Abstract
The majority of malignant melanomas in the small intestine are metastases from primary cutaneous lesions, it can also develop as a primary mucosal tumor in the gastrointestinal tract. In this report, we present rare cases of primary small bowel melanoma and review the current literature. A 78-year-old male presented with abdominal pain and CT enterography identified a ileal mass. A 79-year-old female presented with signs and symptoms of partial small bowel obstruction. Abdominopelvic CT and small bowel series revealed a obstructing mass in the distal jejunum. The masses were confirmed on laparotomy and histologically diagnosed as melanoma. Extensive postoperative clinical examination revealed no cutaneous lesions. A primary small bowel melanoma is an extremely rare neoplasm. A definite diagnosis can only be made after a thorough investigation has been made to exclude the coexistence of a primary lesion. Curative resection of the tumor remains the treatment of choice.
The majority of malignant melanomas in the small intestine are metastases from primary cutaneous lesions, it can also develop as a primary mucosal tumor in the gastrointestinal (GI) tract [1]. Distinguishing metastatic melanoma of the GI tract from primary melanomas and other primary lesions can be very challenging. We here in report 2 rare cases of primary malignant melanoma of the small intestine. Furthermore, we review the relevant literature for diagnosis and treatment.
The study protocol was approved by the Institutional Review Board of Asan Medical Center (approval number: S2017-2218-0001), in accordance with the Declaration of Helsinki.
A 78-year-old male was admitted to our department with abdominal pain, nausea, generalized edema, and fever for 1 month. His medical history revealed no prior evidence of malignant melanoma. CT enterography performed because of repeated colicky abdominal pain and nausea revealed the presence of a solid tumor possibly originating in the distal ileum. Whole body PET-CT showed a hypermetabolic mass in the pelvic ileal loop; however, there was no indication of cutaneous, retinal, or anal primary lesions.
Exploratory laparotomy revealed an intraluminal mass in the distal ileum. Careful examination of the abdominal cavity revealed no macroscopic evidence of metastases. Small bowel resection was performed with side-to-side anastomosis. The postoperative course was uneventful, and the patient was discharged on postoperative day 6.
Surgical specimen was 22 cm in length and included a 9.2 × 5.5-cm mass (Fig. 1). The resection margins and retrieved 7 lymph nodes were free from tumor invasion. Immunohistochemistry revealed the presence of tumor cells that were positive for the melanoma markers such as Melan-A, HMB45, S100 protein, and SOX10 (Fig. 2).
After the diagnosis of melanoma was established, the patient underwent a clinical and laboratory evaluation. The examination of skin, eyes, esophagus, and anus was negative for primary melanoma and the investigation with chest CT, brain MRI, and PET-CT scan did not report metastatic disease. Therefore, the resected lesion was determined to be a primary melanoma of the small intestine. The patient was scheduled for follow-up at regular intervals every 3 months for the 1st year and every 6 months for up to 5 years. At each follow-up, physical examination and an abdominopelvic CT scan was obtained. Chest X-ray or chest CT was performed alternately every 6 months. During 1 year of regular follow-up, there was no recurrence or metastases. No adjuvant or alternative therapy was used.
A 79-year-old female presented with signs and symptoms of partial small bowel obstruction. The patient had undergone abdominoperineal resection for rectal cancer 11 years earlier. At the time, the tumor was pathologically staged as pT2N0M0, and she was free from recurrent disease. Abdominopelvic CT and small bowel series revealed the presence of a partially obstructing mass in the distal jejunum with several subcentimeter mesenteric lymph nodes. PET-CT, chest CT, and colonoscopy demonstrated no evidence of melanoma at other sites or metastases.
Exploratory laparotomy confirmed the presence of a distal jejunal tumor (Fig. 1) with no intra-abdominal metastases. The patient underwent segmental resection of the small bowel with end-to-end anastomosis. Immunohistochemistry of tissue biopsy specimens revealed positive staining for S100 protein, Melan-A, and HMB45. Further pathologic assessment identified metastatic cancer cells in four out of seven mesenteric lymph nodes.
The postoperative course was uneventful, and the patient was discharged on postoperative day 6. No adjuvant therapy was used. The patient died 7 months after surgery due to recurrent melanoma.
Primary mucosal melanoma can arise at any site within the GI mucosa, but it is most common in anorectal (anal canal, 31.4%; rectum, 22.2%) and oropharyngeal (32.8%) regions, whereas esophagus (5.9%), stomach (2.7%), small intestine (2.3%), gallbladder (1.4%), and large intestine (0.9%) are extremely rare sites of origin [2].
Presence of melanocytes has not yet been demonstrated in the small intestine, and the origin of primary melanoma of the small intestine remains unknown. One potential origin of the primary melanoma of small intestine is melanoblastic cells of the neural crest that migrate to the distal ileum through the omphalomesenteric canal. Accordingly, the ileum, which represents the distal end of the omphalomesenteric canal, should be the most common site of primary malignant melanoma within the small intestine [3]. Another hypothesis was that these tumors originate from enteric neuroendocrine noncutaneous tissue in the form of amine precursor uptake decarboxylase cells that have undergone neoplastic transformation. This would also account for the remaining nonileal intestinal malignant melanomas [3] .
Some authors question the existence of primary melanoma of the small intestine, suggesting that all melanomas in the small intestine are metastases from unknown or regressed primary cutaneous melanoma [1]. A clear distinction between primary intestinal melanoma and intestinal metastatic deposits can be difficult when the diagnosis is considered based on histopathological features alone. The clinical importance of this distinction lies within the differential in prognosis. Prognosis is worse for primary intestinal melanomas which tend to grow faster and more aggressively. A primary GI mucosal melanoma is considered in patients with no obvious primary cutaneous melanoma or those with an isolated GI lesion in the absence of other extraintestinal metastases. Blecker et al. [1] suggested the following criteria for the diagnosis of primary intestinal melanoma: no evidence of concurrent melanoma or atypical melanocytic lesion of the skin, absence of extraintestinal metastatic spread of melanoma, and presence of intramucosal lesions in the overlying or adjacent intestinal epithelium.
Primary intestinal melanoma tends to be more aggressive and is associated with worse prognosis than cutaneous melanoma. Cheung et al. [2] reported that the mean age at the time of diagnosis of primary GI melanoma was 54 years and that 75% had mesenteric lymph node metastases. They also showed that the prognosis of melanoma of the small intestine was poor, with a median survival of 16 months. Another study showed that the 1-year survival post resection was only 50% (8 of 16 cases), with half of the operated patients dying within a year of surgery, as a result of tumor recurrence [4]. This may be in part due to the very low rate of early diagnosis of mucosal melanomas, particularly those of the GI tract. In addition to aggressive tumor behavior, poor outcomes result from late diagnosis and fast tumor growth supported by the rich vascular and lymphatic supply of the intestinal mucosa.
Because of rare cases and worse prognosis, it is difficult to assess the prognostic factors in patients with primary malignant melanoma of small intestine. In the study of Cheung et al. [2] which included 659 primary melanomas of whole GI mucosa location of tumor, advanced tumor stage, failure to undertake surgical resection, positive lymph node status, and age have been found to be independent predictors of poorer outcome. However, in that study, small bowel melanoma was included only 15 cases (2.3%). In our cases, the patient with node metastasis showed worse prognosis than the patient without node metastasis. Furthermore, the relevant data from Table 1 in our study showed that 5 of 11 patients (45%) had lymph node metastasis, and they seemed to have a worse prognosis. However, a large scale multicenter data collection and analysis is necessary to elucidate this assumption.
Surgery is the main treatment option for primary melanoma of the small intestine and should include excision of the intestine with tumor-free margins and of mesentery to remove regional lymph nodes. In these patients, systemic adjuvant therapy has a limited role, and chemotherapy regimens have very low response rates [3]. Recently, some articles reported that immune checkpoint inhibitor (PD-1 antibody and/or CTLA-4 antibody) provides unprecedented efficacy gains in metastatic or advanced melanoma [5]. However, the effect of immunotherapy as an adjuvant treatment on musosal melanoma has not been proved yet.
In conclusion, primary intestinal malignant melanoma is an unusual tumor of the small intestine. Therefore, definitive diagnosis can only be established after thorough investigation to exclude the coexistence of a primary lesion elsewhere. Complete surgical resection of the intestinal lesions may be associated with improved outcomes and the patients who had lymph node metastasis seemed to have a worse prognosis.
Figures and Tables
Fig. 1
Surgical specimen (A, case 1; C, case 2) and macroscopic image of the tumor cut in half (B, case 1; D, case 2).

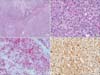
Fig. 2
Histologic feature of malignant melanoma. (A) The lesion shows diffuse atypical cells infiltration forming solid sheet (H&E, ×40). (B) The cells are medium-to large-sized with irregular nuclear contours, macronucleoli, and numerous mitotic activities (×400). Immunohistochemical staining showed that the malignant cells were strongly positive for Melan A (C) and S100 (D) (×200).
References
1. Blecker D, Abraham S, Furth EE, Kochman ML. Melanoma in the gastrointestinal tract. Am J Gastroenterol. 1999; 94:3427–3433.

2. Cheung MC, Perez EA, Molina MA, Jin X, Gutierrez JC, Franceschi D, et al. Defining the role of surgery for primary gastrointestinal tract melanoma. J Gastrointest Surg. 2008; 12:731–738.

3. Lens M, Bataille V, Krivokapic Z. Melanoma of the small intestine. Lancet Oncol. 2009; 10:516–521.

4. Hadjinic ol, Hadji t, Athanasopoulos PG, Shah R, Ala AA. Primary small bowel melanomas: fact or myth? Ann Transl Med. 2016; 4:113.
5. Byrne EH, Fisher DE. Immune and molecular correlates in melanoma treated with immune checkpoint blockade. Cancer. 2017; 123(S11):2143–2153.

6. Spiridakis KG, Polichronaki EE, Sfakianakis EE, Flamourakis ME, Margetousakis TH, Xekalou AS, et al. Primary small bowel melanoma. A case report and a review of the literature. G Chir. 2015; 36:128–132.

7. Manouras A, Genetzakis M, Lagoudianakis E, Markogiannakis H, Papadima A, Kafiri G, et al. Malignant gastrointestinal melanomas of unknown origin: should it be considered primary? World J Gastroenterol. 2007; 13:4027–4029.

8. Timmers TK, Schadd EM, Monkelbaan JF, Meij V. Survival after resection of a primary malignant melanoma of the small intestine in a young patient: report of a case. Case Rep Gastroenterol. 2013; 7:251–260.

9. Khosrowshahi E, Horvath W. Primary malignant melanoma of the small intestine--a case report. Rontgenpraxis. 2002; 54:220–223.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download