Abstract
Several dermatoses have been reported in association with Becker's nevus. Eczematous dermatitis associated with Becker's nevus is extremely rare, described in only two previous case reports. We report a case of 21-year-old male with recurrent eczema lesions which were always localized within the underlying Becker's nevus lesion. This case may be explained as a Wolf's isotopic response-like phenomenon.
Becker's nevus is a unilateral, hyperpigmented, hypertrichotic organoid cutaneous hamartoma. Lesions are usually asymptomatic and rarely associated with several dermatoses and structural abnormalities. Skin diseases such as acneiform lesions1, lichen planus2, prurigo nodularis3, hypohidrosis4, lymphomatoid papulosis5, desmoid tumor6, localized scleroderma, leiomyoma cutis, and plexiform neurofibroma7 have been reported in association with Becker's nevus. Structural abnormalities associated with Becker's nevus include breast hypoplasia, supernumerary nipples, aplasia of the pectoralis major muscle, ipsilateral limb shorting, segmental odontomaxillary dysplasia, and lipoatrophy37. Eczematous dermatitis associated with Becker's nevus is rarely reported, described in only two previous case reports38.
A 21-year-old healthy male presented with pruritic erythematous papules overlying a hyperpigmented, hypertrichotic patch on his right upper back (Fig. 1A, B). Underlying hyperpigmented lesion had been prominent since around puberty and remained asymptomatic until 3 years ago when eczematous pruritic lesions intermittently developed on it. During the first episode, 3 years ago, he came to our office and was prescribed with topical corticosteroid (Fig. 1C). After applying topical ointment for 1 month, pruritic lesions were improved (Fig. 1D). Then he was lost to follow-up, and 3 years later he visited our office again with a similar complaint. He said that pruritic lesions recurred intermittently during follow-up loss period and the lesions were always localized to underlying hyperpigmented patch on each occasion. He controlled them himself with topical corticosteroid whenever they occurred. He had atopic dermatitis as a child.
Physical examination revealed excoriated pruritic papules confined to an underlying well-demarcated, irregularly shaped hyperpigmented patch on his right upper back (Fig. 1A, B). There were no eczema lesions elsewhere. A 4-mm punch biopsy from a pruritic papule demonstrated increased basal pigmentation and a moderate superficial perivascular inflammatory infiltrate with lymphocytes and eosinophils (Fig. 2A~C). In dermis, smooth muscle bundles were irregularly placed without association with hair follicles (Fig. 2D). There was a focal sub-epidermal bleb; however, autoimmune blistering diseases were excluded by a negative direct immunofluorescence test. Histologic findings were consistent with eczematous dermatitis coexisting with Becker's nevus. Based on the clinical and pathologic findings, diagnosis was made as Becker's nevus with eczema limited to the nevus lesion. He was prescribed topical desoxymethasone 0.25% ointment to be applied twice daily. After one month of treatment, pruritic lesions almost cleared (Fig. 3).
Various skin and structural abnormalities have been associated with Becker's nevus and there are plausible explanations about their association. An increase in androgen receptors in Becker's nevus may contribute to the occurrence of acneiform eruption and breast hypoplasia17. Hypohidrosis co-localized with Becker's nevus is considered to be related to genetic mutation or mosaicism4. Eczematous dermatitis associated with Becker's nevus has been described in two previous case reports38. As in the previous reports, eczema lesions were confined to the nevus lesion in the present case. Interestingly, the eczema lesions were improved by topical treatment and then recurred always localized to the nevus lesion on each occasion. This case demonstrates more solid evidence of the association between the two diseases.
The fact that pruritic lesions were recurrent and always localized to the hyperpigmented patch suggests that co-existence of these two diseases is more than a mere coincidence. Wolf's isotopic response, which is the occurrence of a new unrelated disease at the same location as previously healed disease9, may explain our case. Since underlying Becker's nevus lesion continues to exist, our case is not exactly consistent with the definition of Wolf's isotopic response. Nevertheless, our case is associated with Wolf's isotopic response in that two unrelated diseases occurred at the same location. Therefore we suggest calling our case as a Wolf's isotopic response-like phenomenon.
The precise patho-mechanism of Wolf's isotopic response is still unknown. Various hypotheses have been proposed to explain the phenomenon, and there are 4 most representative theories: viral hypothesis, vascular hypothesis, immunologic hypothesis, and neural hypothesis10. Viral hypothesis is derived from cases where new skin lesions developed on the previously healed herpetic virus infected lesion, suggesting that neurovascular alteration by virus creates a vulnerable environment for new skin disease development11. Vascular hypothesis suggests that the local microcirculatory damage after inflammation makes the area vulnerable to damage and localized inflammation upon future insult12. Immunologic hypothesis proposes that initial skin disease modifies the regional immune system or causes formation of memory T cells and these immunologic changes make the area vulnerable to new skin disease10. Neural hypothesis suggests that local inflammation made by initial skin disease destroys nerve fibers, and the destroyed nerves release various neuropeptides and neurotransmitters which cause abnormal local immune response to second attack1013. Conversely, immune cells express more cell membrane receptors for various neural secretions after first dermatosis, so neural activation can be exaggerated upon the same secretions10. Since none of the above hypotheses can solely explain the phenomenon of isotopic response, these factors probably work in concert to cause the second skin disease. However, this case is different in that Becker's nevus is not an inflammatory dermatosis but a persistent hamartomatous condition resistant to treatment. Although pathogenesis of Becker's nevus is still unclear, we suggest that a certain unusual environment within the nevus makes the area more vulnerable to new skin disease in line with Wolf's isotopic response, especially in view of the fact that this patient's skin barrier and immune system is abnormal or skewed by his atopic athesis.
Figures and Tables
 | Fig. 1(A) Pruritic erythematous papules confined to underlying hyperpigmented, hypertrichotic patch on the right upper back. (B) Close-up view. (C) The first episode of occurrence of pruritic papules overlying hyperpigmented patch. (D) Improved lesions after one month of treatment. |
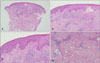 | Fig. 2(A) Biopsy from a pruritic papule (H&E, ×40). (B) A focal sub-epidermal bleb with superficial perivascular inflammatory infiltration (H&E, ×100). (C) Increased basal pigmentation and a moderate superficial perivascular inflammatory infiltrate with lymphocytes and eosinophils (H&E, ×200). (D) Irregulary placed smooth muscle bundles which are not associated with hair follicles in the dermis (H&E, ×100). |
References
1. Santos-Juanes J, Galache C, Curto JR, Carrasco MP, Ribas A, Sánchez del Río J. Acneiform lesions in Becker's nevus and breast hypoplasia. Int J Dermatol. 2002; 41:699–700.

2. Terheyden P, Hornschuh B, Karl S, Becker JC, Bröcker EB. Lichen planus associated with Becker's nevus. J Am Acad Dermatol. 1998; 38:770–772.

3. Lockshin BN, Brogan B, Billings S. Eczematous dermatitis and prurigo nodularis confined to a Becker's nevus. Int J Dermatol. 2006; 45:1465–1466.

4. Do JE, Kim YJ, Kang HY. Hypohidrosis colocalized with Becker's naevus. Br J Dermatol. 2007; 156:766–767.

5. Buder K, Wendel AM, Cerroni L, Goebeler M, Kerstan A. A case of lymphomatoid papulosis limited to Becker's melanosis. Dermatology. 2013; 226:124–127.

6. Sciallis GF, Sciallis AP. Becker nevus with an underlying desmoid tumor: a case report and review including Mayo Clinic's experience. Arch Dermatol. 2010; 146:1408–1412.
7. Glinick SE, Alper JC, Bogaars H, Brown JA. Becker's melanosis: associated abnormalities. J Am Acad Dermatol. 1983; 9:509–514.

8. Lee DJ, Kang HY. Eczema confined to Becker's nevus on the face: the behavior of melanocytes during inflammation. Ann Dermatol. 2012; 24:99–100.

9. Wolf R, Wolf D, Ruocco E, Brunetti G, Ruocco V. Wolf's isotopic response. Clin Dermatol. 2011; 29:237–240.

10. Mahajan R, De D, Saikia UN. Wolf's isotopic response: report of a case and review of literature. Indian J Dermatol. 2014; 59:275–282.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download