid fibrous histiocytoma-case series with emphasis on a late fibrotic variant. J Dtsch Dermatol Ges. 2015; 13:441–448. PMID: 25918088.
4. Thway K, Fisher C. Angiomatoid fibrous histiocytoma: the current status of pathology and genetics. Arch Pathol Lab Med. 2015; 139:674–682. PMID: 25927151.

5. Huerter ME, Hammadeh R, Zhou Q, Riker AI. Recurrent angiomatoid fibrous histiocytoma: a case report and review of the literature. Ochsner J. 2014; 14:441–444. PMID: 25249813.
Fig. 1
(A) A skin colored mass on the right shoulder. (B) Punch biopsy of the lesion showed inflamed pseudocyst with organizing hematoma (H&E, ×40). (C) On magnetic resonance imaging, the tumor shows multiple chambers with fluid level, which is finding of hemangioma or other soft tissue tumors with internal hemorrhage. (D) Ultrasonography reveals increased vascularity of the tumor. (E) The tumor consists of various cells such as round cells or spindle cells with sheet-like or fascicular architecture (H&E, ×100). (F) Multiple aggregates of inflammatory cells are composed mainly of lymphocytes in the periphery of the tumor (H&E, ×40). (G~I) The tumor cells show positive staining for (G) CD68, (H) epithelial membrane antigen, and (I) CD99 (G~I: ×100).
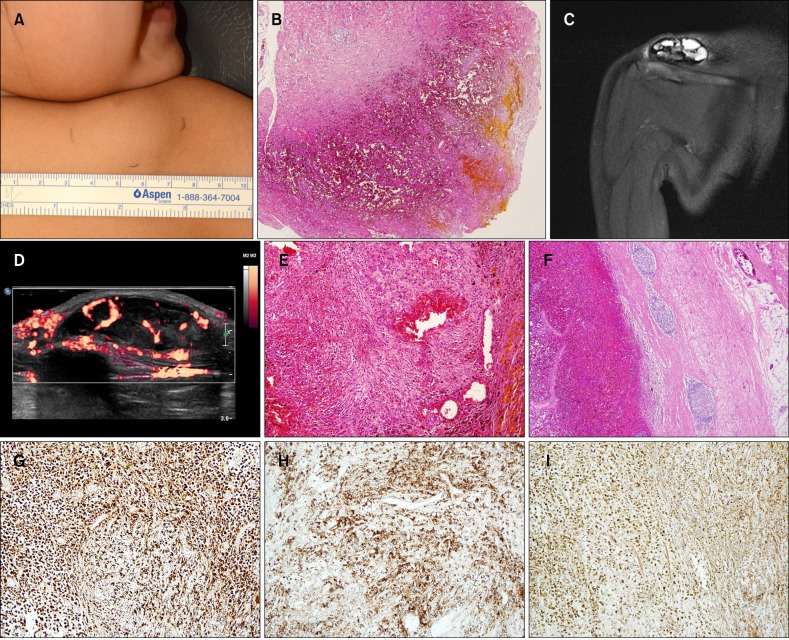
Table 1
Clinical features of patients of angiomatoid fibrous histiocytoma reported in dermatologic journal
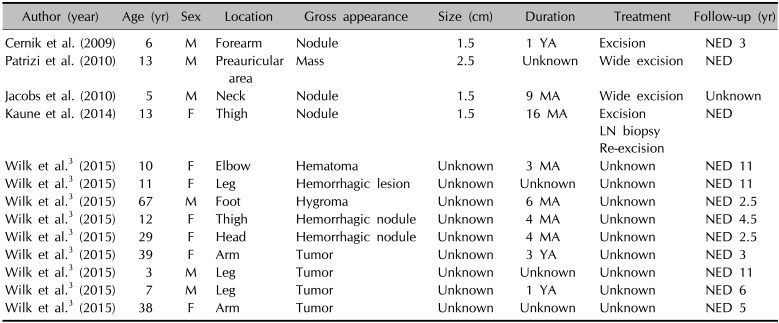
| Author (year) | Age (yr) | Sex | Location | Gross appearance | Size (cm) | Duration | Treatment | Follow-up (yr) |
|---|---|---|---|---|---|---|---|---|
| Cernik et al. (2009) | 6 | M | Forearm | Nodule | 1.5 | 1 YA | Excision | NED 3 |
| Patrizi et al. (2010) | 13 | M | Preauricular area | Mass | 2.5 | Unknown | Wide excision | NED |
| Jacobs et al. (2010) | 5 | M | Neck | Nodule | 1.5 | 9 MA | Wide excision | Unknown |
| Kaune et al. (2014) | 13 | F | Thigh | Nodule | 1.5 | 16 MA | Excision | NED |
| LN biopsy | ||||||||
| Re-excision | ||||||||
| Wilk et al.3 (2015) | 10 | F | Elbow | Hematoma | Unknown | 3 MA | Unknown | NED 11 |
| Wilk et al.3 (2015) | 11 | F | Leg | Hemorrhagic lesion | Unknown | Unknown | Unknown | NED 11 |
| Wilk et al.3 (2015) | 67 | M | Foot | Hygroma | Unknown | 6 MA | Unknown | NED 2.5 |
| Wilk et al.3 (2015) | 12 | F | Thigh | Hemorrhagic nodule | Unknown | 4 MA | Unknown | NED 4.5 |
| Wilk et al.3 (2015) | 29 | F | Head | Hemorrhagic nodule | Unknown | 4 MA | Unknown | NED 2.5 |
| Wilk et al.3 (2015) | 39 | F | Arm | Tumor | Unknown | 3 YA | Unknown | NED 3 |
| Wilk et al.3 (2015) | 3 | M | Leg | Tumor | Unknown | Unknown | Unknown | NED 11 |
| Wilk et al.3 (2015) | 7 | M | Leg | Tumor | Unknown | 1 YA | Unknown | NED 6 |
| Wilk et al.3 (2015) | 38 | F | Arm | Tumor | Unknown | Unknown | Unknown | NED 5 |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download