Abstract
The purpose of this study was to determine the length of the semitendinosus muscle belly and its tendon in South Indian population and to study the topography and diameter of its neurovascular pedicles. The study included 46 formalin fixed human cadaveric lower limbs. The length of the semitendinosus muscle belly and its tendon were measured. The neurovascular pedicles of the semitendinosus muscle were identified and counted. The diameter of the neurovascular pedicle was measured just before its entrance into the semitendinosus muscle. The topographical distance of the neurovascular pedicles from the origin of the semitendinosus muscle were determined. The mean length of the semitendinosus muscle belly was 332.3±36.1 mm and its tendon measured 154.8±31.9 mm. The mean diameter of the vascular pedicle was measuring 11.4±9.1 mm, just before its entrance into the semitendinosus muscle. The neurovascular pedicles, of the semitendinosus muscle were ranging between 1 and 7. The distance of the entrance of neurovascular pedicle to the semitendinosus muscle from its origin was ranging between 46 and 272 mm. It was observed that the neurovascular pedicles were highest (31%) at the range of 151–200 mm away from the ischial tuberosity. The morphometric data obtained in the present study is enlightening to the orthopedic and plastic surgeons. The topographical knowledge of the neurovascular pedicles has its implications during the harvesting of the grafts and pedicle flaps. The diameter of vessels in the pedicles is enlightening because of new method of anterior cruciate ligament reconstruction.
Semitendinosus (ST) muscle is among the hamstring muscles, which are located in the back of thigh region. As the name suggests, the ST muscle partly consists of tendon morphology. Its tendon begins approximately at two-thirds of the back of thigh [1]. This muscle has its proximal attachment at the ischial tuberosity and distally inserts into the deeper layer of medial surface of superior part of tibia as a part of pes anserinus [12]. The pes anserinus includes the tendinous insertions of Sartorius, gracilis and ST muscles. The tendon of ST muscle has its clinical application as the autograft in various surgeries. The ST muscle tendon autograft has been used for the anterior cruciate ligament reconstruction [34]. The ST muscle tendon graft is also used to reconstruct the tears of tendo-calcaneus [5]. The ST muscle allografts have given the good results in the reconstruction of lateral ligaments of ankle joint as well [6]. It was described that the preoperative knowledge of ST muscle tendon length will help the operating surgeon in choosing the alternative grafts [3].
The challenges in this procedure are variability in the length and thickness of the ST muscle tendon graft and the graft harvesting [78]. The ST muscle graft can be harvested as double, triple or quadruple forms or in association with the gracilis tendon and other combinations [3]. The topography of the entrance of neurovascular pedicles into the muscle is important to the operating plastic surgeons, while choosing the flaps [9]. It has been reported that, during the plastic surgery, proximal part of the muscle will be incised just superior to the entrance of its vascular pedicle and the superior margin of the flap will be elevated proximally [9]. However, in spite of the clinical implications, there are only few studies being reported about the morphometry of the ST muscle. The anatomical studies about the neurovascular pedicles of ST muscle from South Indian population are not being reported. The diameter of neurovascular pedicles is of interest because of the recent method of the reconstruction of the anterior cruciate ligament with a pedicle graft. It was described that the harvesting of graft may be sometimes difficult, because of lack of reports in the literature from an anatomical point of view, which can escort and help their harvesting [10]. In this context, the purpose of the present study was to provide the morphological database of the ST muscle, its tendon and its neurovascular pedicle from the South Indian population, which can be utilized by the operating surgeon during the procedures like reconstructions of anterior cruciate ligament, ligaments of the ankle joint and the tendo Achilles.
The present study included 46 formalin fixed adult human cadaveric lower limbs, of them 26 were right sided and 18 were left sided. The anatomical specimens which were utilized for the teaching of first year medical students were used for the present study. The cadavers were donated bodies and unclaimed bodies at the government hospital. They were received at the department of anatomy as per the ethical committee guidelines of our institution. The lower extremities were already disarticulated and were stored in a formalin tank. Because of this, the age and gender of the cadavers, could not be determined. Specimens with congenital deformities like genu valgum, genu varum and below knee amputated specimens were excluded from the present study.
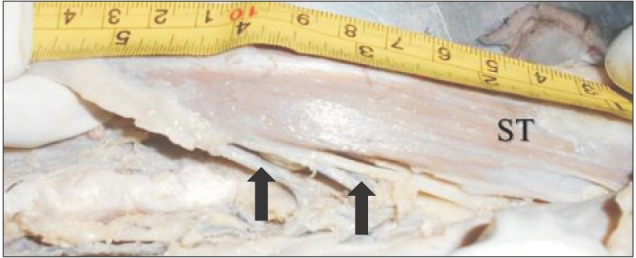
The length of the ST muscle belly and its tendon were measured as separate. The length of the muscle belly (AB) was measured at the midpoint from its origin from the ischial tuberosity (A) until its transition (B) as the tendon (Fig. 1). This measurement was performed by using a measuring tape. The length of the tendon of the ST muscle (BC) was measured at the midpoint from its transition zone as tendon (B) until its insertion into the supero-medial surface (C) of the tibia at the pes anserinus formation (Fig. 1). This tendon length measurement was performed by using the cotton thread. The measurements were taken at the midpoint as the border between ST muscle belly and its tendon was obscured. The diameter of neurovascular pedicle was measured by using the digital Vernier caliper (Mitutoyo Corporation, Kawasaki, Japan).
The number of neurovascular pedicles entering into the ST muscle (Fig. 2) were counted in each lower limb and distance of them from the origin of the ST muscle were measured. For the study purpose, the ST muscle was divided into 6 equal parts (50 mm each) to observe the site of entrance of neurovascular pedicle. This helped us to analyze the site of entrance of the neurovascular pedicle into the ST muscle. This measurement was performed by using the measuring tape. The data were tabulated (Table 1).
Each of the measurements were performed by three authors of the present study, to prevent the observer bias. The average of the three measurements were obtained and tabulated for the data analysis.
The length of the ST muscle belly and its tendon were tabulated separately for the right and left sides. The statistical comparison was performed by using the paired t test.
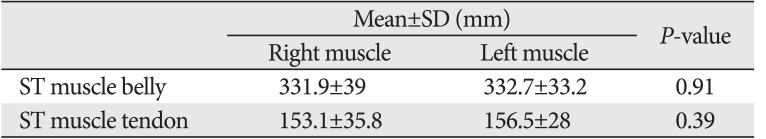
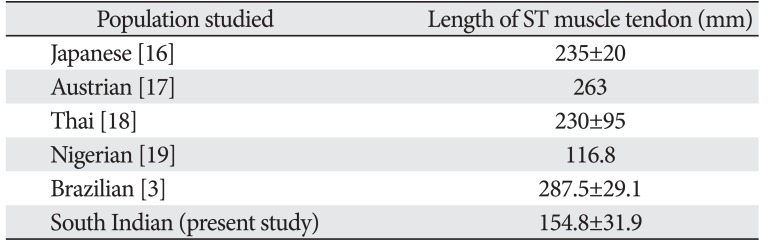
The present study observed that the border between the ST muscle belly and its tendon (transition zone) was obscured. The border was not transverse in morphology but it was oblique and serrated. The ST muscle belly measured 332.3±36.1 mm as its mean length and its tendon measured 154.8±31.9 mm (Table 1). The data are given in their frequency of range in Table 1.
The number of neurovascular pedicles of the ST muscle were ranging between 1 and 7. The frequency of number of neurovascular pedicles entering into the ST muscle are analyzed and represented in Fig. 3. The distance of the entry of neurovascular pedicle to the ST muscle from ischial tuberosity was ranging between 46 to 272 mm. The frequency of range of distance of neurovascular pedicles from the origin of ST muscle (from the ischial tuberosity) is being represented in Fig. 4. It was observed that the neurovascular pedicles were highest (31%) at the range of 151–200 mm away from the ischial tuberosity. They were least (2%) at the initial 1–50 mm and last 251–300 mm, from the origin of the muscle. The diameter of the neurovascular pedicle was ranging between 2 and 42 mm and the mean was 11.4±9.1 mm. This was at their entrance into the ST muscle.
The tendons of the medial hamstring muscles are used as a source for auto graft, in the reconstruction of anterior cruciate ligament of the knee joint [11]. The ST muscle tendon graft is known to give powerful strength, because of its length and it is more suitable to bridge the larger gaps [5]. It has been reported that the remaining portion of the ST muscle tendon regenerates after few years of harvesting the graft from it. Cross et al. [12] were the first to opine the higher chances of regenerative power of the ST muscle after its harvest. The microscopic appearance of regenerated tendon was same as that of the non-harvested ST muscle tendon on the contralateral limb [13]. It has also been radiologically observed, that the ST muscle tendon has a greater prospective to rejuvenation after its elimination [14]. The ST muscle tendon graft is preferred over the patellar tendon graft, because the harvesting of ST muscle tendon is easier with a tiny incision. There will be very minimal post-surgical pain at the graft donor area. There is very minimal discomfort at the movements of the knee joint and the long-term clinical results are excellent [15]. For the anterior cruciate ligament reconstruction, the ST muscle graft is usually tripled or quadrupled. This needs a graft of not only acceptable width, but also suitable length [4].
Reboonlap et al. [4] have reported that the ST muscle tendon graft length, which is required for the anterior cruciate ligament reconstruction ranges between 218 and 337 mm in Thai population. Since the graft length is proportional to the height of the person, it is advisable to prepare the graft with respect to the height of the person. The radiological investigations like computed tomography and nuclear magnetic resonance can be performed to forecast the length and diameter of the grafts, before the surgical procedure [3]. The mean length of the ST muscle tendons was 235±20 mm in a Japanese study [16]. It was reported that the tendon of ST muscle measured 263 mm in length, in a study performed from Austrian population [17]. The mean length of ST muscle tendon in a Brazilian study was 287.5±29.1 mm [3]. The length of ST muscle tendon in male and female were 243.3 and 218.9 mm, respectively, in a Thai population study performed by Limitlaohaphan et al. [18]. They opined that the leg length can be used to predict the graft length. The comparison of the length of the ST muscle tendon of the present study with the previous reports from other population groups is given in Table 3. The present investigation from South Indian population observed that, the mean length of the ST muscle tendon was 154.8±31.9 mm. This length of ST muscle tendon, ranged between 73 and 229 mm. This is lesser in comparison to the previous reports from Brazilian, Japanese, Austrian, and Thai populations (Table 3), but our data is similar to the measurement from Nigerian population (Table 3), in which the mean length of the ST muscle tendon was 116.8 mm [19]. We believe that the smaller length of the ST muscle tendon in the present study could be because of the racial variations and also because of the variation in the measurement performed. The previous authors [3161718] might have included the extension of the ST muscle insertion (pes anserinus at the superomedial part of the anterior surface of tibia) as well. We did not include this measurement, as we considered the pes anserinus as the conjoint tendon formed by sartorius, gracilis, and ST muscles. We clarify with the data of the present study that, pes anserinus cannot be included as the length of the tendon of ST muscle as it is a confluence of musculotendinous structures. The present study used the cotton thread for the measurement of the tendon of ST muscle, because the tendon was not straight and it was directed anteriorly. The previous authors used the Vernier caliper to measure the tendon of ST muscle. We believe that, these may be the reasons for the smaller dimension of the length of ST muscle tendon being observed in the present study in comparison to the previous reports.
The avulsion of the hamstring origin of ST muscle is a very rare injury and can happen in young athletes. It can cause significant amount of morbidity. In chronic cases, the primary repair may not be possible because of the retraction of muscle mass [20]. Muellner et al. [20] reported a novel operation procedure to reconstruction this type of chronic avulsion by using contralateral ST muscle autograft.
The neurovascular pedicles are of interest to the plastic and reconstructive surgery. Since the data are not available about the neurovascular pedicles of ST muscle, the present study was performed in South Indian population. The ST muscle is considered as the best, for the reconstructive surgery in comparison to the long head of biceps femoris due to its topography of vascular and nerve supply [21]. The ST muscle was used to reconstruct the anal sphincter since it has plenty of arterial and nerve supply [21]. It has been reported that any graft harvesting procedure involving the fleshy part of ST muscle should preserve its arterial supply [22]. The ST muscle receives its arterial supply through the medial circumflex femoral artery pedicles, near its origin and there are also pedicles given from the second perforating branch of the femoral artery. The ST muscle receives its nerve supply from the sciatic nerve as two motor branches [21]. These arteries and nerves together constituted the neurovascular pedicle in the present study. In a canine model study, it was observed that ST muscle can withstand its arterial supply from anyone of its neurovascular pedicles, which supports its possible clinical use as the muscle flap [23]. In another animal study, it was reported that the superior part of the ST muscle was considered as the best for transfer in the treatment of larger wounds as a pedicle flap [24]. The present study supports this opinion, because the neurovascular pedicles were more in number at the superior part of the ST muscle. Guelinckx et al. [25] reported that construction of a muscular cuff around the anal sphincter can task as a regular anal sphincter in patients suffering from fecal incontinence. This is possible because of the better neurovascular pedicle of the ST muscle.
Advanced surgical techniques like microsurgery have led to the complex, compound and composite pedicle flap procedures. Because of the novel and rapidly evolving era of the perforator flaps, there is no perfectness about the terminology and nomenclature, which creates a lot of confusion in the surgical literature [26]. In this context, the present study aimed to observe the morphology of the entrance of the neurovascular pedicles into the ST muscle. These findings are being hypothesized to give topographical idea to the operating surgeon about the exact location of nerve and artery entering into the ST muscle.
The present study observed that, 48% of the ST muscles have solitary neurovascular pedicle and 32% had double neurovascular pedicles. The neurovascular pedicles were highest (31%) at the distance of range of 151–200 mm away from the ischial tuberosity. The pedicles were few (2%) in the initial 1–50 mm from the origin of the muscle and in the terminal 251–300 mm of the muscle. It was obvious that the neurovascular pedicles were distributed all over the muscle, however their number were less near the origin of the muscle and also at the transition zone near the beginning of its tendon. So, the pedicle flap can be taken from any location of ST muscle other than these terminal end parts.
We believe that the present study has provided the novel data about the diameter of the neurovascular pedicles entering the ST muscle. This diameter is important to the arthroscopic surgeon, because ST pedicle flaps are used as a graft, during the anterior cruciate ligament reconstruction. The present investigation reported the mean length of the ST muscle belly from South Indian population. The ST muscle tendon length was also documented in this study, and the topographical distribution of neurovascular pedicles of the ST muscle was studied. The present study involved the measurement of the distance of the neurovascular pedicle from the origin of the muscle. The topography of the entry of neurovascular pedicles into the ST muscle is clinically important. For the study purpose, the ST muscle was divided into 6 equal parts (50 mm each) to observe the site of entry of pedicle.
It is believed that the morphometric data reported in the present investigation will be helpful to the orthopedic and plastic surgeons. The data have implications during the harvesting of grafts and pedicle flaps. The data are imperative to the orthopedician, during the surgical procedures like anterior cruciate ligament and Achilles tendon reconstruction.
The data about the ST muscle were not available from South Indian population and this manuscript provides the novel information. We believe that the morphometric and topographical data of the present study can be used as an anthropological database of the ST muscle of South Indian population. This data can be used for global comparison across the world. The present study provides the diameter of neurovascular pedicles entering the ST muscle, which is being reported for the first time and considered as a novel data. This is important to the arthroscopic surgeon during the anterior cruciate ligament reconstruction. It was observed that the pedicles were few in number near the origin of the ST muscle and at the transition as tendon. This knowledge about the neurovascular pedicles is enlightening to the plastic surgeon.
Acknowledgements
The authors of the present study would like to convey their deep sense of gratitude to all the non-teaching staff members of their department for the help presented while carrying out this analysis.
References
1. Moore KL, Dalley AF, Agur AM. Clinically oriented anatomy. 5th ed. Baltimore, MD: Lippincott Williams and Wilkins;2006. p. 616–617.
2. Lee JH, Kim KJ, Jeong YG, Lee NS, Han SY, Lee CG, Kim KY, Han SH. Pes anserinus and anserine bursa: anatomical study. Anat Cell Biol. 2014; 47:127–131. PMID: 24987549.
3. Pereira RN, Karam FC, Schwanke RL, Millman R, Foletto ZM, Schwanke CH. Correlation between anthropometric data and length and thickness of the tendons of the semitendinosus and gracilis muscles used for grafts in reconstruction of the anterior cruciate ligament. Rev Bras Ortop. 2016; 51:175–180. PMID: 27069886.
4. Reboonlap N, Nakornchai C, Charakorn K. Correlation between the length of gracilis and semitendinosus tendon and physical parameters in Thai males. J Med Assoc Thai. 2012; 95(Suppl 10):S142–S146.
5. Maffulli N, Longo UG, Gougoulias N, Denaro V. Ipsilateral free semitendinosus tendon graft transfer for reconstruction of chronic tears of the Achilles tendon. BMC Musculoskelet Disord. 2008; 9:100. PMID: 18611249.
6. Hua Y, Chen S, Jin Y, Zhang B, Li Y, Li H. Anatomical reconstruction of the lateral ligaments of the ankle with semitendinosus allograft. Int Orthop. 2012; 36:2027–2031. PMID: 22722541.
7. Biau DJ, Tournoux C, Katsahian S, Schranz PJ, Nizard RS. Bone-patellar tendon-bone autografts versus hamstring autografts for reconstruction of anterior cruciate ligament: meta-analysis. BMJ. 2006; 332:995–1001. PMID: 16603564.
8. Prodromos CC, Han YS, Keller BL, Bolyard RJ. Stability results of hamstring anterior cruciate ligament reconstruction at 2- to 8-year follow-up. Arthroscopy. 2005; 21:138–146. PMID: 15689861.
9. Azar FM, Beaty JH, Canale ST. Campbell's operative orthopaedics. 13th ed. Philadelphia, PA: Elsevier;2017. p. 41–45.
10. de Lima Lopes C, Arantes G, de Oliveira RV, Pinto DM, Gonçalves MC, Gonçalves RC. Anatomical reference point for harvesting a flexor graft during arthroscopic reconstruction of the anterior cruciate ligament. Rev Bras Ortop. 2015; 50:164–167. PMID: 26229911.
11. Tabuchi K, Soejima T, Murakami H, Noguchi K, Shiba N, Nagata K. Inducement of tissue regeneration of harvested hamstring tendons in a rabbit model. Bone Joint Res. 2016; 5:247–252. PMID: 27340141.
12. Cross MJ, Roger G, Kujawa P, Anderson IF. Regeneration of the semitendinosus and gracilis tendons following their transection for repair of the anterior cruciate ligament. Am J Sports Med. 1992; 20:221–223. PMID: 1558254.
13. Åhlén M, Lidén M, Movin T, Papadogiannakis N, Rostgård-Christensen L, Kartus J. Histological evaluation of regenerated semitendinosus tendon a minimum of 6 years after harvest for anterior cruciate ligament reconstruction. Orthop J Sports Med. 2014; 2:2325967114550274. PMID: 26535362.
14. Eriksson K, Hamberg P, Jansson E, Larsson H, Shalabi A, Wredmark T. Semitendinosus muscle in anterior cruciate ligament surgery: morphology and function. Arthroscopy. 2001; 17:808–817. PMID: 11600977.
15. Charalambous CP, Kwaees TA. Anatomical considerations in hamstring tendon harvesting for anterior cruciate ligament reconstruction. Muscles Ligaments Tendons J. 2012; 2:253–257. PMID: 23738306.
16. Tohyama H, Beynnon BD, Johnson RJ, Nichols CE, Renström PA. Morphometry of the semitendinosus and gracilis tendons with application to anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1993; 1:143–147. PMID: 8536018.
17. Pichler W, Tesch NP, Schwantzer G, Fronhöfer G, Boldin C, Hausleitner L, Grechenig W. Differences in length and cross-section of semitendinosus and gracilis tendons and their effect on anterior cruciate ligament reconstruction: a cadaver study. J Bone Joint Surg Br. 2008; 90:516–519. PMID: 18378932.
18. Limitlaohaphan C, Kijkunasatian C, Saitongdee P. Length of semitendinosus and gracilis tendons and the relationship of graft length and leg length. J Med Assoc Thai. 2009; 92(Suppl 6):S200–S203. PMID: 20120686.
19. Ashaolu JO, Osinuga TS, Ukwenya VO, Makinde EO, Adekanmbi AJ. Pes anserinus structural framework and constituting tendons are grossly aberrant in Nigerian population. Anat Res Int. 2015; 2015:483186. PMID: 26246910.
20. Muellner T, Kumar S, Singla A. Proximal hamstring reconstruction using semitendinosus and gracilis autograft: a novel technique. Knee Surg Sports Traumatol Arthrosc. 2017; 25:112–114. PMID: 27826636.
21. Rab M, Mader N, Kamolz LP, Hausner T, Gruber H, Girsch W. Basic anatomical investigation of semitendinosus and the long head of biceps femoris muscle for their possible use in electrically stimulated neosphincter formation. Surg Radiol Anat. 1997; 19:287–291. PMID: 9413073.
22. Rouffet F, Honnart F, Calmat A. The blood supply of the semitendinosus, gracilis and sartorius muscles and surgical applications (author's transl). J Chir (Paris). 1977; 114:193–199. PMID: 925107.
23. Solano M, Purinton PT, Chambers JN, Munnell JF. Effects of vascular pedicle ligation on blood flow in canine semitendinosus muscle. Am J Vet Res. 1995; 56:731–735. PMID: 7653880.
24. Chambers JN, Purinton PT, Allen SW, Moore JL. Identification and anatomic categorization of the vascular patterns to the pelvic limb muscles of dogs. Am J Vet Res. 1990; 51:305–313. PMID: 2301845.
25. Guelinckx PJ, Sinsel NK, Gruwez JA, Lammens M, Bourgeois I Jr. Neurovascular intact muscle transposition for anal sphincter repair: experimental model and experience with dynamic pacing. Dis Colon Rectum. 1995; 38:878–885. PMID: 7634983.
26. Blondeel PN, Van Landuyt KH, Monstrey SJ, Hamdi M, Matton GE, Allen RJ, Dupin C, Feller AM, Koshima I, Kostakoglu N, Wei FC. The “Gent” consensus on perforator flap terminology: preliminary definitions. Plast Reconstr Surg. 2003; 112:1378–1383. PMID: 14504524.
Fig. 1
Measurements performed in the present study (AB, length of semitendinosus [ST] muscle belly; BC, length of semitendinosus muscle tendon). The border between the ST muscle belly and its tendon (point B in this picture) was oblique in morphology and serrated.
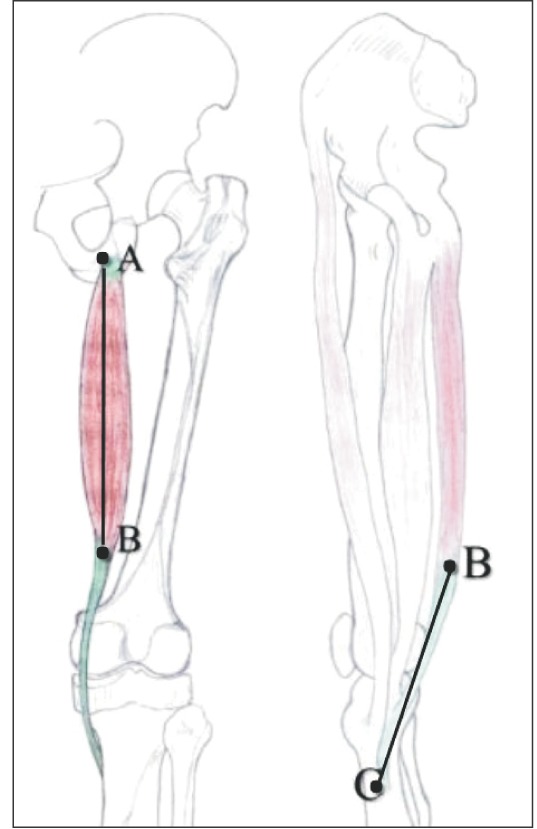
Fig. 3
Frequency of number of neurovascular pedicles entering into the semitendinosus muscle (n=46).
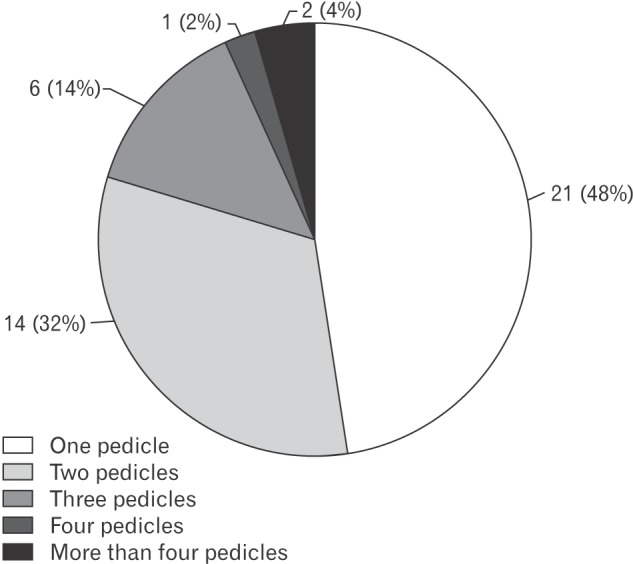
Fig. 4
Frequency of distance of neurovascular pedicles entering into the semitendinosus muscle from the ischial tuberosity.
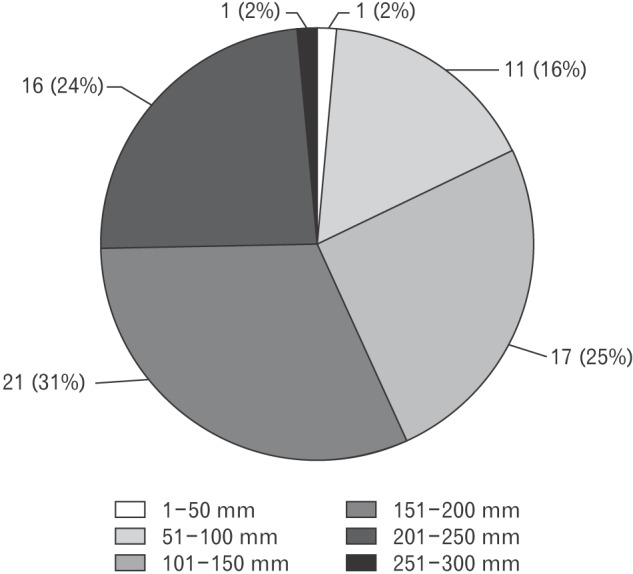
Table 1
Morphometric data obtained in the present study
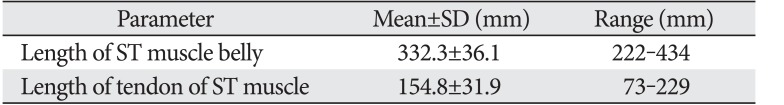
| Parameter | Mean±SD (mm) | Range (mm) |
|---|---|---|
| Length of ST muscle belly | 332.3±36.1 | 222–434 |
| Length of tendon of ST muscle | 154.8±31.9 | 73–229 |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download