INTRODUCTION
Skeletal Class II malocclusion can result from either maxillary protrusion, mandibular retrusion, or a combination of the two.
12 In cases of growing patients with skeletal Class II malocclusion with mandible retrusion, the Class II Twin-block appliance can be used to stimulate and enhance mandibular growth. This appliance, originally developed by Dr. William J. Clark, consists of upper and lower removable plates. In comparison with removable functional monoblocks, the appliance's separate plates and a less bulky appearance improve patient compliance and increase the time for which the subjects wear the appliance.
3
In Class II Twin-block treatment, lower facial soft-tissue adaptation can occur in response to mandibular advancement. Previous studies that used lateral cephalometric radiographs that investigated the skeletal, dental, and soft-tissue effects of the Class II Twin-block appliance have reported reduced maxillomandibular discrepancy, decreased overjet, and advancement of the lower lip and chin point in response to mandibular growth stimulation.
4567
Orthodontic treatment is predominately used to improve facial esthetics. Since the demand for facial attractiveness is increasing, facial profile improvement, with a focus on soft-tissue changes, has become more important. Previous studies investigating the effect of the Class II Twin-block appliance have shown esthetic improvement of the facial profile.
68 However, individual variation in the response to Class II functional appliance treatment has also been reported, with some patients exhibiting poor facial profile improvement after treatment.
910
Several studies investigating successful Class II functional treatment outcomes have proposed several cephalometric predictors including pretreatment overjet and overbite, sella-nasion-point B angle (SNB), maxillary-mandibular plane angle, point A-nasion-point B angle (ANB), and condylar angle.
101112 However, these studies defined treatment success based on hard-tissue changes, such as the reduction of anterior overjet. To date, no studies have investigated the predictors of successful Class II Twin-block appliance treatment based on soft-tissue profile outcomes. Therefore, the aim of this retrospective study was to determine factors related to the successful outcomes of Class II Twin-block appliance treatment based on the evaluation of soft-tissue profile changes in growing patients with skeletal Class II malocclusion.
MATERIALS AND METHODS
The pre- and post-treatment lateral cephalometric records of 45 patients (35 boys and 10 girls) treated with the Class II Twin-block appliance were collected. The mean (± standard deviation [SD]) age of the patients at the start of treatment was 10.4 ± 1.2 years. For all the patients, lateral cephalometric radiographs were taken with the teeth in occlusion and the lips in the resting position. The study protocol was approved by the Institutional Review Board of Kyung Hee University Hospital at Gangdong (IRB approval No. 2014-10-022). Patient inclusion criteria were as follows:
A diagnosis of Skeletal Class II relationship with mandibular deficiency,
Class I molar relationship and normal overjet/overbite obtained after treatment,
Only received treatment with the Class II Twin-block appliance,
No craniofacial syndrome or congenital maxillofacial deformity,
No congenital missing tooth or teeth which affected the facial profile.
A modified form of Dr. Clark's Twin-block appliance comprising two separate, upper and lower, removable appliances was used in this study (
Figure 1). The bite registration was taken with the incisors in an edge-to-edge position with at least a 5-mm vertical posterior opening. All patients were instructed to wear the appliance 24 hours per day (except when eating). The mean (± SD) total treatment time of these patients was 10 ± 3.9 months.
Profile silhouettes were produced from the soft-tissue profile tracings of the pre- and post-treatment lateral cephalograms by the same operator (
Figure 2).
13 The tracings were arranged with the Frankfort line parallel to the horizontal aspect of the computer monitor and were saved as JPEG images. Using a photo editor program, the profile tracings were filled in black, against a white background, and were standardized for size and range, from the soft-tissue glabella to slightly below the throat point.
For each patient, the silhouette pairs (pre- and posttreatment) were randomly assigned a number (1–45) and were inserted on the same sheet: pre-treatment image on the left side and post-treatment image on the right (
Figure 2). The extent of silhouette improvement was evaluated by a panel comprised of three orthodontists, each with an orthodontic experience of more than 10 years. The panel was provided with an explanation of the study and allowed 10 seconds to view each silhouette pair. The panel then recorded the extent of the silhouette improvement following treatment by using an unmarked 100-mm visual analogue scale (VAS) from 0 (no improvement of facial profile) to 100 (facial profile improved close to Class I).
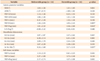
Patients were then divided into two groups based on their VAS scores: a favorable group comprising the upper 30% of VAS scores, and an unfavorable group comprising the lower 30%. Pre- and post-treatment lateral cephalograms of each group were traced and analyzed by one operator. Landmarks used in the study are presented in
Table 1 and
Figure 3A, while the linear and angular measurements are shown in
Table 2 and
Figure 3B–3D.
14
Statistical analysis
Cephalometric tracings and analysis were performed by one operator using the software program V ceph™ 6.0 (Osstem Inc., Seoul, Korea). Twenty randomly selected lateral cephalograms were traced 2 weeks after the first measurements were taken. The error of the first and second measurements was compared using Dahlberg's formula. All statistical analyses were performed using PASW Statistics for Windows, version 18.0 (IBM Co., Armonk, NY, USA). A normal distribution of the variables was confirmed using the Kolmogorov-Smirnov test. Statistical comparison of the pre-treatment measurements between the favorable and unfavorable groups was performed using an independent t-test. A logistic regression test was performed to determine the most highly correlated factor among the pretreatment variables and an intra-class correlation coefficient was used to determine intra-panel reliability; a high correlation coefficient (0.895) was recorded between the orthodontists within the panel.
RESULTS
Analysis using Dahlberg's formula revealed that the linear measurement error varied between 0.20 mm (lower anterior facial height) and 1.23 mm (condylion to gonion length), and the angular measurement error varied between 0.54° (sella-nasion line [SN] to pogonion angle) and 1.21° (upper incisor to maxillary plane angle [MxP]). The favorable group was comprised with 14 subjects (mean age, 10.5 ± 1.4 years; 12 boys and 2 girls) and the unfavorable group was comprised with 14 subjects (mean age, 10.4 ± 1.3 years; 12 boys and 2 girls).
Table 3 presents the comparative data for pre-treatment cephalometric measurements in both groups. An independent
t-test indicated that there were statistically significant pre-treatment cephalometric differences in symphysis inclination, lower incisor to mandibular plane angle (IMPA), lower incisor to occlusal plane angle (L1 to Occ), lower incisor to pogonion distance (L1 to pogonion), ANB, SN to MxP, SN to mandibular plane angle (MnP), and gonial angle between the two groups. With the exception of L1 to Occ, the favorable group had the lowest cephalometric measurements. There were no statistically significant differences in pre-treatment soft-tissue measurements between the two groups.
Table 4 presents the cephalometric treatment changes; statistically significant differences were observed in the gonial angle, vertical reference plane (VRP) to B point, and VRP to pogonion between the two groups. Increase in gonial angle, VRP to B point, and VRP to pogonion following treatment were significantly larger in the favorable group compared to the unfavorable group.
Logistic regression analysis was used to determine the predictors of favorable soft-tissue profile outcomes. With one independent variable, L1 to pogonion was the most effective predictor with a coefficient of determination of 0.473, and with two independent variables, the IMPA and gonial angle were the most strongly related variables, with a coefficient of determination of 0.719. In combination with L1 to pogonion, the coefficient of determination was 0.751, and this increased to 0.818 when combined with the vertical factor SN to MxP.
DISCUSSION
After Class II Twin-block treatment, the extent of soft-tissue profile improvement among patients was variable, despite the fact that treatment resulted in Class I molar relationship and normal overjet and overbite in all the patients. Some patients exhibited an excellent profile improvement, obtaining almost a Class I orthognathic profile, while some exhibited extremely small profile changes, retaining a retrognathic appearance. Other patients also showed profile improvement however, it was not enough to classify as a straight profile. The objective of this study was to determine factors related to favorable soft-tissue profile outcomes following Class II Twin-block treatment.
The findings revealed that in the favorable group, there was a relationship between a favorable soft-tissue profile response and several pre-treatment cephalometric features, including a smaller symphysis inclination, IMPA, L1 to pogonion, ANB, SN to MxP, SN to MnP, and gonial angle, as well as a larger L1 to Occ. A logistic regression analysis showed that the effective predictors of favorable treatment outcomes were L1 to pogonion, IMPA, gonial angle, and SN to MxP. The size of the coefficient of determination with IMPA and gonial angle (0.719) suggests that these two features alone may act as useful predictors of favorable profile improvement. This suggests that clinicians can expect more soft-tissue profile improvements when using the Class II Twin-block appliance in patients with a small IMPA and gonial angle.
Cephalometric characteristics of patients with improved soft-tissue profiles after Class II Twin-block treatment can be summarized as reduced lower incisor protrusion and low divergent skeletal patterns. Dental compensation for the Class II skeletal relationship can cause lower incisor protrusion which reduces the dental occlusal discrepancy in comparison to the skeletal discrepancy. Since clinicians aim to obtain a Class I dental relationship by using functional appliances, this dental compensation reduces the activation of the appliance to a level that is required to relieve skeletal discrepancy. For example, when a patient has 10 mm of maxillomandibular skeletal base discrepancy, but because of a lower incisor protrusion, has only 6 mm of anterior overjet, the clinician can only advance the mandible by 4 mm and achieve a normal 2-mm anterior overjet. Considering the functional appliance effect is a mixture of dental and skeletal changes, such patients could only benefit from less than 4 mm of skeletal changes.
To address the problem mentioned above, a treatment plan to remove lower incisor protrusion before or after Class II Twin-block treatment is required in addition to allowing the sufficient advancement of the mandible in order to fully address the skeletal discrepancy. In many cases, lingual uprighting of the lower incisor may require extraction treatment, which is not clinically possible prior to Class II Twin-block treatment. In such cases, lower incisor uprighting after Twin-block treatment should be performed, and during treatment, sufficient skeletal advancement of the mandible is also required, regardless of the dental relationship. This form of Class II functional treatment may result in anterior cross bite, which can be corrected through subsequent fixed appliance treatment. However, this treatment protocol is aggressive and should not be performed without adequate supporting scientific evidence.
The symphysis inclination appeared to be lower in the favorable group than in the unfavorable group, indicating that severe frontal inclination of the mandibular symphysis is associated with the least favorable profile outcomes after Class II Twin-block treatment. The association of the inclination of symphysis with mandibular growth direction has also been reported in a previous study.
15 In that study, metallic implants were used to discriminate the forward mandibular rotator from the backward rotator; cephalometric characteristics were also investigated. In the forward rotating type, the symphysis swung forward in the face and the chin was prominent, while in the backward rotating type, the symphysis swung back and the chin receded. While the precise definition of symphysis inclination measurement in that study differed from that used in the present study (angle between the tangent to the anterior surface of the mandible and the anterior cranial base versus the angle between the mandibular plane and infradentale-pogonion plane), the broad meaning of the two definitions was similar. This indicates that patients with more forward symphysis inclination tend to have a clockwise rotation growth pattern, hindering the projection of the chin point. Mandibular growth acceleration acquired during Twin-block treatment can be expressed in a more vertical direction rather than a sagittal direction, with a smaller advancement of the chin point resulting in a less favorable profile improvement. In addition, the visual effect of a relatively protruded incisal portion, with a relatively retruded chin point, may worsen the retrognathic appearance.
In the present study, smaller measurements of SN to MxP, SN to MnP, and gonial angle were observed in the favorable group. These angle values indicate low divergent skeletal patterns in more favorable soft-tissue profiles after Class II Twin-block treatment. High divergence may indicate backward growth rotation, similar to the protruded symphysis inclination, and mandibular growth can progress in a more downward and backward manner. In previous studies evaluating vertical skeletal pattern and activator appliance effects, increased maxillary-mandibular plane angles with an open bite resulted in further deterioration of the sagittal relationship with an exaggerated open bite.
1617 However, without an open bite, the maxillary-mandibular plane angle did not reduce the overjet in activator treatment. In the present study, while none of the patients had an open bite before treatment, they did not show an aggravation of the Class II relationship and did not fail to achieve a normal Class I anterior overjet and overbite. However, it seems reasonable to assume that increased vertical divergence may not favor treatment outcomes and, consequently, the soft-tissue profile results. Franchi and Baccetti
12 reported similar results in a Class II patient with a pretreatment value of Co-Go-Me degrees greater than 125.5° is expected to respond poorly to treatment including functional jaw orthopedics.
Another feature associated with favorable treatment outcomes in this study was the ANB angle. The group with favorable soft-tissue profile results had a smaller ANB angle before treatment than did the group with unfavorable soft-tissue profile results. A previous study investigating the results of activator treatment found that a larger pre-treatment ANB angle was the only morphologic difference between successfully and unsuccessfully treated patient groups.
18 In addition, another study demonstrated that larger pretreatment ANB angles enable a larger increase in SNB during treatment.
19 While the definition of successful treatment and favorable profile results are different and the study results cannot be directly compared, the results of the present study contradict these previous findings. However, the ANB angle alone may not be an important factor in soft-tissue profile outcomes. It can be affected by vertical skeletal patterns; when the mandibular length remains the same, clockwise rotation increases the ANB angle and
vice versa. Therefore, it would be reasonable to assume that the difference in the ANB angle was a secondary effect of the vertical pattern difference between the groups. Furthermore, logistic regression revealed that the ANB angle is not a highly correlated factor.
In this study, none of the pre-treatment soft-tissue measurements or treatment changes was statistically significantly different between the two groups. This suggests that clinicians cannot accurately judge whether a patient's soft-tissue profile will improve after Class II Twin-block treatment based on facial profile examinations alone. In studies analyzing soft-tissue profile changes after Class II Twin-block treatment, some of the features reported included the retraction of the upper lip, anterior movement of the soft-tissue pogonion, reduction in soft-tissue convexity, and reduction in the H and mentolabial angles.
68 In this study, both the favorable and unfavorable groups showed advancement of the lower lip and soft-tissue pogonion after treatment; however, the difference was not statistically significant which may be due to the small sample size. Esthetic judgment may be more dependent on total facial balance rather than regional changes, and the favorable group in this study may have had the best total facial balance. More statistically significant treatment changes in the hard-tissue B point and pogonion were observed in the favorable group compared to the unfavorable group; however, the corresponding soft-tissue changes were not statistically different. This may indicate that the soft-tissue response is not fully synchronized with the underlying hard tissue. A study evaluating the soft-tissue changes after Twin-block and mini-block appliance treatment reported a wide range of responses and concluded that a simple hard-tissue to soft-tissue change ratio may not be ideal.
20 In addition, the measurement method itself may be inappropriate because, while growth may occur in both the vertical and sagittal directions, only the sagittal direction was measured.
An increase in the gonial angle after Class II Twinblock treatment in the favorable group (mean = 2.17°) was observed, while only a relatively small increase (0.55°) was observed in the unfavorable group. Furthermore, considering that the angular measurement error was between 0.54° and 1.21°, the angular change in the unfavorable group was negligible. Several studies have reported an increase in the gonial angle after treatment with Twin-block or other functional appliances.
212223 Nelson et al.
22 observed an increase in the gonial angle after treatment with a Harvold appliance and concluded that this was due to articular shifting posteriorly rather than menton or gonion changes. Sharma et al.
23 also reported an increase in the gonial angle following Class II Twin-block treatment and discussed that this phenomenon may be the result of changing muscle functions or due to sagittally directing condylar growth, leading to greater increments in total mandibular length. According to these authors, the increase in the gonial angle after Class II Twin-block treatment is a positive indication of mandibular morphogenetic change, resulting in an improved jaw relation. This could be one of the reasons for the improvement in soft-tissue profile outcomes in the favorable group reported in the present study; however, further research is required to elucidate the precise mechanism.
In a randomized clinical trial (RCT) comparing patients with Class II division 1 malocclusion receiving early treatment with Twin-block and fixed appliances, treatment with the fixed appliance only showed no difference in the cephalometric skeletal pattern over 10 years of post-treatment follow-up.
24 The authors concluded that early treatment for Class II malocclusion is unjustified. It is uncertain whether a lack of difference in skeletal pattern corresponds to a lack of difference in soft-tissue profile; it is also unclear if the profile improvements recorded in the patients of the present study were maintained until the completion of facial growth. As previously discussed, the profile results in this study varied among patients receiving Class II Twin-block treatment, and it appears that some skeletal patterns may be more responsive to treatment. The Angle classification of the sagittal relationship is not complex enough to characterize the skeletal patterns, and it is generally accepted that not all patients with Class II malocclusion are the same. A previous RCT
20 specified a 7-mm overjet as a patient inclusion criteria; this appears to be too simple. The patient sample used in that study could have comprised a mixture of unfavorable and favorable Class II patients which may have resulted in a zero-sum average which was not statistically significantly different from non-functional appliance-treated Class II patients. Classification and analysis of Class II skeletal patterns needs to be more detailed and sophisticated to differentiate patients with Class II malocclusion in the view of the potential benefits of a functional appliance.
It would have been unnecessary for patients in the favorable group to receive second phase orthodontic treatment using a fixed appliance unless they had dental alignment problems. These patients could benefit from Class II Twin-block treatment, avoiding the need for fixed appliances. While early treatment using a Class II Twin-block appliance can be justified in these patients, for patients in the unfavorable group, second-phase orthodontic treatment and extraction treatment are more likely to be required. According to the RCT mentioned above, early treatment with a Twin-block appliance and subsequent treatment with a fixed appliance did not result in any improvements, compared with the treatment using a fixed appliance alone.
23 Therefore, if fixed-appliance treatment seems inevitable, initial Twin-block application may not be justified. Consequently, when patients are expected to have an unfavorable profile after Twin-block treatment, the application of a Twin-block appliance is not recommended; however, further studies with long-term follow-up profiles are required to confirm this finding.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download