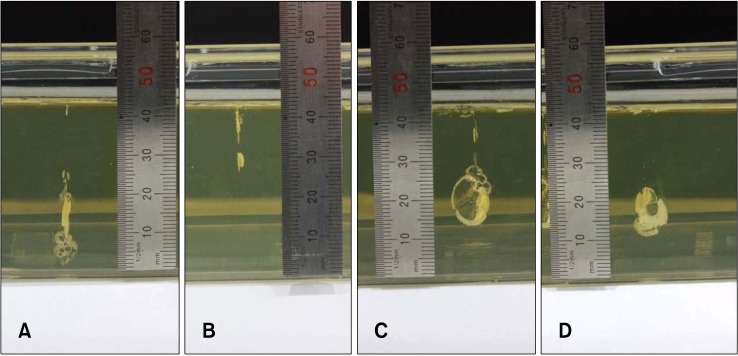
 | Fig. 1(A) Tissue-mimicking (TM) phantom only (Group 1), penetration depth: 5.7 cm. (B) TM phantom+ polyethylene vinyl (Group 2), penetration depth: 3.2 cm. (C) TM phantom+polyethylene vinyl+120 µm hole (Group 3), penetration depth: 4.5 cm. (D) TM phantom+ polyethylene vinyl+430 µm hole (Group 4), penetration depth: 4.8 cm. |
Dear Editor:
Pneumatic needle-free injection devices are widely used for skin rejuvenation and scar treatment purposes12. They are often used in combination with other treatment methods in order to increase treatment effectiveness34. Cadaver studies confirmed that injection fluid enters the skin at different depths and shapes depending on pressure when using only a pneumatic needle-free injection device. However, it has not been determined what occurs when performing such treatments together with other methods5. In this study, we generated models for subcision and fractional laser treatments, which are used widely for scars and wrinkles, and tested them on a tissue-mimicking (TM) phantom.
We pneumatically injected hypertonic glucose solutions at a 20% concentration into a TM phantom in order to assess fluid infiltration tendencies and patterns. We generated the TM phantom in order to mimic tissue responses induced by pneumatic injections under diverse conditions. We prepared a transparent gelatin phantom as described in a previous study with only minimal modification by mixing 12.5% (w/v) gelatin (Sigma-Aldrich, St. Louis, MO, USA) with distilled water6. We promptly poured the combination into a polycarbonate housing after degassing and let the mixture stiffen in a refrigerator for 12 hours at 39.2℉ (4℃). We then built a polycarbonate frame to accurately replicate the injection of experimental solutions under all test circumstances. This required the instrument's handpiece to be held by the frame. The injection button was controlled remotely to ensure the stabilization of the handpiece. A transcutaneous pneumatic injection device (SheMax™; Shenb Co., Ltd., Seoul, Korea) was used for injections. The injections into the TM phantom were performed with a nozzle diameter of 200 µm, and at a pressure of 3.63 bar 0.01 ml/injection.
After treatment with the fractional laser, we used the pneumatic needle-free injection device to perform injections under the 4 following conditions: 1) Without any resistance, TM phantom only (Group 1); 2) with 0.02 m of polyethylene vinyl applied to cover the TM phantom, in order to replicate the conditions of the epidermis, TM phantom+polyethylene vinyl (Group 2); 3) TM phantom+ polyethylene vinyl+120 µm hole (Group 3); and 4) TM phantom+polyethylene vinyl+430 µm hole (Group 4). The 120 µm holes were created using the DeepFX handpiece of the UltraPulse Encore (Lumenis Inc., Palo Alto, CA, USA), and the 430 µm holes were generated using the ProFractional-XC (Sciton Inc., Palo Alto, CA, USA).
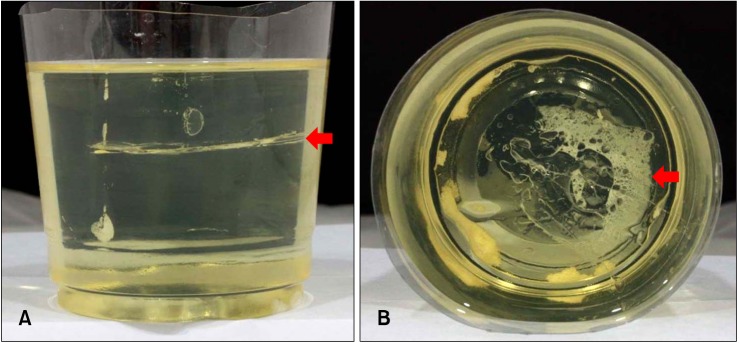
In order to observe outcomes of using pneumatic needle-free injection devices after subcision, we performed injections of the TM phantom after subcision at its center with a 18 gauge needle.
When using a pneumatic needle-free injection device after performing fractional laser treatment, the depths that the injections reached were: 5.7 cm (Group 1), 3.2 cm (Group 2), 4.5 cm (Group 3), and 4.8 cm (Group 4) (Fig. 1). We confirmed that the injected material would diffuse in the subcision plane when using a pneumatic needle-free injection device after subcision (Fig. 2).
Pneumatic needle-free injections are a new method for introducing diverse substances into the skin. Such substances may include aesthetic medicines, hyaluronic acid, botulinum toxin, and placental extracts. Studies of these devices have recently been performed, and are beginning to reveal positive effects on scar remodeling by stimulating the fibroblasts via micro-trauma and activating neocollagenesis, in addition to administering extended skin planes17. In studies using mice, pneumatic needle-free injections promoted collagen synthesis and enhanced dermal thickening8. As proof of the effectiveness of pneumatic needle-free injections accumulates, this method is now being applied for skin rejuvenation and scar treatment. Furthermore, it is being tested for combination therapy with other forms of treatment. Treatments used in combination therapy include fractional laser and subcision. We previously examined the phenomena that occur when these methods are used together with pneumatic needle-free injection910.
When using pneumatic needle-free injection devices after using a fractional laser, we have found that the material reaches greater depths with all other conditions being equal. We also found that the larger the hole size created by the fractional laser, the greater the depth the material reached. Therefore, when using a pneumatic needle-free injection device after using a fractional laser, if a clinician desires to inject material at the same depth as when a fractional laser was not used before the injection, the clinician would need to apply less pressure, and the pressure is expected decrease as the hole size grows larger.
Using a pneumatic needle-free injection device after subcision results in the diffusion of the injected material as it enters the subcision plane. Therefore, when performing subcision, it is important to cautiously define the depth to which one desires to have the material diffuse, and to control the pressure of the injection device so that the material will reach at least the depth of the subcision plane. When using this method, clinicians are expected to be able to introduce materials evenly at the subcision plane when injecting materials that have a low cohesivity and high loss modulus (G″). This method is also expected to be useful for preventing injected material from penetrating to undesired depths.
The limitations of this study are that we were only able to perform our experiments on the TM phantom, and therefore may not be generalizable to predict the results of injections performed on actual human skin. In addition, as polyethylene vinyl cannot exactly represent the resistance characteristics of the epidermis, the results of this study may only cautiously be applied for the treatment of actual patients. In this study, we sought to reveal phenomena that can occur when using pneumatic needle-free injection in company with other methods of treatment. In the future, there will be a need to observe differences in efficacy and histologic changes when performing combination therapy on actual human patients.
References
1. Levenberg A, Halachmi S, Arad-Cohen A, Ad-El D, Cassuto D, Lapidoth M. Clinical results of skin remodeling using a novel pneumatic technology. Int J Dermatol. 2010; 49:1432–1439. PMID: 21091682.

2. Seok J, Hong JY, Jang JH, Bae JH, Choi SY, Yoo KH, et al. The NEEDLELESS MICROJET: a novel device for hypertrophic scar remodelling on the forehead. J Eur Acad Dermatol Venereol. 2016; 30:e145–e146. PMID: 26537185.

3. Seok J, Kwon HJ, Choi SY, Yoo KH, Oh CT, Kim BJ. Successful treatment of thyroidectomy scar with a pneumatic needleless injector and silicone gel. Int Wound J. 2016; 13:1089–1090. PMID: 26991428.

4. Seok J, Choi SY, Park KY, Jang JH, Bae JH, Kim BJ, et al. Depressed scar after filler injection successfully treated with pneumatic needleless injector and radiofrequency device. Dermatol Ther. 2016; 29:45–47. PMID: 26301992.

5. Seok J, Oh CT, Kwon HJ, Kwon TR, Choi EJ, Choi SY, et al. Investigating skin penetration depth and shape following needle-free injection at different pressures: a cadaveric study. Lasers Surg Med. 2016; 48:624–628. PMID: 27075398.

6. Ding T, Zhang S, Fu Q, Xu Z, Wan M. Ultrasound line-byline scanning method of spatial-temporal active cavitation mapping for high-intensity focused ultrasound. Ultrasonics. 2014; 54:147–155. PMID: 23673346.

7. Stachowiak JC, Li TH, Arora A, Mitragotri S, Fletcher DA. Dynamic control of needle-free jet injection. J Control Release. 2009; 135:104–112. PMID: 19284969.

8. Kwon TR, Seok J, Jang JH, Kwon MK, Oh CT, Choi EJ, et al. Needle-free jet injection of hyaluronic acid improves skin remodeling in a mouse model. Eur J Pharm Biopharm. 2016; 105:69–74. PMID: 27257030.

9. Carniol PJ, Hamilton MM, Carniol ET. Current status of fractional laser resurfacing. JAMA Facial Plast Surg. 2015; 17:360–366. PMID: 26133312.

10. Orentreich DS, Orentreich N. Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg. 1995; 21:543–549. PMID: 7773602.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download