Dear Editor:
Atrophoderma vermiculatum (AV) is a rare, slowly progressive, benign follicular disorder that affects primarily children1. AV is characterized by the development of inflammatory, keratotic papules of the face that form pitted, atrophic, and depressed scars in a reticular or honeycomb pattern12.
A 12-year-old girl presented with sudden onset of atrophic scarring of both cheeks. Examination showed multiple, pitted, honeycomb scars on the both cheeks, temples, chin and neck. The lesions were similar regarding their size and morphology, were oval shaped, skin-colored, 1~2 mm in diameter, and approximately 1 mm deep (Fig. 1A, B). The lesions had developed several years prior and had gradually expanded centrifugally. Neither the eyebrows nor eyelashes were involved; no scarring alopecia was evident. The patient denied any subjective symptoms including itching or pain. Her medical history contained atopic dermatitis but no evidence of any physical trauma or inflammation prior to disease onset. The physical examination and routine laboratory test showed all normal results. There was no relevant family history.
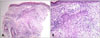
Histopathological examination of a punch biopsy specimen of an atrophic keratotic papule on the cheek revealed follicular hyperkeratosis; aberrant, atrophic pilosebaceous units formed small finger-like projections into the surrounding connective tissue, accompanied by sclerosis of the dermal collagen. Both mild perifollicular fibrosis and chronic perifollicular inflammation were apparent (Fig. 2).
The clinical and histopathological features and the age of the patient allowed us to diagnose AV. The patient was treated with daily 0.01% topical tretinoin. At the 12-month follow-up examination, lesional progression had ceased, and the lesions were slightly lighter in color and cosmetically improved. The lesions did not completely regress, but no additional scarring developed, and the patient's appearance improved (Fig. 1C, D).
AV, also known as folliculitis erythematosa reticulata, typically presents in childhood. However, our patient's age of onset was older than the typical age. Early erythema and follicular keratotic papules slowly progress to atrophy, characterized as worm-eaten, reticular, or honeycomb in appearance, evident on the cheeks, pre-auricular area, and forehead123. In the present case, the skin lesions suddenly occurred, furthermore, compared to typical lesion, more extensive lesions were observed up to the chin and neck. The extent of inflammation, presence/absence of milia, and extent of follicular plugging are all variable. AV, along with keratosis pilaris atrophicans (KPA) faciei and keratosis pilaris spinulosa decalvans, are clinical variants of KPA23. The etiology of AV remains unclear. AV is typically sporadic, although autosomal dominant inheritance has been reported. The defect is believed to be attributed to abnormal keratinization of the pilosebaceous follicle. Treatment of all types of KPA is challenging and often unrewarding. Most treatments are topical keratolytics, topical and intralesional corticosteroids, topical and oral retinoids, oral antibiotics and ultraviolet irradiation therapy23. When the condition stabilizes, dermabrasion, collagen implantation, and laser therapy (carbon dioxide, pulsed dye lasers and erbium Yttrium Aluminum Garnet laser) can be considered234.
Our patient presented with abrupt onset AV in adolescence, which is unusual. To our knowledge, there is only one case of AV in Korean literatures5. Herein, we report a rare and interesting case of patient with AV with history of atopic dermatitis who had sudden onset of extensive skin lesion, and showed good therapeutic response to topical tretinoin.
Figures and Tables
Fig. 1
(A, B) Multiple, pitted oval in shape, skin-colored, 1~2 mm in diameter, and approximately 1 mm deep scars were evident on both cheeks (red arrow, yellow circle) and temples, and the chin and neck. (C, D) After treatment with 0.01% topical tretinoin for 12 months, pitlike erythematous atrophic scars improved cosmetic appearance (red arrow, yellow circle).

Fig. 2
Histopathological examination of an atrophic keratotic papule on the cheek revealed follicular hyperkeratosis; aberrant, atrophic pilosebaceous units, accompanied by sclerosis of the dermal collagen. Mild perifollicular fibrosis and chronic perifollicular inflammation were apparent (H&E; A: ×100, B: ×200).
References
1. Frosch PJ, Brumage MR, Schuster-Pavlovic C, Bersch A. Atrophoderma vermiculatum. Case reports and review. J Am Acad Dermatol. 1988; 18:538–542.
2. Luria RB, Conologue T. Atrophoderma vermiculatum: a case report and review of the literature on keratosis pilaris atrophicans. Cutis. 2009; 83:83–86.
3. Apalla Z, Karakatsanis G, Papageorgiou M, Kastoridou C, Chaidemenos G. A case of atrophoderma vermiculatum responding to systemic isotretinoin. J Dermatol Case Rep. 2009; 3:62–63.

4. Park J, Kim BJ, Kim MN, Lee CK. A pilot study of Q-switched 1064-nm Nd:YAG laser treatment in the keratosis pilaris. Ann Dermatol. 2011; 23:293–298.

5. Shim C, Song DH, Lee SH, Kim DS. Atrophoderma vermiculatum occuring in a patient with congenital heart disease. Korean J Dermatol. 1989; 27:222–226.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download