Abstract
Objective
The aim of this study is to quantitatively evaluate the stability of the skeletal and dental widths using cone-beam computed tomography (CBCT) after segmental Le Fort I osteotomy in adult patients with skeletal Class III malocclusion requiring maxillary expansion.
Methods
In total, 25 and 36 patients with skeletal Class III malocclusion underwent Le Fort I osteotomy (control group) and segmental Le Fort I osteotomy (experimental group), respectively. Coronal CBCT images were used to measure the dental and skeletal widths before (T1) and after (T2) surgery and at the end of treatment (T3). The correlation between the extent of surgery and the amount of relapse in the experimental group was also determined.
Results
In the control group, the dental width exhibited a significant decrease of 0.70 ± 1.28 mm between T3 and T2. In the experimental group, dental and skeletal expansion of 1.83 ± 1.66 and 2.55 ± 1.94 mm, respectively, was observed between T2 and T1. The mean changes in the dental and skeletal widths between T3 and T2 were −1.41 ± 1.98 and −0.67 ± 0.72 mm, respectively. There was a weak correlation between the amount of skeletal expansion during segmental Le Fort I osteotomy and the amount of postoperative skeletal relapse in the experimental group.
With the recent introduction of skeletal fixtures and advancements in various orthodontic techniques, the range of camouflage treatment techniques for patients with skeletal malocclusion has expanded. However, tooth movement for camouflage treatment may result in root resorption, damage the periodontal tissues, or cause dentoalveolar relapse in the future; therefore, fundamental changes in the alveolar and basal bone positions in patients with severe skeletal malocclusion definitively require orthognathic surgery.1234
During orthodontic treatment for orthognathic surgery, the transverse width of the maxillary bone may be insufficient, even if appropriate initial tooth alignment is achieved. In particular, many patients with an open bite or Class III malocclusion exhibit relatively decreased transverse widths due to maxillary hypoplasia, which is closely associated with the development of the dentition.45
In children with a primary dentition or an early mixed dentition, sufficient skeletal expansion can be achieved using traditional rapid palatal expansion (RPE) with Haas or Hyrax appliances.6 However, in some patients who have crossed their pubertal growth spurt years, skeletal effects may not be evident with conventional RPE alone because of partial or complete fusion of the midpalatal suture. The forced use of an expander in patients with a certain degree of fusion of the midpalatal suture may result in adverse effects such as buccal tipping of the molars78 and lingual alveolar bone resorption.9 Miniscrew-assisted RPE (MARPE) was introduced as a method for preventing such adverse effects and inducing cracks in the fused midpalatal suture. With this technique, it is reportedly possible to achieve successful skeletal expansion.1011
In adults who require a large amount of expansion or adults with complete maturation of the midpalatal suture, expansion is performed with the help of a surgical procedure. Surgically assisted RPE (SARPE) splits the maxillary bone to allow a greater amount of expansion; however, it necessitates an additional surgical procedure prior to the orthognathic surgery.12
For patients requiring Le Fort I osteotomy, segmental Le Fort I osteotomy (bipartition, midpalatal split) that achieves surgical expansion through additional splits near the midpalatal suture (which are created by passage between the roots of the maxillary incisors) can be considered.121314 Segmental Le Fort I osteotomy is generally indicated when the required amount of expansion does not exceed 6 to 7 mm. This procedure does not require additional surgery or complex equipment; therefore, it is convenient for the patient. Moreover, unnecessary force is not applied on the teeth, which allows for adequate control of buccolingual tipping. 1315
Although segmental Le Fort I osteotomy was introduced long ago,16 there are few studies on the stability of the skeletal width after this procedure. This may be attributed to some factors that complicate the implementation of such studies. First, several factors such as mechanical resistance from the circummaxillary sutures and tension from the tough palatal mucosa influence relapse after segmental Le Fort I osteotomy.17 Second, the number of patients is generally limited. Accordingly, the objective of the present study was to quantitatively evaluate the stability of the skeletal and dental widths using cone-beam computed tomography (CBCT) after segmental Le Fort I osteotomy in adult patients with skeletal Class III malocclusion requiring maxillary expansion. The null hypothesis of this study was that the transverse dental and skeletal stability after maxillary expansion by segmental Le Fort 1 osteotomy is not satisfactory.
Adult patients who visited the first author's private dental clinic for orthognathic surgery between January 2014 and December 2015 were included in this study. CBCT was performed for skeletal evaluation in all patients, and all surgeries were performed by a single oral and maxillofacial surgeon. The patients were divided into two groups as follows: a control group, which included 25 (A point-nasion-B point angle [ANB], −2.35 ± 1.97°; 16 men and nine women; mean age, 22.48 ± 3.81 years) patients with skeletal Class III malocclusion who underwent Le Fort I osteotomy and bilateral sagittal split ramus osteotomy (BSSRO), and an experimental group, which included 36 (ANB, −2.97 ± 2.18°; 10 men and 26 women; mean age, 24.50 ± 6.19 years) patients with skeletal Class III malocclusion who underwent segmental Le Fort I osteotomy and BSSRO.
A surgery-first approach was used in 19 (76.0%) patients in the control group and 28 (77.8%) patients in the experimental group.
The inclusion criteria for this study were as follows: presence of both left and right maxillary first molars; no history of extraction or planned extraction for orthodontic treatment; availability of CBCT images obtained within 1 month before surgery, within 1 month after surgery, and at the end of treatment; no congenital deformity or trauma in the oral and maxillofacial region; and no previous history of orthodontic treatment for maxillary traction or expansion.
In the experimental group, both Le Fort I osteotomy and segmental osteotomy were performed. A wafer was used to fix the two segments after splitting. This wafer was maintained for 1 month after surgery, during which any additional fixture or orthodontic force was not applied (Figure 1). This study was approved by the institutional review board of Dankook University Dental Hospital (DKUDH IRB No. 2017-10-001).
CBCT was performed using Pax Reve3D (Vatech, Hwa-seong, Korea). During the scanning procedure, patients sat in an upright position while maintaining a natural head position, with the Frankfort horizontal plane (superior aspect of the external auditory canal to the infraorbital rim line) parallel to the ground. The imaging parameters were as follows: tube voltage, 80 kVp; tube current, 3.5 mA; shooting time, 10 seconds; field of view, 150 × 150 mm; and voxel size, 0.25 mm.
The acquired images were evaluated using Invivo5 (Anatomage, San Jose, CA, USA). For assessment of changes in the transverse width after maxillary segmental Le Fort I osteotomy, both skeletal and dental measurements were recorded.
For evaluation of changes in the width between the maxillary segments separated to both sides, the greater palatine foramen was used as a reference point.18 An axial reference plane was set to pass through the most medial point of the right and left greater palatine foramina, at the level of and parallel to the nasal floor. A coronal reference plane was set to pass through the most medial point of the right and left greater palatine foramina, at the level of the nasal floor and perpendicular to the axial reference plane. The width of the greater palatine foramen was measured between the narrowest part of the left and right foramina at the same vertical height as the nasal cavity floor on a coronal image (Figure 2).
Coronal CBCT images were reoriented such that the left and right mesiolingual cusp tips of the maxillary first molars were visible, and the dental width was measured between the cusp tips (Figure 3). These coronal images can appear similar to posteroanterior (PA) cephalograms, although their quality is compromised by the superimposition of various structures. Therefore, for accurate measurement of the dental width in this study, CBCT images were reoriented such that the two mesiolingual cusp tips appeared in a single image.
The dental and skeletal widths, referred to as M and GPF, respectively, were measured before (T1) and after (T2) surgery and at the end of treatment (T3).
All measurements were recorded by a single investigator. To test the intraexaminer reliability, 10 images were randomly selected for repeat measurements at 3 weeks after completion of the initial measurements.
All statistical analyses were performed using SPSS software (version 21.0; IBM Co., Armonk, NY, USA). An intraclass correlation test was performed to test the intraexaminer reliability.
Descriptive statistics were used, and the Shapiro-Wilk test was used to test the normality of the measured variables. Because all variables showed normal distribution, parametric statistics were used.
An independent t-test was performed to assess the significance of differences between the control and experimental groups, while paired t-tests were performed to compare changes after surgery and during the postoperative orthodontic treatment period within the experimental group.
In addition, Pearson's correlation analysis was performed to determine the correlation of the amount of postoperative relapse with the amount of maxillary impaction, amount of maxillary advancement, and amount of expansion between two segments in the experimental group.
The intraclass coefficients for measurement of the skeletal (0.941) and dental (0.923) widths indicated excellent intraexaminer reliability.
Table 1 presents descriptive statistics for the baseline characteristics of patients and the extent of surgery in both groups. There was no significant difference between groups in any parameter.
Table 2 shows the dental and skeletal widths measured at each time point. The dental width at T1 was significantly smaller in the experimental group (41.24 ± 4.57 mm) than in the control group (43.85 ± 3.16 mm). The amount of change in the dental width after surgery (T2-M to T1-M) was small in the control group (−0.31 ± 1.10 mm). However, significant expansion was achieved in the experimental group (1.83 ± 1.66 mm). There was no significant difference in the width at T2 between the two groups; this was maintained up to T3.
There was no significant difference in the skeletal width at T1 between the two groups (experimental group: 30.59 ± 2.51 mm, control group: 31.17 ± 2.39 mm). The amount of change in the skeletal width after surgery (T2-GPF to T1-GPF) was very small in the control group (−0.14 ± 0.80 mm). However, significant expansion was achieved in the experimental group (2.55 ± 1.94 mm). The width at T2 was significantly greater in the experimental group (33.14 ± 3.20 mm) than in the control group (31.03 ± 2.58 mm). During the postoperative orthodontic treatment period, the experimental group exhibited a significant decrease in the skeletal width (−0.67 ± 0.72 mm), unlike the control group (0.30 ± 0.87 mm).
In the control group, there was no significant difference in the skeletal width between T2 and T1 and between T3 and T2, although there was a significant decrease in the dental width (0.70 ± 1.28 mm) between T3 and T2, i.e., during the postoperative orthodontic treatment period (Table 2).
In the experimental group, there were significant differences in the dental and skeletal widths between all-time points (Table 2). Dental and skeletal expansion of 1.83 ± 1.66 and 2.55 ± 1.94 mm, respectively, was observed after surgery (between T2 and T1), while the dental and skeletal widths decreased by 1.41 and 0.67 mm, respectively, during the postoperative orthodontic treatment period (between T3 and T2). All relevant p-values are presented in Table 2.
In the experimental group, the amount of maxillary posterior impaction and advancement showed no correlation with the extent of changes in the postoperative dental and skeletal widths (p > 0.05), while the amount of skeletal expansion during surgery (T2-GPF to T1-GPF) showed a weak negative correlation with the amount of postoperative skeletal relapse (T3-GPF to T2-GPF; Pearson's correlation coefficient, −0.547; p = 0.001; Table 3).
In the present study, we quantitatively evaluated the stability of the skeletal and dental widths using CBCT after segmental Le Fort I osteotomy in adult patients with skeletal Class III malocclusion requiring maxillary expansion. We found that maxillary expansion via segmental Le Fort I osteotomy showed good stability, with a skeletal relapse rate of 26.3% over approximately 12 months.
Severe discrepancy in the dental and skeletal widths in fully grown adults requires a surgical approach. Two widely accepted methods are SARPE and segmental Le Fort I osteotomy, both of which are associated with a pattern of relapse, as observed with all other treatment methods. A significant amount of relapse after these procedures is accounted for by the effects of ligaments and soft tissues attempting to regress to their original state.12 During segmental Le Fort I osteotomy, the superior aspect of the maxillary bone does not contain any structures that induce relapse; however, the anterior and inferior aspects are covered by gingival tissue, which is a key factor for regression of the expanded maxillary width.19 A study by Phillips et al.20 that used dental casts reported a relapse of 30% and 49% in the transverse width between the left and right premolars and second molars, respectively, following approximately 2 years of follow-up after the completion of orthodontic treatment in patients who underwent segmental Le Fort 1 osteotomy. Marchetti et al.15 used dental casts to compare expansion and stability between SARPE and segmental Le Fort I osteotomy, although they only analyzed dental expansion in their study.
For the analysis of skeletal expansion and stability, PA cephalograms or CBCT images are necessary. In a study by Chamberland and Proffit21 that used PA cephalograms, jugular points were used as the reference points for measurement of the skeletal width. However, the maxillary buccal vestibule is located near the site of Le Fort I osteotomy, and the fixation plate and its boundary are not well defined. Consequently, it is difficult to obtain reproducible measurements from CBCT images. Accordingly, the greater palatine foramen was selected as the reference point for skeletal width measurements in the present study; this provided reproducible measurements and even facilitated measurements on CBCT images obtained immediately after surgery, which exhibit severe noise. Many previous studies have reported that the greater palatine foramen has excellent reproducibility as a reference point and allows easy measurements.18222324
There are almost no existing studies that used CBCT to observe skeletal and dental expansion after segmental Le Fort I osteotomy. This is because CBCT images obtained before and immediately after surgery, as well as those obtained from several months to several years after surgery, must be available for the evaluation of both expansion and relapse. In 2014, Yao et al.18 used CBCT to evaluate skeletal and dental expansion and relapse after segmental Le Fort I osteotomy and reported skeletal expansion of 3.43 mm relative to the greater palatine foramen, with a relapse of 0.86 mm (approximately 25%) over 9 months. In the present study, the amount of skeletal expansion after segmental Le Fort I osteotomy was 2.55 mm, while the amount of relapse was 0.67 mm or 26.3%, which was similar to the amount reported by Yao et al.18 The amount of expansion in the present study was somewhat smaller than that reported by Yao et al.18 (2.55 mm vs. 3.43 mm); however, because the amount of maxillary expansion achieved via segmental Le Fort I osteotomy reflects the actual amount of expansion required, it is difficult to make direct comparisons between the two studies. Moreover, at our dental clinic, segmental Le Fort I osteotomy is aggressively performed to establish stable occlusion by addressing not only width discrepancies but also buccolingual tipping problems and premature contact areas in the molars. As a result, the amount of expansion, on an average, may have been somewhat small. Another study conducted in 2015 by Seeberger et al.13 also used CBCT, although only images obtained at the initial examination and 9 months after surgery were assessed, because of which the amount of decrease in the width from the immediate postoperative period to 9 months after surgery could not be determined.
In the present study, the experimental group exhibited dental expansion of 1.83 mm after segmental Le Fort I osteotomy, which was followed by a decrease of 1.41 mm in the dental width by the end of treatment. Thus, the relapse rate was 77.0%, which was higher than that (20–50%) reported in other studies.152025 A surgery-first approach was used for 28 of the 36 patients (77.8%) in the experimental group. Patients with skeletal Class III malocclusion and a narrow maxillary arch often exhibit buccal tipping of the maxillary molars as a compensatory mechanism. When orthodontic treatment is performed before surgery, buccal tipping of the maxillary molars is sufficiently decompensated. With the surgery-first approach, however, buccal tipping of the maxillary molars begins to return to the original level once orthodontic treatment is initiated after surgery This could be a reason for a decrease in the width between the mesiolingual cusps of the maxillary first molars after surgery; the dental width also decreased by 0.70 mm during the postoperative orthodontic treatment period in the control group. Because the distance between the greater palatine foramina, i.e., the skeletal width, was maintained better than the dental width (77% decrease vs. 26% decrease), it would be difficult to interpret this result as poor stability after segmental Le Fort I osteotomy.
To investigate factors that influence relapse in the maxillary width expanded via segmental Le Fort I osteotomy, the correlation of the amount of postoperative relapse with the amount of maxillary posterior impaction, amount of maxillary advancement, and amount of expansion between two segments after splitting was analyzed in the experimental group (Table 3). There was a mild negative correlation between the amount of skeletal expansion and the amount of skeletal relapse, which indicated that an increased amount of skeletal expansion results in a greater amount of relapse. The palatal gingival tissue and buccal soft tissue and muscles may also cause relapse in the expanded maxillary bone. When a greater amount of expansion is planned, methods such as the use of an absorbable plate in the palatal region, bone grafting in the area of expansion, and the use of a transpalatal arch for width maintenance may be recommended. According to a study by Kretschmer et al.,26 the use of an absorbable plate in the palatal region or bone grafting in the expanded palatal region did not have any significant influence on the relapse rate. However, the sample size in that study was very small, and additional studies with well-controlled conditions are necessary to validate their findings.
SARPE and segmental Le Fort I osteotomy are often compared as techniques used for patients with severe maxillary deficiency. Chamberland and Proffit21 analyzed changes in the amount of postoperative expansion by measuring the distance between the left and right jugular points on PA cephalograms obtained from patients who underwent SARPE. They reported that the amounts of dental expansion and relapse were approximately 5.5 to 8 mm and 25% to 59%, respectively, depending on the tooth, while the skeletal width barely changed. In the study by Yao et al.,18 a greater amount of dental expansion in the molar region was achieved with SARPE, while a greater amount of skeletal expansion was achieved with segmental Le Fort I osteotomy. In that study, segmental Le Fort I osteotomy was performed when the dental width was deficient by 3 to 6 mm, while SARPE was performed when the width was deficient by ≥ 6 mm. Accordingly, the greater amount of dental expansion achieved with SARPE may be an obvious outcome. However, a greater amount of skeletal expansion was achieved with segmental Le Fort I osteotomy; therefore, the percentage of dental expansion relative to that of skeletal expansion was higher with SARPE. This indicated that expansion by SARPE occurred in the form of skeletal tipping, whereas that by segmental Le Fort I osteotomy occurred in a parallel manner when viewed from the front. In the present study, the amounts of postoperative dental and skeletal expansion were 1.83 and 2.55 mm, respectively, which indicated that maxillary expansion occurred in a nearly parallel manner. In the study by Yao et al.,18 dental relapse was greater with SARPE than with segmental Le Fort I osteotomy, although the pattern (decreasing pattern) was similar. Interestingly, segmental Le Fort I osteotomy was associated with a decrease in the skeletal width over time, whereas SARPE was associated with a slight increase in the skeletal width over time. This pattern was also observed in the 2011 study by Chamberland and Proffit27 The reason for these findings is the nature of the technique. Because SARPE does not involve downfracture of the posterior maxilla, skeletal expansion does not occur over a short period of time; rather, gradual expansion occurs as the built up internal stress is released over time.
A possible limitation of this study is the inclusion of patients who received a surgery-first approach as well as those who underwent conventional surgery in the experimental and control groups. To clarify the results, we analyzed only those patients who received the surgery-first approach in both groups and found the same results. Only T3-GPF showed different findings; it was not significantly different between the control and experimental groups (31.33 mm vs. 32.48 mm, p = 0.132), although the difference became significant when only patients who received the surgery-first approach were analyzed (30.63 mm vs. 32.84 mm, p = 0.015). This means that the expanded skeletal width in the experimental group was favorably maintained at T3.
Segmental Le Fort I osteotomy enables expansion in any direction. Accordingly, to analyze the three-dimensional movement of the segment, we initially decided to measure the intercanine width and corresponding anterior skeletal width (width of piriform aperture). However, surgical plates in close proximity to the piriform aperture resulted in radial artifacts, because of which we could not obtain accurate measurements of the aperture width. Therefore, the intercanine width and piriform aperture width were not measured in our study. The small sample size and the lack of long-term follow-up data are other limitations of our study. Future studies with large sample sizes and long-term follow-up data are desirable.
In conclusion, our findings suggest that maxillary expansion via segmental Le Fort I osteotomy results in favorable postoperative stability, as observed by the skeletal relapse rate of 26% over approximately 12 months. However, a greater amount of expansion requires greater efforts to prevent relapse. Various methods such as the use of absorbable plates in the palatal region, bone grafting in the area of expansion, and placement of a transpalatal arch may aid in maintenance of the expanded width in such situations.
Figures and Tables
Figure 1
Segmental Le Fort I osteotomy in an adult patient with skeletal Class III malocclusion. Maintenance of the expanded maxillary width using a surgical wafer.

Figure 2
Measurement of the skeletal width. Measurement of the distance between the right and left greater palatine foramina on a coronal cone-beam computed tomography image.
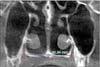
Figure 3
Measurement of the dental width. Measurement of the distance between the right and left mesiolingual cusps of the first molars on a coronal cone-beam computed tomography image.

Table 1
Baseline (T1) characteristics of patients and the extent of Le Fort I osteotomy in the control and experimental groups

Table 2
Mean dental and skeletal widths and changes in the widths at different time points before and after surgery in the control and experimental groups

Control group, Le Fort I osteotomy; experimental group, segmental Le Fort I osteotomy; SD, standard deviation; T1, before surgery; T2, after surgery; T3, end of treatment; M, dental width; GPF, skeletal width.
*p<0.05; comparison between groups using independent t-test or comparison within group using paired t-test.
References
1. Kook YA, Park JH, Bayome M, Kim S, Han E, Kim CH. Distalization of the mandibular dentition with a ramal plate for skeletal Class III malocclusion correction. Am J Orthod Dentofacial Orthop. 2016; 150:364–377.

2. Jing Y, Han X, Guo Y, Li J, Bai D. Nonsurgical correction of a Class III malocclusion in an adult by miniscrew-assisted mandibular dentition distalization. Am J Orthod Dentofacial Orthop. 2013; 143:877–887.

3. Suh HY, Lee SJ, Park HS. Use of mini-implants to avoid maxillary surgery for Class III mandibular prognathic patient: a long-term post-retention case. Korean J Orthod. 2014; 44:342–349.

4. Posnick JC, Adachie A, Choi E. Segmental maxillary osteotomies in conjunction with bimaxillary orthognathic surgery: indications - safety - outcome. J Oral Maxillofac Surg. 2016; 74:1422–1440.

5. Franchi L, Baccetti T. Transverse maxillary deficiency in Class II and Class III malocclusions: a cephalometric and morphometric study on postero-anterior films. Orthod Craniofac Res. 2005; 8:21–28.

6. Haas AJ. Rapid expansion of the maxillary dental arch and nasal cavity by opening the mid-palatal suture. Angle Orthod. 1961; 31:73–90.
7. Timms DJ. A study of basal movement with rapid maxillary expansion. Am J Orthod. 1980; 77:500–507.

8. Wertz RA. Skeletal and dental changes accompanying rapid midpalatal suture opening. Am J Orthod. 1970; 58:41–66.

9. Timms DJ, Moss JP. An histological investigation into the effects of rapid maxillary expansion on the teeth and their supporting tissues. Trans Eur Orthod Soc. 1971; 263–271.
10. Lee KJ, Park YC, Park JY, Hwang WS. Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am J Orthod Dentofacial Orthop. 2010; 137:830–839.

11. Choi SH, Cha JY, Kang DY, Hwang CJ. Surgical-orthodontic treatment for skeletal class II malocclusion with vertical maxillary excess, anterior open bite, and transverse maxillary deficiency. J Craniofac Surg. 2012; 23:e531–e535.

12. Starch-Jensen T, Blæhr TL. Transverse expansion and stability after segmental Le fort I osteotomy versus surgically assisted rapid maxillary expansion: a systematic review. J Oral Maxillofac Res. 2016; 7:e1.

13. Seeberger R, Gander E, Hoffmann J, Engel M. Surgical management of cross-bites in orthognathic surgery: Surgically assisted rapid maxillary expansion (SARME) versus two-piece maxilla. J Craniomaxillofac Surg. 2015; 43:1109–1112.

14. Gurgel JA, Tiago CM, Normando D. Transverse changes after surgically assisted rapid palatal expansion. Int J Oral Maxillofac Surg. 2014; 43:316–322.

15. Marchetti C, Pironi M, Bianchi A, Musci A. Surgically assisted rapid palatal expansion vs. segmental Le Fort I osteotomy: transverse stability over a 2-year period. J Craniomaxillofac Surg. 2009; 37:74–78.

16. Steinhauser EW. Midline splitting of the maxilla for correction of malocclusion. J Oral Surg. 1972; 30:413–422.
17. Lee HW, Kim SJ, Kwon YD. Salvage rapid maxillary expansion for the relapse of maxillary transverse expansion after Le Fort I with parasagittal osteotomy. J Korean Assoc Oral Maxillofac Surg. 2015; 41:97–101.

18. Yao W, Bekmezian S, Hardy D, Kushner HW, Miller AJ, Huang JC, et al. Cone-beam computed tomographic comparison of surgically assisted rapid palatal expansion and multipiece Le Fort I osteotomy. J Oral Maxillofac Surg. 2015; 73:499–508.

19. Proffit WR, Turvey TA, Phillips C. The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: an update and extension. Head Face Med. 2007; 3:21.

20. Phillips C, Medland WH, Fields HW Jr, Proffit WR, White RP Jr. Stability of surgical maxillary expansion. Int J Adult Orthodon Orthognath Surg. 1992; 7:139–146.
21. Chamberland S, Proffit WR. Closer look at the stability of surgically assisted rapid palatal expansion. J Oral Maxillofac Surg. 2008; 66:1895–1900.

22. Goldenberg DC, Goldenberg FC, Alonso N, Gebrin ES, Amaral TS, Scanavini MA, et al. Hyrax appliance opening and pattern of skeletal maxillary expansion after surgically assisted rapid palatal expansion: a computed tomography evaluation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:812–819.

23. Goldenberg DC, Alonso N, Goldenberg FC, Gebrin ES, Amaral TS, Scanavini MA, et al. Using computed tomography to evaluate maxillary changes after surgically assisted rapid palatal expansion. J Craniofac Surg. 2007; 18:302–311.

24. Podesser B, Williams S, Bantleon HP, Imhof H. Quantitation of transverse maxillary dimensions using computed tomography: a methodological and reproducibility study. Eur J Orthod. 2004; 26:209–215.

25. Proffit WR, Turvey TA, Phillips C. Orthognathic surgery: a hierarchy of stability. Int J Adult Orthodon Orthognath Surg. 1996; 11:191–204.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download