Abstract
Piezoelectric surgery is a novel surgical approach used in orthodontic treatment for rapid tooth movement. This paper presents a case series wherein osseous outgrowths were observed in response to piezosurgery-assisted en-masse retraction. Sixteen patients requiring upper premolar extractions were treated with miniscrew-supported en-masse retraction and received minimally invasive decortication via piezosurgery. Computed tomography (CT) of the maxillary anterior region was performed to investigate the nature of the outgrowths. In 8 of the 16 patients, hemispheric or disc-shaped osseous outgrowths were observed on the sites where piezosurgery was performed during retraction. CT images revealed that these outgrowths were alveolar bone. This case series presents a previously unreported osseous response to piezosurgery-assisted tooth movement during orthodontic treatment. The response is mostly transient and is observed in 50% of the treated patients, suggesting a bone turnover that can be assessed clinically and radiographically.
Accelerated orthodontic tooth movement can be achieved using various strategies ranging from invasive surgical decortication1234 to non-invasive methods such as photobiomodulation and vibration.567 Among the surgery-assisted techniques, piezoelectric surgery is a minimally invasive method that has been introduced to the dental practice by Vercellotti et al.8 The rationale behind this approach is to minimize the invasiveness of selective decortications and overcome the heat generated by diamond and carbide burs, which could potentially lead to marginal osteonecrosis and impaired alveolar regeneration.910 Piezosurgery permits safer cuts while producing substantially less collateral tissue damage and results in better healing and reduced risk of postoperative necrosis.111213 The aim of using piezosurgery in conjunction with orthodontic therapy is to promote intensified alveolar resorption in order to reduce treatment time by enhancing the rate of tooth movement. While protocols have been standardized and successful clinical results have been obtained in animals and humans, the tissue response to and turnover rates of piezosurgery-assisted orthodontic tooth movement in humans have remained unknown.91415161718
We have treated a series of cases by using piezosurgery- assisted en-masse retraction and observed transient osseous outgrowths in 50% of these cases. Therefore, the aim of this study was to present and discuss the tissue response to piezoelectric surgery during en-masse retraction.
Sixteen patients (average age, 17.7 ± 3.4 years) whose treatment plan called for premolar extractions were treated using miniscrew-supported en-masse retraction after obtaining formal approval from the ethical committee of Baskent University (Ankara, Turkey). Patients were also expected to meet the following criteria: no systemic disease or drug use that would affect the tooth movement rate, minimum age at the beginning of retraction of 14 years and above, full permanent dentition, no previous orthodontic treatment history, and adequate oral hygiene. All of the patients received 0.018 × 0.025-inch incisor and canine brackets and 0.022 × 0.028-inch premolar brackets and molar tubes (MBT prescription; 3M Unitek, Monrovia, CA, USA) for reducing friction during retraction. To further prevent friction at the posterior segment, bonding of the second molars were postponed until the end of retraction. When the maxillary dental arches were fully leveled and aligned, piezoelectric surgery was performed. Without reflecting a full periodontal flap, vertical soft-tissue incisions from canine-to-canine were made on the buccal side in the interradicular areas, at the midroot level under local infiltration anesthesia. Seven piezosurgical cuts were made with a depth-coded piezoelectric knife (SG1, VarioSurg; NSK, Hoffman Estates, IL, USA). These cuts were limited to a 3-mm depth, cutting both the cortical and medullary bones. Due importance was given to apply minimal pressure and avoid overheating. All of the soft-tissue incisions were then sutured with a 4–0 vicryl suture (Ethicon®; Johnson & Johnson, Irvine, CA, USA) and retained for a week. All surgical procedures were performed by an experienced periodontist (B.F.O.).
During the same session, en-masse retraction was initiated on a 0.016 × 0.022-inch stainless steel archwire with 7-mm-long power hooks (Ortho Organizers Inc., Carlsbad, CA, USA) placed distal to the lateral incisors. Two miniscrews with 1.5- to 1.4-mm diameter and 7-mm length (AbsoAnchor; Dentos, Daegu, Korea) were placed between the roots of the second premolars and first molars on both sides. From these miniscrews, nickel-titanium closed coil springs (Ormco Corp., Orange, CA, USA), exerting 250 g of force per side, were attached to the power hooks anteriorly. Computed tomography (CT) images were acquired at the beginning and end of retraction to identify the nature of the outgrowths. Moreover, three-dimensional superimposition was performed with the best-fit method, and axial images acquired from the same height were compared.
After piezosurgery, eight of the 16 patients manifested osseous outgrowths during retraction on the surgical sites. These outgrowths appeared in the interradicular areas and in the middle third of the maxillary incisor and canine roots. The outgrowths were assumed to be alveolar tissue based on the fact that their structural properties presented continuity with the alveolar bone on the CT slices. The following cases are representative and illustrate the clinical and radiographical characteristics of tissue response in these cases.
An 18-year-old female patient had a chief complaint of unpleasant appearance upon smiling. She had class I molar relationship, severely proclined incisors, and 4.6 mm of anterior open bite. In order to reduce the proclination of the incisors, achieve an ideal overbite, and increase incisor exposure upon smiling, the maxillary and mandibular first premolars were extracted.
In the second month of retraction, osseous outgrowths resembling hemispheres started appearing in the maxilla where piezosurgery was performed. These curved and solitary outgrowths then consolidated and formed flatter and larger ones mesiodistally. At the end of the treatment, a significant reduction was observed (Figure 1). The retraction time was 12 months.
A 16-year-old female patient had a chief complaint of protrusive upper teeth. She had a mild skeletal class 2 and Angle class II, division 1 malocclusion. The treatment plan called for extraction of the maxillary first premolars.
Two solitary osseous outgrowths emerged during the second month of retraction: a bigger one between the right central and lateral incisors, and a smaller one between the right lateral incisor and canine (Figure 2). The osseous outgrowths had not regressed spontaneously until the end of treatment (Figure 3). The retraction took 11 months.
A 22-year-old female patient had a chief complaint of aesthetically unpleasing appearance of her teeth. She had proclined incisors, class I molar relationship, increased overjet, and decreased overbite. She was a carrier for hepatitis C, for which she was receiving vaccination. The objectives were to reduce incisor proclination, achieve ideal overjet and overbite, and reduce the prominence of the lips. The treatment plan was to extract four first premolars.
The most extensive and severe osseous outgrowths were seen in this patient, and these were visible from the first month. Nine months after debonding, these outgrowths were still apparent; however, a significant regression was observed (Figure 4). The retraction time was 11 months.
In this case series, we found that 50% of the patients treated with piezosurgery-assisted en-masse retraction manifested torus-like osseous outgrowths on the buccal surface of the maxilla. CT images from the maxillary anterior region support the assumption that the true nature of these outgrowths is bony tissue. Our study, however, was not the first to show bone modeling after piezoelectric surgery. Preti et al.19 showed in a pilot study that bone around the implants treated with piezoelectric bone surgery exhibited an earlier increase in growth factors as well as consistently more active neo-osteogenesis. Di Alberti et al.20 also found that piezoelectric implant site preparation promoted better bone density and osteogenesis. Taken together with the findings of these studies in the literature, our findings lead to the conclusion that piezoelectric bone surgery seems to encourage neo-osteogenesis by anabolic bone modeling.
In the orthodontic literature, not only piezosurgery but also decortication with rotary instruments is associated with increased appositional activity. In the study by Baloul et al.,14 the levels of osteoprotegerin, a molecule responsible from inhibiting osteoclastogenesis, were elevated after decortication-assisted tooth movement. This shows that a coupled mechanism of bone resorption and apposition takes place during the earlier stages of treatment. However, osseous outgrowths were not reported after any of the surgery-assisted techniques other than piezosurgery in the literature. Ultrasonic vibrations are believed to support increased bone deposition after piezoelectric surgery because cell proliferation, migration, and matrix synthesis are promoted by vibrations.152122 Therefore, the amphoteric nature of piezoelectric surgery may inherently be causing a more extensive and diffuse alveolar remodeling process.16 Furthermore, heavy orthodontic forces acting on the alveolar bone through the anterior teeth might amplify this effect. Because none of the previous studies in the literature using piezoelectric surgery for rapid tooth movement reported a similar bone remodeling activity, we believe that heavy orthodontic forces are effective in the occurrence of these outgrowths.
Another explanation for these protrusions could be the blistering of adjacent soft tissues because of overheating.23 If the piezotome is used without sufficient coolant irrigation or if the tip is moved too deep for the irrigation to be effective, the bone and adjacent soft tissues can be burned. However, in our study, not only irrigation from the piezotome itself, but also a secondary syringe of water was used in order to prevent overheating. Moreover, the piezotome was only moved to a depth of 3 mm, which is relatively shallow. Furthermore, all of the surgical procedures were performed by an experienced periodontist. Therefore, if the surgical technique was imprecise right from the beginning, then all of the treated patients would be expected to present these outgrowths. In addition to these, CT images support the opinion that these outgrowths were indeed of bony origin. Therefore, the possibility of soft-tissue blistering can be ruled out. At this point, a bone biopsy could have provided a more accurate diagnosis; however, the ethical committee of our university rejected our request for a second surgery for only diagnostic and non-therapeutic reasons.
The most severe case of osseous outgrowths was seen in the patient who was a carrier for hepatitis C. In the study by Schiefke et al.,24 significantly reduced bone mineral density and alterations of bone metabolism were reported in non-cirrhotic chronic hepatitis C infection. This information, in concurrence with ours, shows that systemic diseases may have some effects on the results of dental surgeries and due importance must be given to the medical history of patients.
This case series presents a previously unreported osseous response to piezosurgery-assisted tooth movement during orthodontic treatment. Neo-osteogenesis after piezosurgery might be beneficial; however, this might be an unpleasing condition if the patient has increased gingival exposure upon smiling. Therefore, the amount of gingival display should be taken into consideration when deciding to perform piezosurgery on the anterior surface of the maxilla. The response is mostly transient; however, long-term follow-up should be encouraged because spontaneous regression of these formations is still unknown.
Figures and Tables
Figure 1
A, Computed tomography (CT) image (axial slice) from the maxillary anterior region acquired from Patient 1 at the beginning of retraction. B, Osseous outgrowths at the end of retraction. C, CT image from the maxillary anterior region acquired at the end of retraction. D, Significant regression at the end of treatment.
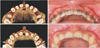
Figure 2
A, Computed tomography (CT) image (axial slice) from the maxillary anterior region acquired from Patient 2 at the beginning of retraction. B, Two osseous outgrowths: a bigger one between the right central and lateral incisors, and a smaller one between the right lateral incisor and canine. C, CT image from the maxillary anterior region acquired at the end of retraction. D, Osseous outgrowths at the end of treatment.
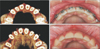
Figure 3
The three-dimensional superimposition of computed tomography images acquired at the beginning and end of retraction. The image in brown is the one acquired at the beginning of retraction, and the image in green is the one acquired at the end of retraction.

Figure 4
A, Computed tomography (CT) image (axial slice) from the maxillary anterior region acquired from Patient 3 at the beginning of retraction. B, Extensive osseous outgrowths on the buccal maxilla during retraction. C, CT image from the maxillary anterior region acquired at the end of retraction. D, Osseous outgrowths 9 months after debonding.

References
1. Kole H. Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg Oral Med Oral Pathol. 1959; 12:515–529.

2. Wilcko WM, Wilcko MT, Bouquot JE, Ferguson DJ. Accelerated orthodontics with alveolar reshaping. J Ortho Practice. 2000; 10:63–70.
3. Wilcko WM, Wilcko T, Bouquot JE, Ferguson DJ. Rapid orthodontics with alveolar reshaping: two case reports of decrowding. Int J Periodontics Restorative Dent. 2001; 21:9–19.
4. Wilcko MT, Wilcko WM, Pulver JJ, Bissada NF, Bouquot JE. Accelerated osteogenic orthodontics technique: a 1-stage surgically facilitated rapid orthodontic technique with alveolar augmentation. J Oral Maxillofac Surg. 2009; 67:2149–2159.

5. Shaughnessy T, Kantarci A, Kau CH, Skrenes D, Skrenes S, Ma D. Intraoral photobiomodulation-induced orthodontic tooth alignment: a preliminary study. BMC Oral Health. 2016; 16:3.

6. Kau CH, Kantarci A, Shaughnessy T, Vachiramon A, Santiwong P, de la Fuente A, et al. Photobiomodulation accelerates orthodontic alignment in the early phase of treatment. Prog Orthod. 2013; 14:30.

7. Pavlin D, Anthony R, Raj V, Gakunga PT. Cyclic loading (vibration) accelerates tooth movement in orthodontic patients: a double-blind, randomized controlled trial. Semin Orthod. 2015; 21:187–194.

8. Vercellotti T, Nevins ML, Kim DM, Nevins M, Wada K, Schenk RK, et al. Osseous response following resective therapy with piezosurgery. Int J Periodontics Restorative Dent. 2005; 25:543–549.
9. Dibart S, Surmenian J, Sebaoun JD, Montesani L. Rapid treatment of Class II malocclusion with piezocision: two case reports. Int J Periodontics Restorative Dent. 2010; 30:487–493.
10. Kerawala CJ, Martin IC, Allan W, Williams ED. The effects of operator technique and bur design on temperature during osseous preparation for osteosynthesis self-tapping screws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 88:145–150.

11. Aro H, Kallioniemi H, Aho AJ, Kellokumpu-Lehtinen P. Ultrasonic device in bone cutting. A histological and scanning electron microscopical study. Acta Orthop Scand. 1981; 52:5–10.

12. Vercellotti T, Crovace A, Palermo A, Molfetta A. The piezoelectric osteotomy in orthopedics: Clinical and histological evaluations (Pilot study in animals). Mediterr J Surg Med. 2001; 9:89–96.
13. Horton JE, Tarpley TM Jr, Wood LD. The healing of surgical defects in alveolar bone produced with ultrasonic instrumentation, chisel, and rotary bur. Oral Surg Oral Med Oral Pathol. 1975; 39:536–546.

14. Baloul SS, Gerstenfeld LC, Morgan EF, Carvalho RS, Van Dyke TE, Kantarci A. Mechanism of action and morphologic changes in the alveolar bone in response to selective alveolar decortication-facilitated tooth movement. Am J Orthod Dentofacial Orthop. 2011; 139:4 Suppl. S83–S101.

15. Huang H, Williams RC, Kyrkanides S. Accelerated orthodontic tooth movement: molecular mechanisms. Am J Orthod Dentofacial Orthop. 2014; 146:620–632.

16. Dibart S, Yee C, Surmenian J, Sebaoun JD, Baloul S, Goguet-Surmenian E, et al. Tissue response during Piezocision-assisted tooth movement: a histological study in rats. Eur J Orthod. 2014; 36:457–464.

17. Dibart S, Sebaoun JD, Surmenian J. Piezocision: a minimally invasive, periodontally accelerated orthodontic tooth movement procedure. Compend Contin Educ Dent. 346; 30:342–344. 346348–350.
18. Keser EI, Dibart S. Sequential piezocision: a novel approach to accelerated orthodontic treatment. Am J Orthod Dentofacial Orthop. 2013; 144:879–889.

19. Preti G, Martinasso G, Peirone B, Navone R, Manzella C, Muzio G, et al. Cytokines and growth factors involved in the osseointegration of oral titanium implants positioned using piezoelectric bone surgery versus a drill technique: a pilot study in minipigs. J Periodontol. 2007; 78:716–722.

20. Di Alberti L, Donnini F, Di Alberti C, Camerino M. A comparative study of bone densitometry during osseointegration: piezoelectric surgery versus rotary protocols. Quintessence Int. 2010; 41:639–644.
21. Ramli R, Reher P, Harris M, Meghji S. The effect of ultrasound on angiogenesis: an in vivo study using the chick chorioallantoic membrane. Int J Oral Maxillofac Implants. 2009; 24:591–596.
22. Della Rocca GJ. The science of ultrasound therapy for fracture healing. Indian J Orthop. 2009; 43:121–126.

23. Polatsch DB, Baskies MA, Hommen JP, Egol KA, Koval KJ. Tape blisters that develop after hip fracture surgery: a retrospective series and a review of the literature. Am J Orthop (Belle Mead NJ). 2004; 33:452–456.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download