Dear Editor:
Hypopigmented mycosis fungoides (HMF) is an atypical, rare clinical variant of MF characterized by hypopigmented to achromic patches alone or, more commonly, in combination with studding erythematous papules or plaques. The epidemiologic features that distinguish HMF from classical MF are related to its high prevalence among younger patients, such as children and adolescence, as well as patients with high skin phototypes (usually Fitzpatrick skin scale IV~V)1. Psoralen plus ultraviolet A (PUVA) was the main treatment used in the previously reported literature2. Reports on narrowband UVB (NBUVB) phototherapy have recently demonstrated this therapy to be a successful alternative for PUVA therapy3.
A 10-year-old Korean boy presented to Pusan National University Hospital for evaluation of asymptomatic hypopigmented patches of skin and studded erythematous papules on the left upper back and flank (Fig. 1A). Wood light examination did not show pronounced attenuation. The histopathology results were compatible with MF. The microscopic description revealed epidermotrophism of haloed atypical lymphocytes (Fig. 1B). Additional studies on the rearrangement of the T cell receptor gamma gene showed monoclonality (Fig. 2). Considering limited lesional distribution in this patient and higher effectiveness of excimer laser than local NBUVB in focal vitiligo, we chose and performed 308 nm excimer laser therapy once a week for the diagnosis of HMF (stage IA). This treatment resulted in the clearance of the lesions and repigmentation of the hypopigmented areas after about 1 year (Fig. 1C). The mean fluence emitted was 340 mJ/cm2, and the total cumulative dose was 17.7 J/cm2.
The prognosis for HMF is usually good compared with that for classical MF. Infiltrative atypical CD8+ cells are postulated to play a role in preventing the usual patch stage disease from progressing to advanced plaque and tumour stages1. Also, the cytotoxic effect of CD8+ T lymphocytes are believed to influence melanocyte stability and melanogenesis resulting in hypopigmented patches clinically. In respect to treatment, HMF recurs frequently, even if there is a long period of complete remission. Although there were some reports of 308 nm excimer use for patch or plaque stages of MF4, there has been no report of 308 nm excimer for HMF. 308 nm excimer laser has the advantage of avoiding unnecessary ultraviolet radiation exposure to unaffected sites over NBUVB phototherapy, therefore it is widely used alone or with other treatment modality5. According to a previous report4 of a 308 nm excimer laser treatment for classic MF, the mean fluence of 417.5 mJ/cm2 with a total cumulative dose of 9.15 J/cm2 were needed to clear the lesion. These doses were similar doses to those used in our case, indicating that the approximate dose of 400 mJ/cm2 as the mean fluence might be the optimal parameter for use in a future larger trial. Although a larger comparative randomized trial is needed, we hypothesize that the 308 nm excimer laser could be a good option for the treatment of HMF with a limited distribution, similar to the present case.
Figures and Tables
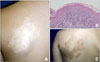 | Fig. 1Hypopigmented mycosis fungoides (HMF). (A) Hypopigmented patch studded with erythematous papules on his left upper back in a 10-year-old boy. (B) Epidermotrophism of haloed atypical lymphocytes (H&E, ×200). (C) Improvement of HMF with hyperpigmentation after about 1 year of 308 nm excimer laser therapy performed once a week. |
References
1. Furlan FC, Sanches JA. Hypopigmented mycosis fungoides: a review of its clinical features and pathophysiology. An Bras Dermatol. 2013; 88:954–960.

2. Wongpraparut C, Setabutra P. Phototherapy for hypopigmented mycosis fungoides in Asians. Photodermatol Photoimmunol Photomed. 2012; 28:181–186.

3. Kanokrungsee S, Rajatanavin N, Rutnin S, Vachiramon V. Efficacy of narrowband ultraviolet B twice weekly for hypopigmented mycosis fungoides in Asians. Clin Exp Dermatol. 2012; 37:149–152.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download