Dear Editor,
Optic neuritis can develop in patients with Behçet's disease in rare cases.1 However, the association between optic neuritis and Behçet's disease has not yet been elucidated, and inflammatory eye diseases such as uveitis and retinal vasculitis can develop in the early stage of Behçet's disease.2 Therefore, the diagnosis of optic neuritis as a manifestation of neuro-Behçet's disease should be carefully considered.
A 64-year-old woman presented with the left visual disturbance that had developed 10 days previously. She had been diagnosed with left optic neuritis both 14 months and 6 months previously, and had received high-dose IV steroid and oral steroid-tapering therapies. Her left visual acuity deteriorated suddenly, and this was accompanied by headache and eyeball pain on the left side. The symptoms responded well to IV steroid treatment. However, the left visual disturbance recurred after steroid discontinuation. Her Behçet's disease had been treated with oral steroids for 3 years, and she had no other specific medical or family history.
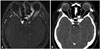
A funduscopic examination and extraocular movement test produced no specific abnormal findings, which had also been the case after the two previous attacks. Left central scotoma in a visual field test and left color blindness in a color vision test were observed whenever sudden visual deterioration occurred, including in the index attack. Her corrected visual acuity was 0.1 on the left and 0.7 on the right. The color vision test produced normal findings on the right and tritanopia on the left (score of 0/15). Her central scotoma and color blindness were improved after treatment with high-dose IV steroid. No defect in the retinal nerve fiber layer was observed in optical coherence tomography (OCT). The full-field visual evoked potential exhibited poor wave formation and prolonged latency of the P100 wave on the left side. Orbit MRI including a fat-suppression T1-weighted gadolinium-enhancement sequence performed both at the second and index attacks did not reveal any signal change or enhancement in the optic nerves or brain parenchyme. Chronic nonspecific sinusitis was observed in the left posterior ethmoid and sphenoid sinuses (Fig. 1).
Standard blood tests and serologic tests including anti-aquaporin-4 antibody, antinuclear antibody, anti-double-stranded DNA antibody, antineutrophil cytoplasmic antibody, lupus anticoagulant, anticardiolipin antibody, and antiphospholipid antibody produced normal findings. HIV and syphilis screening tests were also negative. The findings for angiotensin-converting enzyme, thyroid function tests, and protein and immune electrophoresis were also normal. A cerebrospinal fluid examination produced normal results, and the oligoclonal band was absent.
The patient had been treated with high-dose IV steroid in the acute stage of visual deterioration, and oral steroid and azathioprine for the prevention of neurologic complications after the tentative diagnosis of recurrent optic neuritis associated with neuro-Behçet's disease. However, we doubted this diagnosis because her visual acuity had deteriorated only on the left side whenever the administered steroid was discontinued, and there was no straightforward evidence of optic neuritis in funduscopy, OCT, or orbit MRI.
A surgical exploration was performed for left posterior ethmoidal and sphenoidal sinusitis. A fungal ball was observed and removed. Fungal hyphae were observed in Grocott's methenamine silver and periodic aicd-Schiff staining, and numerous degenerative fungal hyphae suggestive of Aspergillus species were observed in an excisional biopsy sample from the left sphenoid sinus. After surgical treatment her visual acuity gradually recovered, and the headache and eyeball pain on the left side were resolved.
Here we have described a case presenting as unilateral optic neuropathy associated with ipsilateral chronic posterior ethmoidal and sphenoidal sinusitis. The visual disturbance of the patient did not result from the recurrent optic neuritis associated with neuro-Behçet's disease. Her visual disturbance has recurred only on the left side, and funduscopy, OCT, and orbit MRI produced no evidence of optic neuritis. Optic neuropathy can occur due to compression of the canalicular portion of the optic nerve around the posterior ethmoidal and sphenoidal sinusitis.3 The present case exhibited a good response to IV steroid therapy, which may have been due to reduced edema of the compressed optic nerve. Optic neuropathy associated with invasive aspergillus infection has been reported only rarely in immunocompetent patients.45
Optic neuritis has recently become an important manifestation of various autoimmune CNS diseases, including multiple sclerosis, neuromyelitis optica, and even neuro-Behçet's disease. However, as in the present case, if visual acuity deteriorates repeatedly on one side and there is insufficient evidence of optic neuritis, other ophthalmologic and optic nerve conditions must be considered.
Figures and Tables
Fig. 1
Fat-suppression T1-weighted gadolinium-enhanced orbit MRI and contrast-enhanced paranasal sinus CT in the patient. A: Fat-suppression T1-weighted gadolinium-enhanced orbit MRI does not reveal any signal change or enhancement in the bilateral optic nerves. Chronic nonspecific sinusitis was evident in the left posterior ethmoid and sphenoid sinuses (white arrow). The high signal intensity in the left orbit was due to a metallic artifact of the subject's denture (black arrow). B: Contrast-enhanced paranasal sinus CT revealed no specific abnormal density change or lesion in the bilateral orbits or optic nerves. Chronic nonspecific sinusitis was evident in the left posterior ethmoid and sphenoid sinuses (white arrow).
References
2. Khairallah M, Ben Yahia S, Kahloun R, Khairallah-Ksiaa I, Messaoud R. [The eye and Behçet's disease]. J Fr Ophtalmol. 2012; 35:826–837.
3. Rimmer J, Beale T, Lund VJ. Visual loss in patients with sphenoethmoidal cells. J Laryngol Otol. 2015; 129:198–201.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download