Abstract
Dermatofibrosarcoma protuberans (DFSP) is a slow growing low-grade cutaneous sarcoma. Local recurrence after excision is common due to the poorly defined periphery that renders histological control of surgical margin difficult, Mohs micrographic surgery is the optimal method for treatment. A 41 years old male patient, who had a previous history of DFSP, came to our dermatology clinic for evaluation of an asymptomatic firm flesh-colored nodule on the forehead. Total excision biopsy was done and the mass was histologically proved as DFSP. Wide excision with reconstruction was performed and showed no sign of recurrence till 18-month follow up. Local recurrence is known to be common for DFSP but a new visible lesion distant from the initial site may be confused as a de novo lesion or a benign neoplasm especially in scalp area, and thus interrupt early detection of DFSP. Herein, we report a case of recurrent DFSP of scalp which recurred distant from the original lesion.
Dermatofibrosarcoma protuberans (DFSP) is an uncommon cutaneous sarcoma with dermal fibroblastic origin that infiltrates through the dermis and subcutaneous fat. The tumor presents as a pink or purple indurated plaque. It can easily be misdiagnosed as a benign neoplasm1. It rarely metastasizes to distant organ, although local recurrence after excision is common due to aggressive local growth and uncertain margin of tumors. Here we report a case of recurred DFSP in a distant location 10 years after primary excision along with literature review.
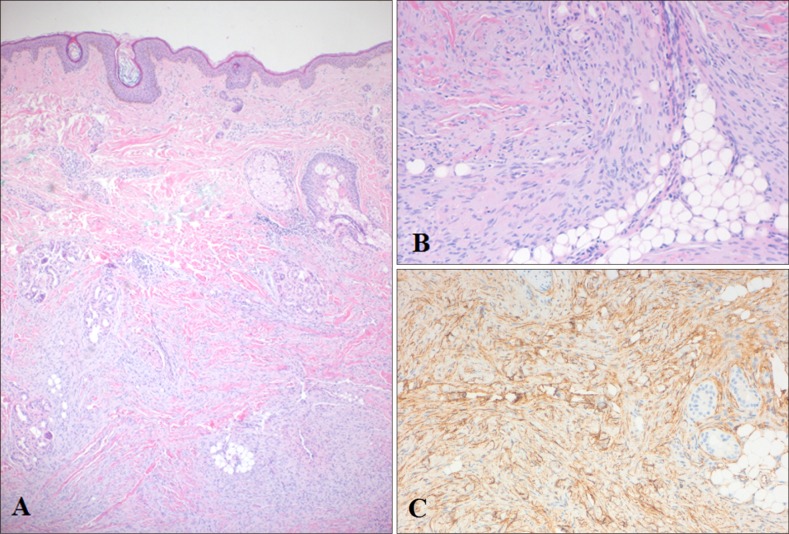
A 41-year-old male patient came to our dermatology clinic for evaluation of an asymptomatic firm flesh-colored nodule on the forehead which appeared 4 months prior to the visit (Fig. 1). The patient had a previous history of DFSP on the fronto-vertex scalp that was thought to be completely removed through wide excision with local triple advancement flap 10 years ago. There was no specific lesion on forehead at that time. Excision biopsy was done on the new lesion under the impression of DFSP and sebaceous cyst. Histopathological examination of the obtained specimen showed densely packed uniform spindle cells in storiform pattern with elongated nuclei (Fig. 2A, B). Immunohistochemistry findings revealed positive results for CD34 (Fig. 2C) but negative for CD68, smooth-muscle actin (SMA), or S-100 protein.
Pathologic report confirmed that the tumor was consistent with DFSP. Subsequently, Mohs micrographic surgery (MMS) was performed. Due to continuous infiltrated margin even after 4 stages of Mohs excision with 5 mm margin, the patient was transferred to department of plastic surgery. Wide excision with reconstruction by thoracodorsal artery perforator flap was performed. There was no evidence of tumor's local recurrence or metastasis during 18-month of follow up.
DFSP is a rare fibrohistiocytic tumor. It accounts for less than 0.1% of all malignancies and approximately 1% of soft-tissue sarcoma12. DFSP typically arises in youthful individuals aged 20~40 years3. The origin of cells in DFSP is believed to be a dermal stem cell or an undifferentiated mesenchymal cell with fibroblastic, muscular, and neurologic features4.
DFSP usually presents as a purple to pinkish firm dermal nodule or plaque. The most common affected sites are trunk and extremities, followed by head and neck region5. Histologically, DFSP consists of densely arranged storiform and cartwheel fascicles of spindle cells with elongated nuclei. Cells of DFSP show little atypia or mitotic activity. The epidermis above DFSP is separated from the tumor by a Grenz zone. DFSP usually infiltrates subcutaneous fat or skeletal muscles with a characteristic honeycomb pattern6. DFSP characteristically shows high expression of CD34 and vimentin antigens. It occasionally shows focal expression of SMA. However, it has negative expression for S-100 protein, factor XIIIa, or D2-4016.
DFSP can easily recur after simple excision because of its indefinite margin. Therefore, MMS needs to be performed to remove DFSP clearly. Gloster et al.7 has insisted that MMS is the treatment of choice for DFSP. In their report, all cases were treated with either surgical wide excision or MMS. Recurrence rate of MMS was 1.6% while recurrence rate of wide excision was 20%. This result can also be applied in cases when DFSP is localized to scalp. Loss and Zeitouni8 have reported that the recurrence rate of scalp DFSP treated by surgical excision is 35%. In addition, 7 cases treated by MMS did not develop any local recurrence.
In the current case, it was difficult to suspect DFSP from the first impression due to difference between the chief complaint (a skin-colored tiny nodule on forehead) and the typical clinical manifestation of DFSP. In addition, DFSP rarely shows distal metastasis. However, there was a lesion on the patient's forehead which was not located close to the previously treated DFSP lesion on the fronto-vertex scalp. Nevertheless, we considered the possibility of DFSP. MMS was performed to treat DFSP with minimized recurrence and additional wide excision with a full thickness skin graft was done. The final pathologic report showed that there was local recurrence on the previously treated DFSP lesions. Recurred tumor had spread subclinically to the forehead. Therefore, when a suspicious lesion is observed on the skin of a patient who has a history of DFSP, the possibility of DFSP should not be overlooked, especially in the scalp, including the forehead. The lesion should be examined through skin biopsy for timely treatment.
References
1. Kim MJ, Hur MS, Choi BG, Kim SY, Lee YW, Choe YB, et al. Pedunculated nodules as a variant of dermatofibrosarcoma protuberans. Ann Dermatol. 2016; 28:629–631. PMID: 27746644.

2. Ratner D, Thomas CO, Johnson TM, Sondak VK, Hamilton TA, Nelson BR, et al. Mohs micrographic surgery for the treatment of dermatofibrosarcoma protuberans. Results of a multiinstitutional series with an analysis of the extent of microscopic spread. J Am Acad Dermatol. 1997; 37:600–613. PMID: 9344201.
3. Snow SN, Gordon EM, Larson PO, Bagheri MM, Bentz ML, Sable DB. Dermatofibrosarcoma protuberans: a report on 29 patients treated by Mohs micrographic surgery with long-term follow-up and review of the literature. Cancer. 2004; 101:28–38. PMID: 15221986.

4. Elgart GW, Hanly A, Busso M, Spencer JM. Bednar tumor (pigmented dermatofibrosarcoma protuberans) occurring in a site of prior immunization: immunochemical findings and therapy. J Am Acad Dermatol. 1999; 40:315–317. PMID: 10025857.

5. Harati K, Lange K, Goertz O, Lahmer A, Kapalschinski N, Stricker I, et al. A single-institutional review of 68 patients with dermatofibrosarcoma protuberans: wide re-excision after inadequate previous surgery results in a high rate of local control. World J Surg Oncol. 2017; 15:5. PMID: 28056985.

6. Thway K, Noujaim J, Jones RL, Fisher C. Dermatofibrosarcoma protuberans: pathology, genetics, and potential therapeutic strategies. Ann Diagn Pathol. 2016; 25:64–71. PMID: 27806849.

7. Gloster HM Jr, Harris KR, Roenigk RK. A comparison between Mohs micrographic surgery and wide surgical excision for the treatment of dermatofibrosarcoma protuberans. J Am Acad Dermatol. 1996; 35:82–87. PMID: 8682970.
8. Loss L, Zeitouni NC. Management of scalp dermatofibrosarcoma protuberans. Dermatol Surg. 2005; 31:1428–1433. PMID: 16416612.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download