Abstract
Pagetoid Bowen disease is a histological variant of Bowen disease which demonstrates large pale staining cells (pagetoid cells). It requires differential diagnosis from other cutaneous malignancies with similar patterns, such as extramammary Paget's disease (EMPD) and Pagetoid melanoma in situ. Herein, we report a case of Pagetoid Bowen disease which was initially misdiagnosed as ectopic EMPD.
Bowen disease is squamous cell carcinoma in situ with full thickness epidermal atypia having potential to become invasive squamous cell carcinoma. Pagetoid Bowen disease is a rare histologic variant of Bowen disease which demonstrates atypical pagetoid cells with abundant pale cytoplasm. It resembles those of extramammary Paget's disease (EMPD) or pagetoid melanoma in situ. Their differential diagnosis is important because they have different prognosis and associated diseases. Immunohistochemical findings are useful to distinguish theses disease, but the distinction is still difficult in some cases. Herein, we report a case of Pagetoid Bowen disease which was initially misdiagnosed as ectopic EMPD.
A 76-year-old Korean man visited our clinic with a 2-cm variably dark-brown and erythematous scaly plaque lesion on the left lower leg; the lesion had been present for 2 years (Fig. 1A). He denied any trauma or previous treatments on the site. There was no pruritus or burning sensation. He reported that the lesion had slowly grown for 2 years. On physical examination, no other skin lesions were found in the axilla, groin, genitalia, perianal area, and umbilicus. No lymph nodes were palpable in cervical, axillary, and inguinal areas. Past medical history included diabetes mellitus on medication. Punch biopsy specimen showed tumor cells in the epidermis with acanthosis (Fig. 1B). The tumor cells had abundant pale cytoplasm and large pleomorphic nuclei. Immunohistochemical staining was focally positive for cytokeratin 7 (CK7) and the initial diagnosis was EMPD. The lesion was totally excised and underwent immunohistochemical staining to confirm the diagnosis. Unexpectedly, the excised specimen was negative for CK7, CK20, carcinoembryonic antigen (CEA), and S-100. On the other hand, it shows positivity for p63, CK5/6, and epithelial membrane antigen (EMA) (Fig. 2). Based on these clinical, histopathological, and immunohistochemical findings, we finally diagnosed the case as Pagetoid Bowen disease. There was no recurrence at 16 months after complete excision.
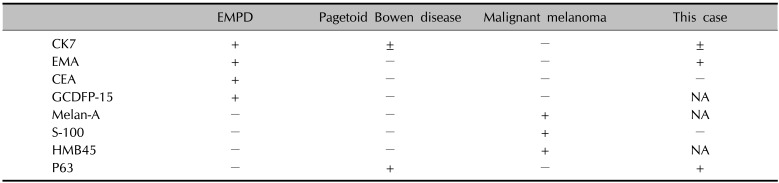
The diagnosis of Pagetoid Bowen disease in this case is based on several features. First, EMPD is usually developed on apocrine gland-rich area, especially on anogenital region, although there are reports of rare cases that developed on non-apocrine gland bearing area1. The patients of this case report had skin lesion on his lower leg, therefore the diagnosis of EMPD is less likely. Second, immunohistochemical traits act as an important diagnostic key. In most of the cases, neoplastic cells in Pagetoid Bowen disease presents immunohistochemical features of squamous cells and are generally negative for CK7, CAM 5.2, CEA and gross cystic disease fluid protein 15 (GCDFP-15). To the contrary, these markers are positive in EMPD234. Also, Memezawa et al.5 reported the usefulness of p63 for differentiation of Pagetoid Bowen disease from EMPD. It is expressed in epidermis, but not in apocrine or eccrine glandular cells. In this case, negativity for CK7, CK20, CEA, S-100 and positivity for CK5/6 and p63 supported the diagnosis of Pagetoid Bowen disease, not EMPD or melanoma in situ. Immunohistochemical findings of Pagetoid Bowen disease, EMPD, and melanoma in situ is summarized in Table 1. However, the distinction is sometimes very difficult. Rosen et al.6 reported a case; histopathologic findings were consistent with Bowen disease by hematoxylin and eosin (H&E) staining, but final diagnosis was Paget's disease by immunohistochemical staining. Similarly, Paget's disease was initially misdiagnosed as melanoma by H&E staining and immunohistochemical staining changed the original diagnosis7.
Additionally, immunohistochemical staining cannot always distinguish the diseases. There are some case reports of Pagetoid Bowen disease that expressed CK7, CEA, or EMA891011. Also, the association of Bowen disease and EMPD is suggested. There are EMPD with Bowenoid features and EMPD combined with Bowen disease1213. Some authors hypothesized bidirectional stell cell differentiation14 and we think that this hypothesis can explain these phenomena. According to the hypothesis, some cases of Pagetoid Bowen disease and EMPD shares the same precursor multipotent stem cells, and if they differentiate bidirectionally to both squamous and secretory cells, they can express the characteristics of both cells1415. The present case report also supports this hypothesis.
To our knowledge, there are only a few case reports161718 of Pagetoid Bowen disease in Korea. In addition, there is scarce report of Pagetoid Bowen disease that expresses immunohistochemical markers of secretory cells like EMA. Its histopathologic differentiation is often difficult and immunohistochemical staining is important to confirm the diagnosis. Further study is needed on the the hypothesis of shared precursor stem cells of Pagetoid Bowen disease and EMPD, and their bidirectional differentiation to neoplastic cells.
References
1. Sawada Y, Bito T, Kabashima R, Yoshiki R, Hino R, Nakamura M, et al. Ectopic extramammary Paget's disease: case report and literature review. Acta Derm Venereol. 2010; 90:502–505. PMID: 20814627.

2. Guldhammer B, Nørgaard T. The differential diagnosis of intraepidermal malignant lesions using immunohistochemistry. Am J Dermatopathol. 1986; 8:295–301. PMID: 2429574.

3. Shah KD, Tabibzadeh SS, Gerber MA. Immunohistochemical distinction of Paget's disease from Bowen's disease and superficial spreading melanoma with the use of monoclonal cytokeratin antibodies. Am J Clin Pathol. 1987; 88:689–695. PMID: 2446491.

4. Lau J, Kohler S. Keratin profile of intraepidermal cells in Paget's disease, extramammary Paget's disease, and pagetoid squamous cell carcinoma in situ. J Cutan Pathol. 2003; 30:449–454. PMID: 12859743.
5. Memezawa A, Okuyama R, Tagami H, Aiba S. p63 constitutes a useful histochemical marker for differentiation of pagetoid Bowen's disease from extramammary Paget's disease. Acta Derm Venereol. 2008; 88:619–620. PMID: 19002351.
6. Rosen L, Amazon K, Frank B. Bowen's disease, Paget's disease, and malignant melanoma in situ. South Med J. 1986; 79:410–413. PMID: 2422766.

7. Reed W, Oppedal BR, Eeg Larsen T. Immunohistology is valuable in distinguishing between Paget's disease, Bowen's disease and superficial spreading malignant melanoma. Histopathology. 1990; 16:583–588. PMID: 1695889.

8. Williamson JD, Colome MI, Sahin A, Ayala AG, Medeiros LJ. Pagetoid Bowen disease: a report of 2 cases that express cytokeratin 7. Arch Pathol Lab Med. 2000; 124:427–430. PMID: 10705400.
9. Mai KT, Alhalouly T, Landry D, Stinson WA, Perkins DG, Yazdi HM. Pagetoid variant of actinic keratosis with or without squamous cell carcinoma of sun-exposed skin: a lesion simulating extramammary Paget's disease. Histopathology. 2002; 41:331–336. PMID: 12383215.

10. Armes JE, Lourie R, Bowlay G, Tabrizi S. Pagetoid squamous cell carcinoma in situ of the vulva: comparison with extramammary paget disease and nonpagetoid squamous cell neoplasia. Int J Gynecol Pathol. 2008; 27:118–124. PMID: 18156986.
11. Raju RR, Goldblum JR, Hart WR. Pagetoid squamous cell carcinoma in situ (pagetoid Bowen's disease) of the external genitalia. Int J Gynecol Pathol. 2003; 22:127–135. PMID: 12649666.

12. Jang EJ, Bae YK, Shin DH, Lee DJ. Extramammary Paget's disease combined with squamous cell carcinoma in situ of the vulva: a case report and differential diagnosis. Ann Dermatol. 2016; 28:497–498. PMID: 27489435.

13. Chung J, Kim JY, Gye J, Namkoong S, Hong SP, Park BC, et al. Extramammary Paget's disease of external genitalia with bowenoid features. Ann Dermatol. 2013; 25:88–91. PMID: 23467383.

14. Peralta OC, Barr RJ, Romansky SG. Mixed carcinoma in situ: an immunohistochemical study. J Cutan Pathol. 1983; 10:350–358. PMID: 6313778.

15. Baldovini C, Betts CM, Reggiani C, Reggiani M, Foschini MP. Ultrastructural examination of a case of pagetoid Bowen disease exhibiting immunohistochemical features in common with extramammary paget disease. Am J Dermatopathol. 2015; 37:e83–e86. PMID: 24786579.

17. Kim SA, Kwon JI, Jung HR, Lee KS, Cho JW. Primary extramammary Paget's disease combined with Bowen's disease in vulva. Ann Dermatol. 2011; 23(Suppl 2):S222–S225. PMID: 22148056.

18. Sohn IB, Kim SC, Ahn SK. A case of pigmented Pagetoid Bowen's disease. Korean J Dermatol. 2000; 38:1691–1692.
Fig. 1
(A) Dark brown to erythematous scaly plaque on left lower leg. (B) Paget cells with abundant pale cytoplasm and large pleomorphic nuclei are widely distributed in the epidermis (H&E, ×400).
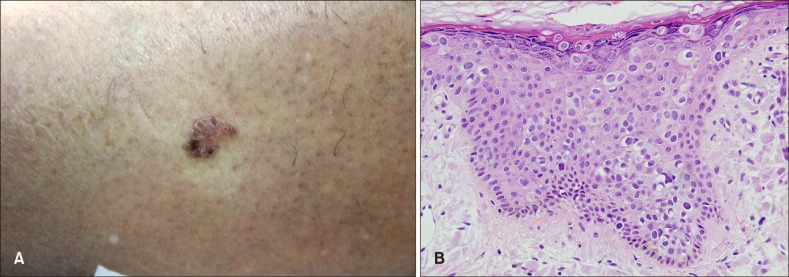
Fig. 2
(A~G) Immunohistochemistry. Neoplastic cells are negative for cytokeratin 7 (CK7) (A), CK20 (C), carcinoembryonic antigen (D), and diffusely positive for epithelial membrane antigen (B). The neoplastic cells show diffuse positivity for p63 (E), CK5/6 (F). Negative S-100 immunohistochemical staining (A~G: ×100).





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download