INTRODUCTION
Melasma is an acquired pigmentary disorder presenting brownish patches on the face, most commonly observed in females with a darker skin type. The major etiological factors are genetic influences, exposure to ultraviolet (UV) radiation, and sex hormones
1, although the exact pathogenesis of melasma is not fully elucidated. The pathophysiology of melasma is believed to involve excess production of melanin or an increase in the number of melanocytes in the skin. Laser toning using low-fluence 1,064 nm Q-switched Nd:YAG laser (QSNY) has been an effective treatment option in Asia, but monotherapy treatment efficacies were variable
234.
Recent studies have suggested that interactions between the altered cutaneous vasculature and melanocytes have an influence on hyperpigmentation development in melasma, which demonstrated that greater vascularity is one of the major findings
56. Based on this finding, it has been investigated whether the treatment targeting blood vessels is beneficial in the treatment of melasma
7891011. Pulsed-dye laser (PDL) is considered a gold standard laser therapy for cutaneous vascular lesions, which has been shown to be an effective treatment option in combination with pigment-targeted modalities for melasma patients in several studies
78910. Also, it has been reported that the copper bromide laser, oral and topical tranexamic acid are effective in the treatment of melasma
7891011.
Dermoscopy is a useful tool for detecting clinically invisible or neglectable vessel changes effectively. We thought these findings may be helpful for the candidate selection for treatment including vascular-target therapy. Several studies have been reported the effect of PDL in melasma treatment, but there has been no comparative study on the therapeutic effect of PDL between melasma patients who show dermoscopic finding of visibly widened capillaries and who do not. Therefore, this study was conducted to investigate whether PDL provides additional improvements when combined with QSNY for melasma treatment, using dermoscopy to find subtle vascular structures and evaluated whether these findings showed differences.
Go to :

MATERIALS AND METHODS
Study subjects
We conducted a randomized, single-blind, split-face prospective study between December 2015 and April 2016. Seventeen Korean women with melasma aged 18 years or above were included in the present study. The Fitzpatrick skin type was determined for all patients. The exclusion criteria included underlying skin diseases, use of isotretinoin or contraceptive pills during the past six months, pregnancy or breastfeeding, topical bleaching agent usage within one month before recruitment, employment of chemical peels, laser therapy or intense pulsed light treatment also within six months at the study's beginng, and sunlight or UV light exposures. This clinical study was approved by the Institutional Review Board of Ulsan University Hospital (Ulsan, Korea) (IRB no. 2014-03-006) and written informed consent was obtained from all subjects.
Treatment methods
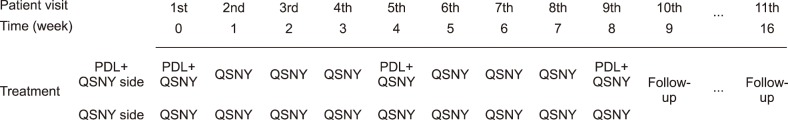
Fig. 1. shows a schematized summary of the treatment schedule. A total of 17 patients were treated, and each side of the face was randomly allocated to either QSNY or PDL+QSNY treatment. All subjects were treated with a total of nine full-face QSNY treatment sessions (Cosjet TR®; Won Technology, Daejeon, Korea) at one-week intervals. On the PDL+QSNY side of the face, additional PDL treatments (Cynergy Multiplex™; Cynosure, Westford, MA, USA) were performed with a total of three sessions at baseline, week 4, and week 8. The patients were treated first with low-fluence QSNY on the entire face and subsequent PDL treatment was performed immediately after QSNY treatment on the half of the face with a 10% overlap of treatment spots to target the vessels. Both laser therapy were stopped when mild erythema appeared around the melasma lesion. No anesthesia was necessary prior to the treatment. The assignment to treatments was made only when a subject attended the first therapy session. Laser parameters for QSNY settings were a 1,064 nm wavelength, 7 mm spot size, and a fluence of 1.2~2.0 J/cm
2 at 10 Hz (five to seven passes), whereas the PDL settings were of a 595 nm wavelength, seven mm spot size, a 20-milisecond pulse duration, as well as a 7~8 J/cm
2 fluence (two to three passes). The patients were not allowed to use any other form of treatment or functional cosmetics and they were also instructed to avoid sun exposure and to apply a broad-spectrum sunscreen.
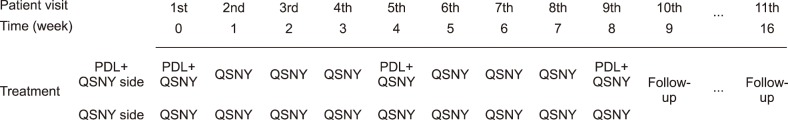 | Fig. 1Schematized summary of treatment schedule. PDL: pulsed-dye laser, QSNY: Q-switched Nd:YAG laser.
|
Efficacy assessments
Before each session, one week after the last treatment (week 9), and follow-up visits after eight weeks since the last treatment (week 16), digital photographic documentation (Nikon D7000; Nikon Corporation, Tokyo, Japan) was obtained under the same conditions. Dermoscopic images were also obtained using dermoscopy equipment (X20) (DermLite II Pro; 3Gen, San Juan Capistrano, CA, USA). Calibration of the different parameters (luminosity, contrast, white balance, color balance) was performed prior to starting a series of images. To visualize vessels, the glass lens was carefully placed on the lesion; also, minimal pressure was applied. Based on the fact whether the visibly widened capillaries were detected or not in dermoscopic images, estimations were made. Two independent dermatologists evaluated the melasma area and severity index (MASI) scores, using the photographs taken at baseline, week 9 and 16. The mean value of the data obtained from each half of the face was calculated and the mean percentage change was compared. Hemi-MASI score was used because of the study design of split-face, and it was calculated based on the percentage of the involved area (A=0~6: 0=0%, 1=1%~9%, 2=10%~29%, 3=30%~49%, 4=50%~69%, 5=70%~89%, 6=90%~100%), darkness of pigment (D=0~4: 0=absent or normal skin color without evidence of hyperpigmentation, 1=slight visible hyperpigmentation, 2=mild visible, 3=marked, 4=severe), and homogenicity of the hyperpigmentation (H=0~4: 0=minimal, 1=slight, 2=mild, 3=marked, 4=severe).
Hemi-MASI score=forehead, 0.15×(D+H)×A+malar, 0.30×(D+H)×A+chin, 0.05×(D+H)×A.
Safety assessments
At each follow-up visit, adverse events were also evaluated. Patients were asked to reports side effects such as erythema, burning, swelling, blistering, crust, hyperpigmentation or hypopigmentation, atrophy, and others during and after treatment. The dermatologist categorized the degree of erythema and burning into four grades: none, mild, moderate, and severe.
Statistical analysis
All analyses were performed using SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). Continuous variables were described as means and standard deviations (SD). Data were analyzed using Mann-Whitney U-test. p<0.05 was considered statistically significant.
Go to :

DISCUSSION
Melasma is a chronic distressing condition and often therapeutically challenging. Various treatments, including whitening or bleaching agents (e.g., hydroquinone, azelaic acid), chemical peels (e.g., glycolic, β-hydroxyl, and trichloroacetic acids), topical steroids, as well as laser treatment demonstrated some therapeutic effect but were often unsuccessful with regard to refractory melasma
1213. A large-spot-size, low-energy-mode of the 1,064 nm QSNY is a popular method of melasma therapy in Asia. The QSNY has a longer wavelength that can penetrate deeper to target both mixed and dermal melasma. It can also target lesional melanocytes and causes of subcellular damage to its melanin particles precisely
1415. Moreover, QSNY may also produce nonspecific dermal wounds and induce inflammation, facilitating a migration of melanophages
16. However, these effects were transient and reversible, with a high recurrence rate
91011.
The pathogenesis of melasma is not completely understood, which renders treatment more complicated. There are many possible contributing factors which include genetic influences, exposure to UV radiation, female sex hormones, thyroid dysfunction, cosmetics, and drugs
1. Although the cause of melasma has not been fully comprehended, it has recently been suggested that vascular endothelial growth factor (VEGF) and skin vascularization might play a role in the melasma pigmentation
23. Human melanocytes may respond to angiogenic factors because normal human melanocytes show functional VEGF receptors. Therefore, VEGF may have a direct influence on melanocyte behavior through its receptors
23. It is also known to stimulate the release of arachidonic acid as well as the phosphorylation and activation of cytosolic phospholipase A2. It is possible that the resulting metabolites from the arachidonic acid pathway affect melanogenesis
23.
Cho et al.
2 reported that only the area affected by melasma presents a pronounced vascular change, showing significant increases in the number and size of dermal blood vessels. Moreover, they considered that the number of vessels is positively related to the degree of pigmentation. Park et al.
17 demonstrated that the degree of erythema is positively correlated with that of pigmentation in a melasma lesion. Thus, vascularity increases may play an important role in the melasma pathogenesis and the cause of PIH after laser therapy by an increase of cytokines and soluble factors released from proliferated vessels
17.
From this point of view, laser targeting blood vessel might decrease the stimulation of melanocytes and prevent relapse. PDL targets oxyhemoglobin within cutaneous vasculatures and it has been widely employed to treat diverse vascular disorders. By targeting not only melanin but also vascularization, PDL might provide—in combination with QSNY—an effective and successful therapeutic approach for melasma.
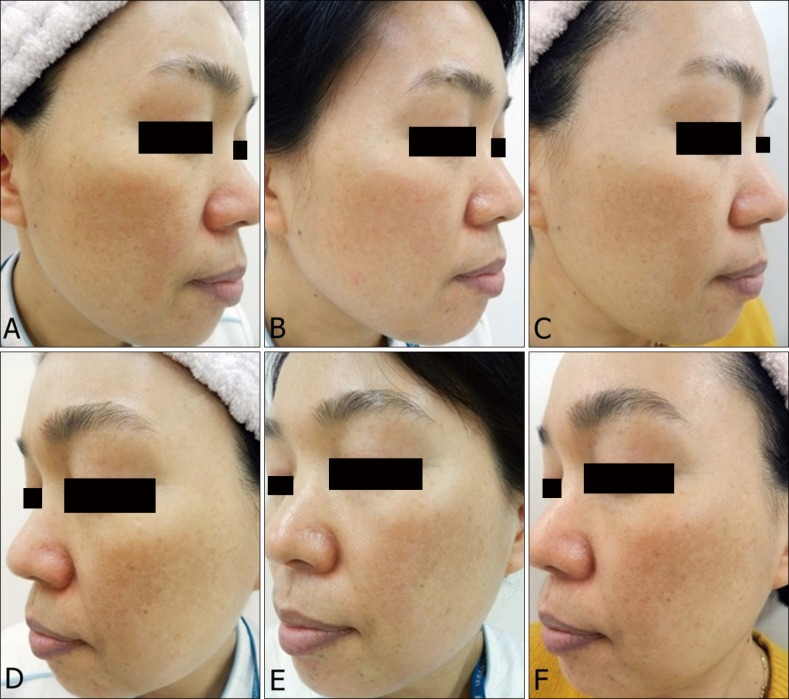
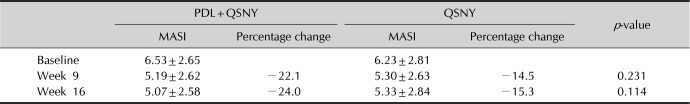
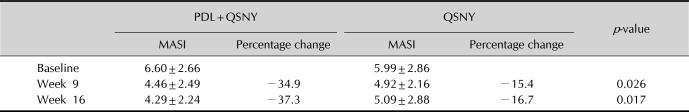
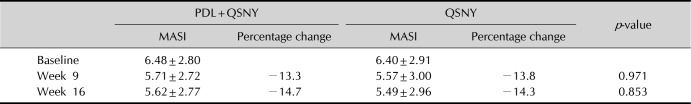
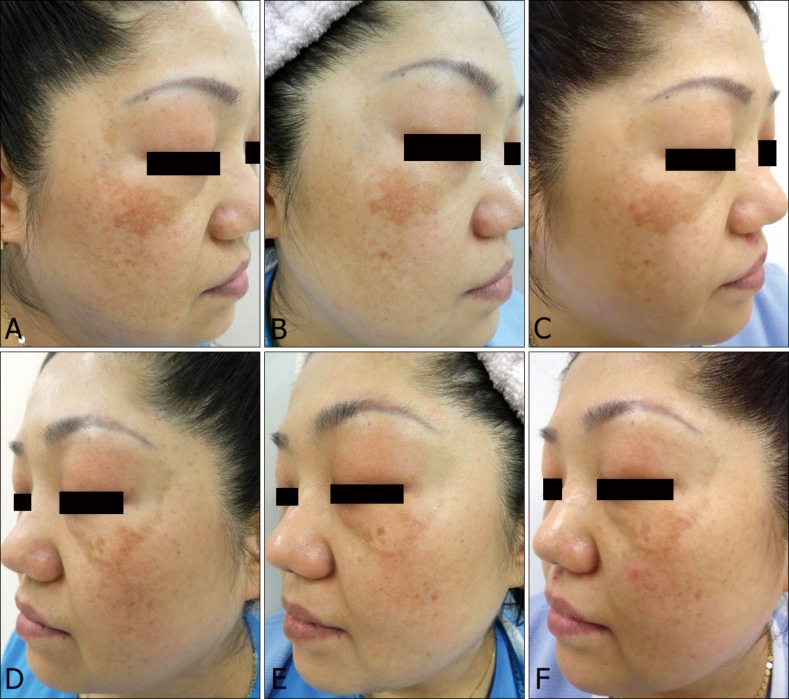
In our split-face study, the MASI scores of both sides decreased significantly during the study period. There was no significant difference in the MASI score change between both sides in all periods. Some of the patients exhibited a greater improvement and all of them had visibly widened capillaries on dermoscopic image. These seven patients showed significant difference in both sides in terms of changes in the MASI score during treatment (p=0.026).
It is reasonable to assume that the efficacy of PDL+QSNY is greater in a melasma with obvious vascular lesions. Moreover, not only the PDL+QSNY reveals an effectiveness in MASI score reduction of during the treatment period, but there was also a tendency for relapse prevention after treatment, while only-side QSNY revealed an increase of the MASI score during the follow-up period.
Laser parameter settings for low fluence QSNY are relatively well established in the Asian melasma treatments. However, in most previous studies which used QSNY at 2.5~4.0 J/cm
2, there were adverse events such as postinflammatory hypopigmentation and punctate leukoderma
234. Thus, we used lower fluence of 1.2~2.0 J/cm
2 than previous studies to minimize the possibility of these unwanted outcomes.
Geddes et al.
7 and Passeron
9 investigated the effect of vascular targeted therapy of melasma and they chose PDL setting as energy fluence of 7.5~8 J/cm
2 and 10 J/cm
2, respectively. These laser settings were chosen to minimize thermal damage and risk of rebound melasma. In addition to these studies, in our preliminary study for determining the parameter of PDL, we observed several cases of purpura after PDL treatment using short pulse width. Thus, we used long pulse width to prevent purpura. Also, we assumed that even though ten patients did not show vascular prominence at dermoscopy finding, they may get subclinical improvement after PDL treatment. Indeed, PDL+QSNY treatment reduced MASI scores of the lesion among these 10 patients (
Table 3).
Even with our conservative PDL parameters (7 mm spot size, a 20-millisecond pulse duration, and a fluence of 7~8 J/cm2), two patients who both had visibly widened capillaries on dermoscopic images presented with adverse effects such as PIH and RH. Hence, an increase in vascularity may be potentially associated with increased inflammatory cytokines and enhanced melanogenesis. Along with excessive cumulative laser energy of PDL+QSNY, this might be a factor with regard to adverse effects such as PIH and RH in our study.
We judge that it can be difficult to clinically find a capillary underlying the melasma lesions. Dermoscopy aids in the visualization of the epidermis and dermis, which is usually used to diagnose pigmented lesions. Recently, it has also increasingly been used to find vascular lesions. The skin's structure can be observed on an enlarged scale, which helps effectively in identifying even subtle vascular structures. We used dermoscopy to detect subtle telangiectasia within melasma lesions. This may also allow the best candidates' selection for the addition of a vascular-targeted therapy and for monitoring a patient's treatment progress.
The study limitations included its small sample size and a relatively short follow-up period. Melasma relapses are common after a certain period despite proper treatments. We could not evaluate long-term results of efficacy in our melasma patients. Additionally, the characteristics of the split-face study make it difficult to detect improvement.
In conclusion, PDL combined with QSNY may be considered as an effective treatment for melasma patients who show visibly widened capillaries on dermoscopy. By targeting the vascular lesions in melasma, PDL may partially inhibit melanocyte activation. These findings could provide physicians with a melasma treatment concept, targeting multiple components. We believe that additional PDL treatment can be effective in managing melasma with a telangiectatic component. Also, dermoscopy may be a helpful diagnostic tool for the candidate selection for PDL treatment. Further prospectively oriented research with additional subjects, skin types, and a long-term follow-up is needed.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download