MATERIALS AND METHODS
Patients
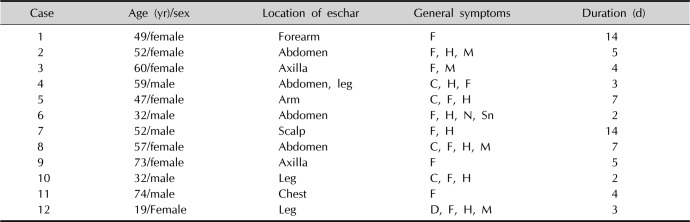
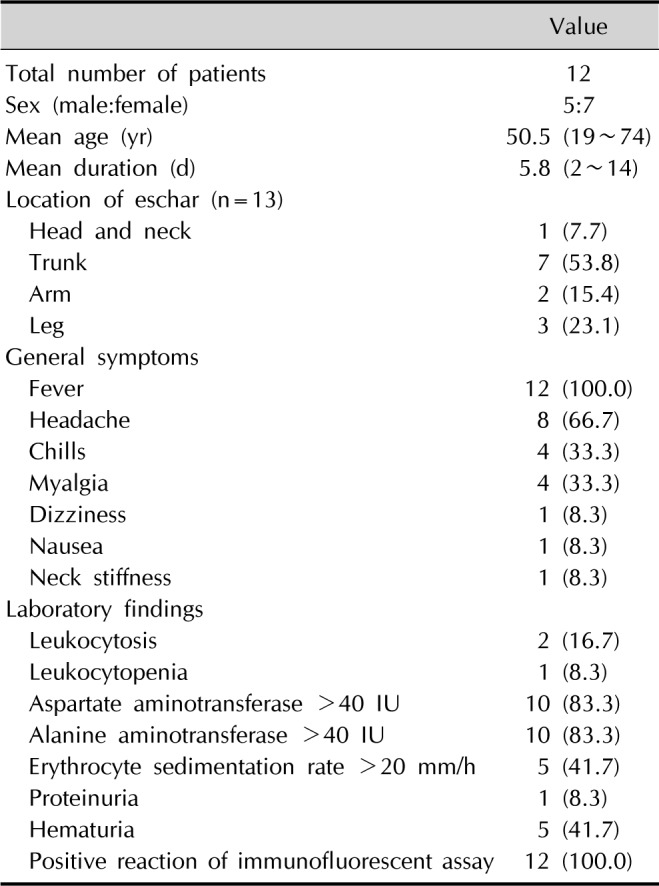
Twelve patients diagnosed with tsutsugamushi disease who visited Kosin University Gospel Hospital over the span of 5 years were evaluated. Diagnosis of tsutsugamushi disease was based on present illness, clinical manifestations including eschar and general symptoms, histopathologic findings, and serology results such as indirect immunofluorescent assay specific to O. tsutsugamushi.
Histopathological and immunohistochemical evaluations
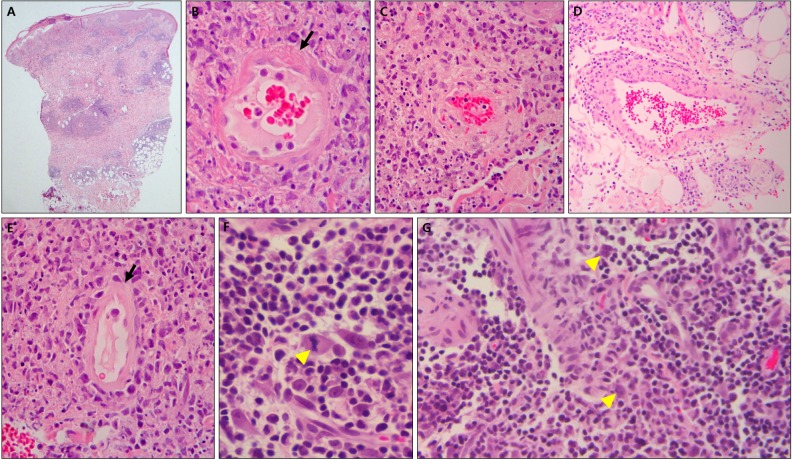
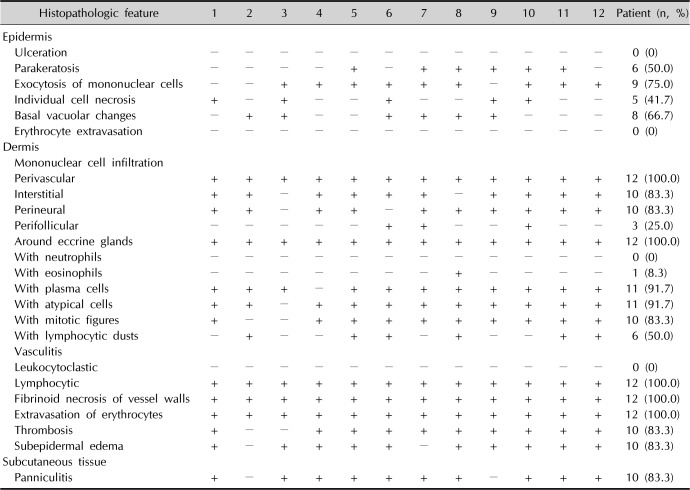
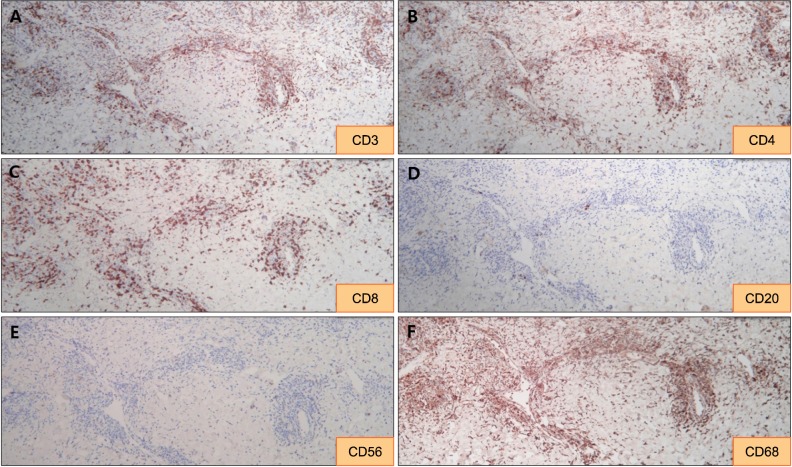
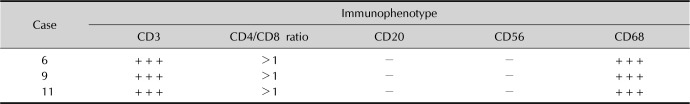
A 4 mm punch biopsy was performed within 1 cm from the eschar in perieschar erythematous area. Epidermal ulcerations, parakeratosis, mononuclear cell exocytosis, individual cell necrosis, basal vacuolar changes, erythrocyte extravasation, dermal mononuclear cell infiltration (including type of infiltrated cell, infiltration site, and presence of mitotic figures), leukocytoclastic vasculitis, lymphocytic vasculitis, fibrinoid necrosis of vessel walls, thrombosis, subepidermal edema, and subcutaneous tissue panniculitis were observed in H&E-stained slides of the samples. Additionally, for tissue slices embedded in paraffin, immunohistochemical staining was performed using monoclonal antibodies for CD3, CD4, CD8, CD20, CD56, and CD68. The presence of staining for each antibody was noted, and the CD4/CD8 ratio was calculated.
Go to :

DISCUSSION
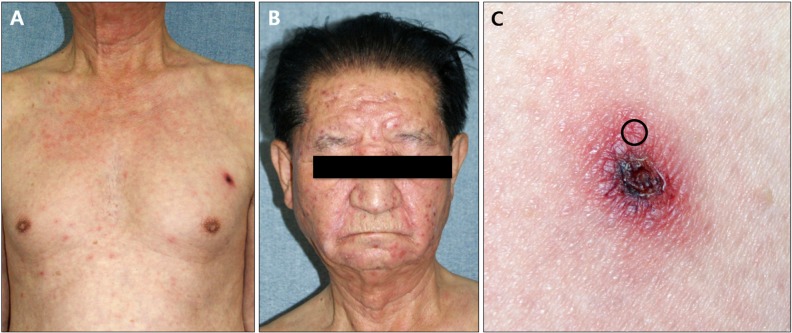
Scrub typhus, also known as tsutsugamushi disease, is an infectious disease caused by
O. tsutsugamushi, a parasite within the cells of mites. Scrub typhus is passed through bites of trombiculid mites, which belong to the Trombiculidae family. Following bites from trombiculid mites, an eschar and a systemic, asymptomatic rash appear. In most cases, the eschar does not have subjective symptoms, and it varies in frequency from 55% to 82%. The most common areas of eschar onset include the armpit, buttocks, narrow parts, and sites typically covered by underwear. Anemia, leukocytosis, leukocytopenia, thrombocytopenia, and hypoalbuminemia are present in some cases. A South Korean study reported that tsutsugamushi disease was accompanied by increased S-GOT and S-GPT in approximately 80% of cases
3.
Allen and Spitz
4 reported that in biopsies of eschar areas, acanthosis, cellular swelling, and necrosis were found in the epidermis. Compact infiltration of monocytes consisting of lymphocytes, plasma cells, mast cells, histiocytes, and Reed-Sternberg cells was observed around sweat glands, hair follicles, sebaceous glands, nerves, and blood vessels in the dermis. They also noted that collagen denaturation similar to coagulative changes accompanying other insect bites are sometimes present along with vasodilation, acute thrombophlebitis, and arteritis. Chaudhary et al.
2 reported that in biopsies of the eschar areas, keratinocyte necrosis, basal vacuolar degeneration, and red blood cell (RBC) entrapment were observed in the epidermis in approximately 20% of cases. In the dermis, leukocytoclastic vasculitis, neutrophil infiltration, and RBC extravasation were observed in 93.3%, 86.7%, and 93.3% of cases, respectively, but lymphocytic vasculitis was observed only in 6.7% of the cases. In addition, vascular wall necrosis, swelling of vascular endothelial cells and thrombosis have reportedly been observed. Vasculitis in tsutsugamushi disease is currently thought to be caused by either destruction of endothelial cells in small vessels or an inflammatory response caused by leukocytes
5. In this study, the histopathological findings of lesions around the eschar included lymphocytic vasculitis and infiltration of atypical lymphohistiocytes around blood vessels, sweat glands, hair follicles, sebaceous glands, and nerves. Leukocytoclastic vasculitis and neutrophil infiltration were not present, but atypical cell infiltration, mitotic figures, vascular wall necrosis, and thrombosis were observed in this study.
In leukocytoclastic vasculitis, circulating immune complexes are deposited on the vascular wall, the complement system is activated, and various inflammatory mediators are isolated to destroy endothelial cells
6. Hypercoagulability was found in 53% of patients with an ulcer caused by leukocytoclastic vasculitis
7. In addition, in the case of ulcers caused by a local injury, leukocytoclastic vasculitis is often found on histopathological examination. For such cases of vasculitis, it is important to consider the possibility of secondary phenomena
8. Some authors define lymphocytic vasculitis as a condition involving lymphocyte infiltration around blood vessels and fibrinoid necrosis of the vascular wall. In this scenario, lymphocytes cause direct damage to vascular endothelial cells and induce changes to the vascular wall, such as vascular fibrin deposition, coagulation, and vascular endothelial growth
9. In psoriasis and granulomatous vasculitis, lymphocyte-medicated vasculitis develops in early stages of the disease. The resulting immune complexes cause an inflammatory response involving leukocytes. The same report also highlighted the possibility of leukocyte infiltration and leukocytoclasia, which are secondarily seen in many diseases after vascular damage due to lymphocytes
10. Lymphocytes can also activate other inflammatory cells, including leukocytes, and can play an important role in leukocytoclastic vasculitis by activating Langerhans cells
11. The reports to date on leukocytoclastic vasculitis in tsutsugamushi disease indicate that studies on the histopathological findings of lesions around eschars are not sufficient. When erythematous papules caused by bites of larval trombiculid mites progress to ulcers or eschars, coagulative necrosis develops at a histopathological level, primarily due to lymphocytic vasculitis and thrombosis. As a secondary response to this, circulating immune complexes are deposited on the vascular wall and leukocytoclastic vasculitis accompanied by keratinocyte necrosis and neutrophil infiltration in the epidermis of the eschar area appear. Therefore, the vasculitis of tsutsugamushi disease is thought to be lymphocytic vasculitis and is not caused by leukocytes. To observe this phenomenon, lesions around eschars should be biopsied, not the eschar area itself.
Like tsutsugamushi disease, insect bites, NK/T cell lymphoma, and lymphomatoid granulomatosis can present with lymphocytic vasculitis. These diseases differ from tsutsugamushi disease in treatment and prognosis, and differentiation is very important. In the case of insect bites, clinical symptoms vary depending on the causative insect. In general, insect bites appear as erythematous macules or papules and blisters. On a histopathological level, edema of the papillary dermis and infiltration of lymphocytes and eosinophils around blood vessels within the reticular dermis are commonly seen. Eosinophil infiltration is rare in tsutsugamushi disease
6, and it was not observed in most cases (91.7%) of this study. Thus, eosinophil infiltration is helpful in differentiating between insect bites and tsutsugamushi disease. NK/T cell lymphoma consists of either Epstein-Barr-virus (EBV)-positive NK cells or, rarely, of T cells showing cytotoxicity. Indurated plaques or tumors may develop, and ulcers are common. These ulcers may show similar clinical manifestations to eschars found in tsutsugamushi disease. Histopathologically, lymphocytes, histiocytes, plasma cells, Reed-Sternberg cells, and atypical lymphocytes infiltrate the dermal and subcutaneous fat layers. Mitotic figures are often observed, angiocentric infiltration is noticeable, blood vessel destruction is severe, and necrosis of the surrounding tissues occurs. Most cases of NK/T cell lymphoma are CD56 positive, EBV positive, TIA-1 positive, granzyme positive, perforin positive, and CD3 negative. Lymphomatoid granulomatosis primarily invades the lungs, and skin symptoms such as erythematous macules, papules, plaques, and nodules appear in approximately 40% of cases
12. It is classified as a B cell lymphoma, and its pathogenesis involves EBV. Histopathologically, it is characterized by vascular destruction and vascular infiltration of lymphocytes and histiocytes. Atypical lymphocytes and mitotic figures are also observed, and it is CD20, CD3, and CD4 positive
13. Tsutsugamushi disease involves infiltration of atypical lymphohistiocytes (consisting of lymphocytes, histiocytes, plasma cells, Reed-Sternberg cells, and atypical lymphoid cells), which can also be observed in angiocentric lymphoma. Tsutsugamushi disease also involves mitotic figures and vascular invasion, and the disease is included in the category of pseudolymphoma. It is important to differentiate between these diseases by completely understanding their clinical, histopathological, and immunohistochemistry findings.
In this study, the clinical manifestations and laboratory findings of tsutsugamushi disease were investigated. By observing the histopathological findings of lesions around eschars, we confirmed that tsutsugamushi disease is considered a pseudolymphoma. The major findings were lymphocytic vasculitis and infiltration of atypical lymphohistiocytes around blood vessels, mimicking angiocentric lymphoma. Especially, leukocytoclastic vasculitis and neutrophil infiltration were not observed in all cases. This is significant because the findings are different from histopathological findings of the eschar areas that have been reported to date. This result indicates that the existing proposed mechanism of vasculitis in tsutsugamushi disease should be adjusted. In conclusion, the vasculitis of tsutsugamushi disease is not caused by neutrophils but is instead a lymphocytic vasculitis. To observe this finding, biopsies should be performed on lesions around the eschar, instead of on the eschar area itself.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download