This article has been
cited by other articles in ScienceCentral.
Dear Editor:
Tinea incognito (TI) is a fungal infection that lost its characteristic clinical manifestation due to improper use of topical steroids. Few studies were reported until Kim et al.
1 published a 9-year multi-center study of TI in Korea. It stated that TI predominantly demonstrated eczema-like manifestation (82.0%) and that folliculitis-like presentation was exceptionally rare (0.7%). Therefore, the present study investigated this rare type of TI to aid diagnosis and management.
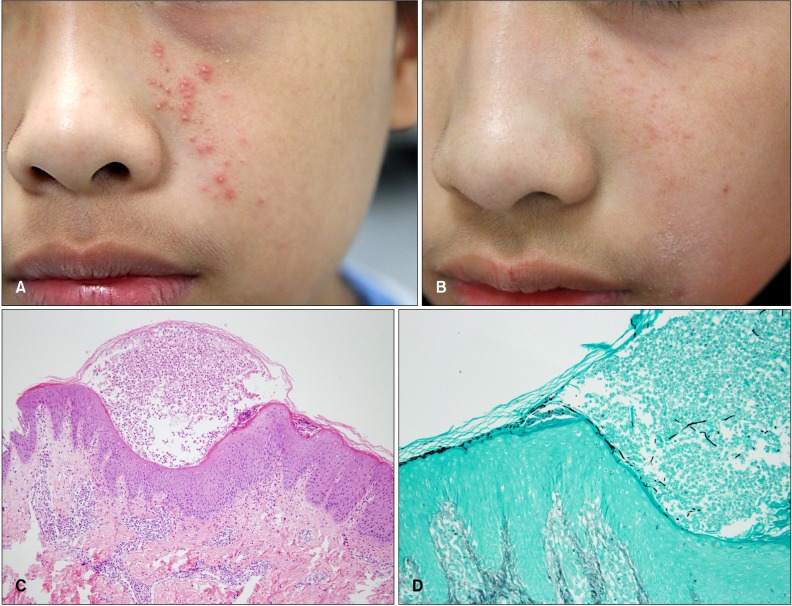
The present study is a case series of 5 TI patients with folliculitis-like presentation. Cases were excluded in which anti-fungal treatment was effective but fungal infection was not confirmed. Their data are summarized in
Table 1. Clinical manifestation included erythematous papules or pustules without scaly annular patches (
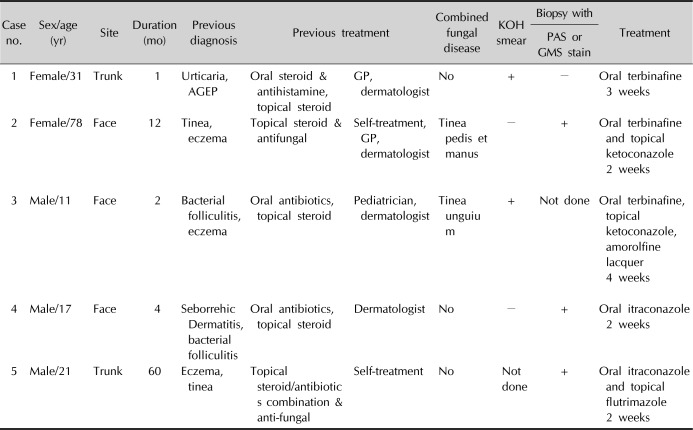
Fig. 1A, B). Two showed TI limited to the sites where a radiofrequency cosmetic procedure was performed (trunk, patient 1) or places sealed by headphones (ears, patient 4). Histopathologic examination revealed pustules with neutrophils and superficial inflammatory cell infiltration. Special staining demonstrated fungal hyphae and spores (
Fig. 1C, D). Treatment with oral anti-fungal agents with or without topical anti-fungal products was successful in all the patients. Long-term follow-up was available in three patients (4, 8, and 12 months), and TI did not recur.
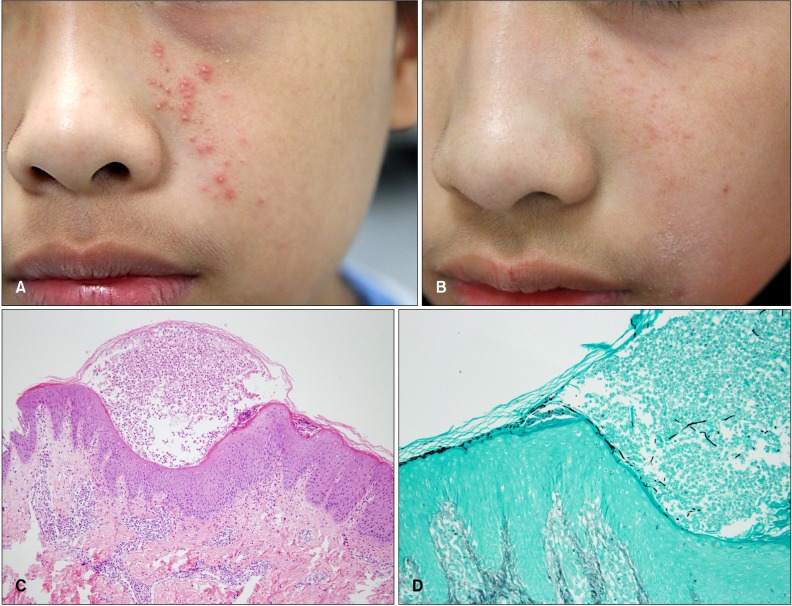 | Fig. 1Tinea incognito with folliculitis-like presentation. (A) Before treatment. (B) Complete resolution of skin lesions after 4 weeks of oral terbinafine. (C) Intracorneal pustules and superficial perivascular superficial perivascular lymphohistiocytic, eosinophilic and neutrophilic infiltration (H&E, ×100). (D) Fungal hyphae and spores (Gomori methenamine silver, ×200).
|
Table 1
Characteristics of patients
|
Case no. |
Sex/age (yr) |
Site |
Duration (mo) |
Previous diagnosis |
Previous treatment |
Combined fungal disease |
KOH smear |
Biopsy with |
Treatment |
|
PAS or GMS stain |
|
1 |
Female/31 |
Trunk |
1 |
Urticaria, AGEP |
Oral steroid & antihistamine, topical steroid |
GP, dermatologist |
No |
+ |
− |
Oral terbinafine 3 weeks |
|
2 |
Female/78 |
Face |
12 |
Tinea, eczema |
Topical steroid & antifungal |
Self-treatment, GP, dermatologist |
Tinea pedis et manus |
− |
+ |
Oral terbinafine and topical ketoconazole 2 weeks |
|
3 |
Male/11 |
Face |
2 |
Bacterial folliculitis, eczema |
Oral antibiotics, topical steroid |
Pediatrician, dermatologist |
Tinea unguium |
+ |
Not done |
Oral terbinafine, topical ketoconazole, amorolfine lacquer 4 weeks |
|
4 |
Male/17 |
Face |
4 |
Seborrehic Dermatitis, bacterial folliculitis |
Oral antibiotics, topical steroid |
Dermatologist |
No |
− |
+ |
Oral itraconazole 2 weeks |
|
5 |
Male/21 |
Trunk |
60 |
Eczema, tinea |
Topical steroid/antibiotics combination & anti-fungal |
Self-treatment |
No |
Not done |
+ |
Oral itraconazole and topical flutrimazole 2 weeks |

TI has been increasing in recent years
1. It is particularly problematic in Korea, where patients can buy a potent topical steroid agent with ease as an over-the-counter drug. In addition, individuals can easily acquire a prescription for steroids from non-dermatologists with relatively high medical accessibility. In the present study, the majority of the cases were initially managed by non-dermatologists or self-treatment was administered with improper use of steroids. However, one case was treated by a dermatologist, which indicates the difficulty of diagnosing this fungal infection. Great imitators in dermatology generally include syphilis, fungal infection, and scabies, which are easily misdiagnosed
2. Topical anti-fungal agents had already been tried in two patients, which was unsuccessful. TI which acquired higher pathogenicity should be treated with oral agents
3. Both oral terbinafine and itraconazole for several weeks were effective in the present study. When TI is suspected, KOH smear and biopsy with special staining should be performed to make an accurate diagnosis and ensure the correct treatment strategy. Histopathological examination can also provide clues of the fungal infection, such as a variable host inflammatory response and neutrophils in the epidermis or horny layer
4. Risk factors for TI included long-lasting erythematous scaly lesions, no response to steroid or calcineurin inhibitor treatment, face or trunk lesion, combined tinea pedis/unguium, and immunosuppression
1. TI does not have the typical characteristics of fungal infection and can mimic other cutaneous diseases, including lupus erythematosus, psoriasis, eczema, and folliculitis
15. Therefore, thorough history taking and physical examination is required to suspect TI and to perform adequate tests.
Trichophyton rubrum was the most common causative pathogen (73.1%) irrespective of the sites, followed by
Trichophyton mentagrophyte (9.0%) in Korea
1. Unfortunately, fungus culture was not performed in the present study.
Clinicians should be familiar with this condition and patients should not self-administer potent steroids.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download