Dear Editor,
The presentation of multiple cranial-nerve palsies is a common clinical scenario in neurological practice. The lesion can be localized anatomically based on the pattern of cranial-nerve involvement. We report a rather rare presentation of a rare disorder with the same manifestations.
A 52-year-old diabetic male presented with the subacute onset of severe holocranial and throbbing headache with a 2-month history. This was associated with vomiting and mild fever lasting 1 week. One week later he developed tinnitus, vertigo, and bilateral sequential severe sensorineural hearing loss associated with bilateral palsy of the lower motor neuron 7th nerve (left>right). There was no history of seizures, focal neurological deficits, joint pains, oral ulcers, or loss of weight or appetite. A physical examination did not reveal any contributory factors, with the exception of mild icterus, involvement of the 7th and 8th cranial nerves, and swaying while walking that was attributed to vestibular dysfunction. Puretone audiometry confirmed the presence of bilaterally severe sensorineural hearing loss with a bilateral type A tympanogram on impedance audiometry. The blink test was not performed.
The differential diagnosis included chronic meningitis, hypertrophic pachymeningitis, noninfectious granulomatous diseases, carcinomatous meningitis, and CNS vasculitis.
The patient was evaluated at another hospital, where brain contrast-enhanced MRI was performed, which produced normal findings. A CSF analysis revealed 16 cells (all lymphocytes) and normal protein and sugar levels. Brain contrast-enhanced MRI and CSF analysis including of malignant cells at our hospital produced findings within normal limits. The patient had already received intravenous steroids at another hospital, which resolved the headache and vomiting and could explain the absence of cerebral/brainstem lesions on brain MRI and the acellular CSF. Serum angiotensin converting enzyme, antinuclear antibody, and anti neutrophilic cytoplasmic antibody levels were also normal.
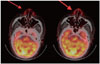
FDG-PET was performed to rule out granulomatous inflammation/malignancy. This revealed increased uptake in the nasal cartilage and right aural cartilage and non-FDG-avid thickening of the left earlobe (Fig. 1). Splenic infarcts were also noted in the lateral aspect of the spleen.
A review found that he had a significant 3-year history of recurrent episodes of painful bilateral external-ear swelling and redness that occurred every year, lasted for 1 week, and was responsive to IV Non-steroidal antiinflammatory drugs. He also had a 30-year history of jaundice. A workup for hemolytic jaundice revealed hereditary spherocytosis as the cause: paroxysmal nocturnal hemoglobinuria mutation, G6PD, and direct Coombs test were negative, and a peripheral blood film revealed spherocytosis with a positive osmotic fragility test.
Based on his clinical presentation (7th and 8th nerve involvement) with evidence of nasal and auricular chondritis on the FDG-PET scan, our patient fulfilled McAdam's diagnostic criteria for relapsing polychondritis.1 In view of the splenic infarct, the possibility of secondary vasculitis was also entertained, and he was started on methylprednisolone and intravenous pulse cyclophosphamide in consultation with a rheumatologist. This intervention produced significant improvements in hearing and facial asymmetry.
Relapsing polychondritis is a rare disease affecting the cartilaginous and proteoglycan-rich structures.2 Neurological manifestations occur in about 3% of patients with relapsing polychondritis and is related to vasculitis of the peripheral nervous system or CNS. The various neurological manifestations include headache, cranial neuropathies, seizures, hemiplegia, aseptic meningitis, and meningoencephalitis. Optic neuropathy is the most-common cranial neuropathy, followed by involvement of the 5th and 7th cranial nerves. Sensorineural deafness is related to vasculitis in the vestibular or cochlear branch of the internal auditory artery. Only a handful of reported cases of relapsing polychondritis have presented as multiple cranial-nerve palsies.34 Vasculitis associated with relapsing polychondritis can involve vessels of any size, being described variously as small-, medium-, and large-vessel vasculitis, and splenic infarction may be a manifestation of medium-vessel vasculitis.5 In the light of the other disease activity, vasculitis due to relapsing polychondritis seemed more likely in the present patient. However, it was impossible to exclude splenic infarction resulting from hereditary spherocytosis in this patient.
Treatment involves the administration of NSAIDs for auricular/ nasal chondritis and immunosuppressive therapy in cases of organ involvement. FDG-PET may be a powerful tool for diagnosing and managing relapsing polychondritis, and can be used to delineate the extent of inflammation in the body and also is useful for targeting biopsy sites.6
To conclude, although rare, relapsing polychondritis can present as headache and multiple cranial-nerve palsies, and it should be considered in the differential diagnosis of multiple cranial-nerve palsies in an appropriate setting.
Figures and Tables
References
1. Vitale A, Sota J, Rigante D, Lopalco G, Molinaro F, Messina M, et al. Relapsing polychondritis: an update on pathogenesis, clinical features, diagnostic tools, and therapeutic perspectives. Curr Rheumatol Rep. 2016; 18:3.

2. Sharma A, Law AD, Bambery P, Sagar V, Wanchu A, Dhir V, et al. Relapsing polychondritis: clinical presentations, disease activity and outcomes. Orphanet J Rare Dis. 2014; 9:198.

3. Ismail FS, Enzi B, Boy C, Kowoll A, Eyding J, Schlegel U. Relapsing polychondritis as an unusual cause of multiple cranial nerve palsies-a case report. Muscle Nerve. 2017; 56:E3–E4.

4. Ushiyama S, Kinoshita T, Shimojima Y, Ohashi N, Kishida D, Miyazaki D, et al. Hypertrophic pachymeningitis as an early manifestation of relapsing polychondritis: case report and review of the literature. Case Rep Neurol. 2016; 8:211–217.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download