This article has been corrected. See "Erratum: Disseminated Superficial Actinic Porokeratosis in a Patient with Psoriasis, after Long-Term Narrowband Ultraviolet B Phototherapy" in Volume 30 on page 511.
Abstract
Porokeratosis is a rare epidermal disorder characterized by annular or linear hyperkeratotic plaques with slightly raised thread-like borders, and in most cases, atrophic centers. Disseminated superficial porokeratosis and disseminated superficial actinic porokeratosis (DSAP), which primarily involve sun-exposed areas, are common types of porokeratoses. Histologically, a column of parakeratotic cells, a so-called cornoid lamella, is a hallmark of porokeratosis. Porokeratosis is considered to result from the inability to eliminate an abnormal keratinocyte clone induced by genetic factors and various stimuli, including sunlight, artificial ultraviolet light, viral infections, immunosuppressive conditions (hematologic malignancies, organ transplants, or autoimmune disease), and immunosuppressive therapies. Here, we report a 59-year-old Korean woman with DSAP that developed after narrowband ultraviolet B (NB-UVB) therapy for psoriasis. Our case emphasizes the occurrence of DSAP due to NB-UVB that is able to induce local immunosuppression at the irradiated site; the pathogenesis of DSAP remains unclear.
Porokeratosis is a rare epidermal disorder characterized by annular or linear hyperkeratotic plaques, with slightly raised thread-like borders. The histologic characteristic of porokeratosis is the presence of “cornoid lamellae.” Porokeratosis is considered to occur as a result of the inability to eliminate an abnormal keratinocyte clone induced by genetic factors and various stimuli, including sunlight, artificial ultraviolet (UV) light, viral infections, and immunosuppressive conditions (hematologic malignancies, organ transplants, autoimmune disease, or immunosuppressant therapies)123. Disseminated superficial porokeratosis (DSP) and disseminated superficial actinic porokeratosis (DSAP), which primarily involve sun-exposed areas, are common types of porokeratoses that demonstrate multiple, small, asymptomatic lesions4. Here, we report a case of DSAP arising after narrowband UVB (NB-UVB) psoriasis therapy. This may be the first reported case of DSAP arising after repeated exposure to NB-UVB in Korea.
A 59-year-old woman (skin type IV) had generalized plaque-type psoriasis for 40 years. She had primary hypertension and hyperlipidemia, but her general health was otherwise unremarkable. The patient's family history did not include porokeratosis or psoriasis. Forty years prior to presentation, she had been treated with NB-UVB and systemic acitretin for 10 years. At that time, her symptoms improved and she discontinued treatment after she married and became pregnant. Twenty years later, her psoriasis recurred, and she was again treated with systemic acitretin and NB-UVB. Three years prior to presentation, she began only NB-UVB therapy, without oral medication, but she experienced repeated improvement and aggravation cycles. At that time, her skin symptoms were suspected to indicate porokeratosis, and the treatment was stopped. She was then referred to our dermatology department.
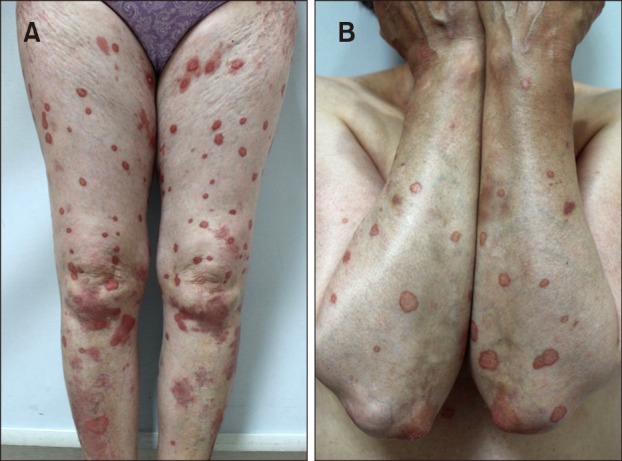
A dermatological examination revealed various annular, scaly patches and plaques, with raised keratotic margins (0.5~5.0 cm in diameter). The plaques were bilaterally located over her entire body (Fig. 1). Some lesions were small, annular plaques with sharp, elevated borders. Many larger plaques (approximately 5.0 cm long) were present on her right shin, and exhibited a typical psoriatic appearance of erythema and thick scales.
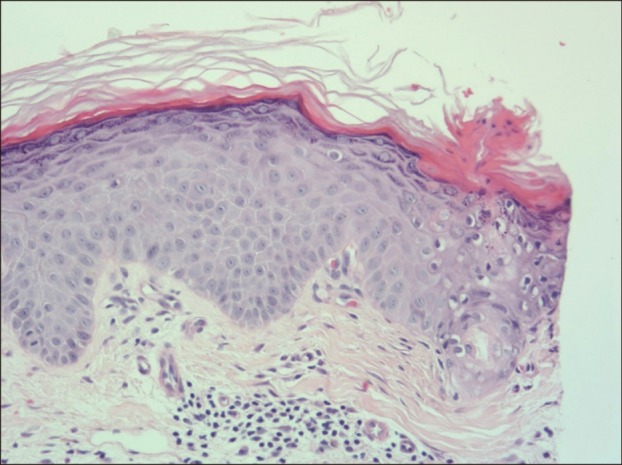
Histopathological examination of a biopsy specimen from a plaque with a thread-like border on her right leg showed the characteristic features of porokeratosis, including cornoid lamellae, irregularly arranged keratinocytes in the spinous layer, and superficial perivascular lymphocytic infiltration in the dermis (Fig. 2).
Porokeratosis is considered to be a chronic progressive disorder of keratinization with an unclear pathogenesis. The condition may be autosomally inherited, although most cases are idiopathic1. Two disseminated forms have been described: DSAP, which is the most common variant, and DSP, a non-actinic variant56. The condition typically manifests during the third and fourth decades of life. Clinically, multiple (>50) small (<1 cm) annular plaques are observed, with thread-like borders; in most cases, atrophic centers are present, usually appearing in sun-exposed areas of skin7.
A column of parakeratotic cells, the so-called cornoid lamella, is a histological hallmark of porokeratosis, and a perivascular lymphohistiocytic infiltrate, which may be focally lichenoid, also presents8.
Although the pathogenesis of porokeratosis is unknown, it may include a combination of genetic and environmental factors. Sun exposure, genetic susceptibility, and immunosuppression are the main factors triggering DSAP, presumably because of induced immunosuppression9. Development of DSAP after chronic UV exposure, including oral psoralens and UVA (PUVA), topical PUVA, broadband UVB, and NB-UVB psoriasis therapies and sun bathing, have also been reported61011121314.
Dermatologically, NB-UVB is a useful treatment option for several skin diseases, including psoriasis, vitiligo, pityriasis rosea, and mycosis fungoides. NB-UVB therapy modulates cytokines, irradiates T cells (important for the prevention of porokeratotic clonal growth), and induces apoptosis; thus, the immune system is suppressed and inflammation is reduced915161718. Hence, focal immunosuppression may be induced by UV irradiation of the irradiated site. Following immunosuppression due to long-term NB-UVB phototherapy, genetically susceptible individuals have been documented to experience induced expression of abnormal epidermal cell clones, disruption of epidermal growth, and promotion of clonal cell proliferation18.
In conclusion, we reported a case of DSAP that developed in a patient with psoriasis, after long-term NB-UVB phototherapy. This may be the first reported case of DSAP occurring after repeated exposure to NB-UVB in Korea. Although this condition is uncommon, clinicians should be aware of the potential development of DSAP in patients receiving immunosuppressive treatments such as NB-UVB therapy.
References
1. Kanitakis J, Euvrard S, Faure M, Claudy A. Porokeratosis and immunosuppression. Eur J Dermatol. 1998; 8:459–465. PMID: 9854155.
2. Jung JY, Yeon JH, Ryu HS, Youn SW, Park KC, Huh CH. Disseminated superficial porokeratosis developed by immunosuppression due to rheumatoid arthritis treatment. J Dermatol. 2009; 36:466–467. PMID: 19691753.

3. Neumann RA, Knobler RM, Metze D, Jurecka W. Disseminated superficial porokeratosis and immunosuppression. Br J Dermatol. 1988; 119:375–380. PMID: 2972310.

4. Kawara S, Oiso N, Kawada A. Disseminated superficial actinic porokeratosis in a patient undergoing treatment with long-term narrowband ultraviolet B for psoriasis. J Dermatol. 2011; 38:585–587. PMID: 21914157.

5. Chernosky ME, Anderson DE. Disseminated superficial actinic porokeratosis. Clinical studies and experimental production of lesions. Arch Dermatol. 1969; 99:401–407. PMID: 5769325.

6. Takahashi H, Takahashi I, Iinuma S, Honma M, Iizuka H. Disseminated superficial actinic porokeratosis in a psoriasis patient with a long-term sun-bathing habit. J Dermatol. 2015; 42:532–533. PMID: 25720967.

7. Chernosky ME. Porokeratosis: report of twelve patients with multiple superficial lesions. South Med J. 1966; 59:289–294. PMID: 5910629.

8. Mibelli V. Contributo allo studio della ipercheratosi dei canali sudoriferi (porokeratosis). G Ital Mal Vener. 1893; 28:313–355.
9. Murase J, Gilliam AC. Disseminated superficial actinic porokeratosis co-existing with linear and verrucous porokeratosis in an elderly woman: update on the genetics and clinical expression of porokeratosis. J Am Acad Dermatol. 2010; 63:886–891. PMID: 20451293.

10. Reymond JL, Beani JC, Amblard P. Superficial actinic porokeratosis in a patient undergoing long-term PUVA therapy. Acta Derm Venereol. 1980; 60:539–540. PMID: 6162345.
11. Lederman JS, Sober AJ, Lederman GS. Psoralens and ultraviolet A, immunosuppression, and porokeratosis. J Am Acad Dermatol. 1986; 14:284–285. PMID: 3950130.

12. Hazen PG, Carney JF, Walker AE, Stewart JJ, Engstrom CW. Disseminated superficial actinic porokeratosis: appearance associated with photochemotherapy for psoriasis. J Am Acad Dermatol. 1985; 12:1077–1078. PMID: 4008702.

13. Allen AL, Glaser DA. Disseminated superficial actinic porokeratosis associated with topical PUVA. J Am Acad Dermatol. 2000; 43:720–722. PMID: 11004640.

14. Cockerell CJ. Induction of disseminated superficial actinic porokeratosis by phototherapy for psoriasis. J Am Acad Dermatol. 1991; 24:301–302. PMID: 2007687.

15. Gilmour JW, Vestey JP, George S, Norval M. Effect of phototherapy and urocanic acid isomers on natural killer cell function. J Invest Dermatol. 1993; 101:169–174. PMID: 8345217.

16. Sigmundsdottir H, Gudjonsson JE, Valdimarsson H. The effects of ultraviolet B treatment on the expression of adhesion molecules by circulating T lymphocytes in psoriasis. Br J Dermatol. 2003; 148:996–1000. PMID: 12786832.

17. Tobin AM, Maguire B, Enright H, Kirby B. The effects of phototherapy on the numbers of circulating natural killer cells and T lymphocytes in psoriasis. Photodermatol Photoimmunol Photomed. 2009; 25:109–110. PMID: 19292789.

18. Bencini PL, Tarantino A, Grimalt R, Ponticelli C, Caputo R. Porokeratosis and immunosuppression. Br J Dermatol. 1995; 132:74–78. PMID: 7756155.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download