Abstract
Purpose
Increasing surgical expertise in minimally invasive surgery has allowed laparoscopic surgery to be performed in many abdominal surgeries. Laparoscopic choledochal cyst excision and Roux-en-Y hepaticojejunostomy are challenging and sophisticated surgeries because of the difficult anastomosis. Recent advances in robotic surgery have enabled more delicate and precise movements, and Endowrist instruments allow for securing sutures during anastomosis. This study aimed to compare surgical outcomes of laparoscopic and robotic hepaticojejunostomy in choledochal cyst excision.
Methods
Sixty-seven patients who underwent laparoscopic or robotic-hybrid choledochal cyst excision from 2004 to 2016 were retrospectively analyzed and compared. In robotic surgery, dissection was performed laparoscopically, and hepaticojejunostomy was performed using a robotic platform.
Results
The mean operative time was significantly longer in robotic surgery than in laparoscopic surgery (247.94 ± 54.14 minutes vs. 181.31 ± 43.06 minutes, P < 0.05). The mean estimated blood loss (108.71 ± 15.53 mL vs. 172.78 ± 117.46 mL, respectively, P = 0.097) and postoperative hospital stay (7.33 ± 2.96 days vs. 6.22 ± 1.06 days, P = 0.128) were comparable between procedures. Compared to the laparoscopic approaches, robotic surgery had significantly less short-term complications (22.4% vs. 0%, P = 0.029). There were more biliary leakage (n = 7, 14.3%) observed during the first 30 days after surgery in laparoscopy while none were observed in the robotic method.
Choledochal cyst is a rare congenital dilatation of the biliary system and it commonly affects the Asian population [1]. Choledochal cyst is mostly diagnosed in the first decade of life. However, because of an increased amount of routine health checkups and advancement of noninvasive hepatobiliary imaging, diagnosis of choledochal cyst in adults has increased. Choledochal cysts are known to be benign. However, the cyst must be excised because of the high risk of developing associated malignancy, such as cholangiocarcinoma, choledocholithiasis, cholangitis, and pancreatitis [23]. Therefore, the current treatment of choice in choledochal cyst is complete cyst excision with Roux-en-Y hepaticojejunostomy anastomosis.
Increasing knowledge and surgical expertise in the era of laparoscopic abdominal surgery has allowed more sophisticated surgery, such as hepaticojejunostomy, to be performed under laparoscopy. Many studies have reported performing laparoscopic choledochal cyst excision and Roux-en-Y hepaticojejunostomy [456789101112]. Although laparoscopy enables magnified surgical views, thereby increasing precision in dissection and anastomosis, reducing tissue injury, and providing excellent cosmetic outcomes, there are inevitable limitations to this approach. Instruments that are used for this technique are rigid with limited degrees of freedom that hinder tension-free suturing. Therefore, the da Vinci Surgical System (Intuitive Surgical, Sunnyvale, CA, USA) is utilized to combine the benefits of laparoscopic and robotic surgery. In the robotic surgery, besides the tremor reducing effect of the robotic platform, precise maneuvers along with the wristed instruments allow for more delicate and secure sutures. Such advantages are especially prominent when performing an anastomosis to small tubular structures such as a small bile duct. Accordingly, robotic surgery is preferred in performing surgeries that require multiple sutures such as during an anastomosis and especially in a particularly small anastomosis. On the other hand, laparoscopic surgery allows a variety of instruments, a wider range of motion, and wider surgical field of view [1314] during dissection of the choledochal cyst.
This study aimed to compare the surgical outcomes between laparoscopic and robotic-hybrid choledochal cyst excision with Roux-en-Y hepaticojejunostomy.
We performed a retrospective analysis of patients who underwent laparoscopic or robotic-hybrid choledochal cyst excision and Roux-en-Y hepaticojejunostomy at the Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, Seoul National University Hospital from 2004 to 2016. All of the patients who were diagnosed with choledochal cyst who underwent laparoscopic or robotic surgery were included. Two patients who were diagnosed with early gallbladder cancer, and laparoscopic cholecystectomy was performed with choledochal cyst excision, were also included. Cases of combined liver resections were excluded.
Pancreatobiliary protocol CT, MRI, or endoscopic retrograde cholangiopancreatography was performed to evaluate the extent of choledochal cyst involvement, anomalous pancreatobiliary ductal union (APBDU), associated biliary stones, or malignancy, and to determine the extent of surgery.
This study has been approved by the Institutional Review Board of the Seoul National University Hospital (approval no. 1610-012-797).
Laparoscopic choledochal cyst excision has been described in previous reports [57]. The position of patients, port placement, cyst dissection and resection, and Roux-en-Y hepaticojejunostomy were performed as previously described [57].
In robotic-hybrid choledochal cyst excision, three 12-mm and two 8-mm trocars were inserted at the lower abdomen. A 5-mm trocar was inserted at the epigastrium if needed for laparoscopic use (Fig. 1). Laparoscopic dissection was performed first and the robotic platform was used in the hepaticojejunostomy anastomosis. First, calot's triangle was exposed and dissected. Once the cystic duct was identified, the hepatoduodenal ligament was dissected first along the right choledochal cyst margin, followed by the supraduodenal margin. The duodenum was retracted downwards for better exposure. Retroduodenal and intrapancreatic portions of the choledochal cyst were further dissected until the transitional area was sufficiently exposed. The distal end of the dilated bile duct was transected with an endo-GIA (Covidien, Norwalk, CT, USA). Using the distal stump of the cyst as a retractor, further upwards, medial and posterior dissection was performed until the hepatic ducts were observed. The bile duct was dissected until just below the hilum and transected, and the cystic duct was ligated and divided using clips.
After excision of the cyst, retrocolic Roux-en-Y hepaticojejunostomy was performed. After placing tagging sutures at both sides of the jejunum, it was transected using an endo-GIA 40 cm distally from the Treitz ligament. The jejunum, 70 cm distal from the hepaticojejunostomy, was then tagged with a suture for jejunojejunostomy to be performed at a later time. The Roux limb was brought up to the hilum for anastomosis and a robotic platform was prepared and docked. Once docking was finished, using the robotic system, interrupted sutures with 1- to 2-mm intervals from the previous suture were placed using 4-0 Vicryl (Ethicon, Somerville, NJ, USA) sutures at the posterior and anterior walls. Cholecystectomy was performed after anastomosis because it provides liver retraction during anastomosis. The gallbladder and excised choledochal cyst were placed into a LapBag (Sejong Co., Paju, Korea) and were extracted at the camera port. The tagged jejunum was also brought out for extracorporeal jejunojejunostomy after extending 1 cm of the camera port site.
Once all of the procedures were performed, a Jackson-Pratt drain was inserted through the right port and placed near the hepaticojejunostomy.
Patients usually started a liquid diet on postoperative day 1. Jackson-Pratt drains were removed if CT scans that were performed on postoperative day 4 showed no evidence of abnormal fluid collection. Patients revisited the outpatient department 2 weeks after discharge and were followed up at 3 months to monitor postoperative complications. If there were no complications, the patients were followed up every 12??8 months. For follow-up, a routine complete blood count, liver function test, measurement of tumor markers, including carcinoembryonic antigen and carbohydrate-associated antigen 19-9, and CT or MRI were performed to evaluate complications, such as pancreatitis, cholangitis, choledocholithiasis, or malignancy.
A total of 49 patients (73.1%) underwent laparoscopic surgery since 2004 and 18 patients (26.9%) underwent robotic surgery since 2015. In the laparoscopic group, 6 patients (12.2%) were male and 43 (87.8%) were female. The mean age was 36.57 ± 10.84 years and the mean body mass index was 21.38 ± 2.98 kg/m2. Nineteen (38.8%), 3 (6.1%), and 11 patients (15.4%) were diagnosed with Todani classification type Ia, Ib, and Ic, respectively, while 16 (32.7%) were diagnosed with type IVa. Forty patients (81.6%) were associated with APBDU and 9 patients (18.4%) had associated biliary tract stones. With regard to histopathology, 2 patients (4.1%) had dysplasia and 2 patients (4.1%) had biliary intraepithelial neoplasia. One patient (2.0%) was diagnosed with pT2N0M0, stage II gallbladder cancer according to the American Joint Committee of Cancer, 7th edition (Table 1).
In contrast, in the robotic-hybrid group, all of the patients were female. The mean age was 36.17 ± 13.33 years and the mean body mass index was 20.94 ± 2.10 kg/m2. Four (22.2%) and 10 patients (55.6%) were diagnosed with Todani classification types Ia and Ic, respectively. Furthermore, 3 patients (16.7%) were diagnosed with type IVa and 1 patient (5.6%) was diagnosed with type IVb. All patients were associated with APBDU and only 1 patient (5.6%) had biliary tract stones. In histopathology, 2 patients (11.1%) had dysplasia and 1 (5.6%) had biliary intraepithelial neoplasia. Moreover, 1 patient (5.6%) was diagnosed with pT2N0M0, stage II gallbladder cancer.
The mean operative time was significantly shorter in the laparoscopic group than in the robotic-hybrid group (181.31 ± 43.06 minutes vs. 247.94 ± 54.14 minutes, P < 0.05). The mean estimated blood loss was not significantly different between the laparoscopic and robotic-hybrid groups (108.71 ± 15.53 mL vs. 172.78 ± 117.46 mL, P = 0.097). Furthermore, the mean postoperative hospital stay was not significantly different between the laparoscopic and robotic-hybrid groups (7.33 ± 2.96 days vs. 6.22 ± 1.06 days, P = 0.128). There was no open conversion in all laparoscopic and robotic surgeries (Table 2).
Short-term surgical complications were defined as complications within 30 days of surgery. A total of 11 complications (22.4%) in the laparoscopic group were observed. There was 1 case (2.0%) of bleeding that required exploration, 1 case (2.0%) of fluid collection, 7 cases (14.3%) of bile leakage, 1 case (2.0%) of postoperative ileus, and 1 case (2.0%) of wound complications. Compared to the laparoscopic approach, there was no complications observed in the robotic-hybrid group. Complications rate was significantly higher in the laparoscopic group regarding short-term complications compared to the robotichybrid group (P = 0.029) (Table 3).
Long-term surgical complications, which occurred 30 days after surgery, were observed in 7 patients (14.3%) in the laparoscopic group. Three patients (6.1%) had a hepatic duct stone postoperatively and 1 patient (2.0%) underwent intervention because of hepaticojejunostomy stricture. Additionally, 1 patient (2.0%) was treated for postoperative adhesive ileus. Only 2 patients (22.2%) in the robotic-hybrid group had longterm complications, such as delayed fluid collection (5.6%) or adhesive ileus (5.6%). No significant difference in long-term complications was observed between the two groups (P > 0.999) (Table 3).
With regard to overall surgical complications, laparoscopic choledochal cyst excision tended to have more complications compared with robotic surgery. Compared to the laparoscopic group, patients who underwent robotic surgery had significantly decreased biliary tract-specific complications (P = 0.029). There were 7 cases (14.3%) of bile leakage with five patients experiencing grade A, transient bile leakage while 2 patients were of grade B bile leakage requiring radiologic interventions. Furthermore, 3 patients (6.1%) had hepatic duct stones while hepaticojejunostomy stricture was observed in 1 patient (2.0%). There was no biliary tract-specific complications observed in the robotic-hybrid group (Table 4).
Choledochal cyst is a rare congenital anomaly of the biliary system that commonly affects the Asian population [1]. The estimated incidence of choledochal cyst and APBDU is 0.3% and 4.1%, respectively, according to a large, multicenter study [2]. The clinical presentation of choledochal cyst differs from children to adults. In adults, this disease entity can manifest cholangitis, pancreatitis, choledocholithiasis, or biliary malignancy, such as cholangiocarcinoma or gallbladder cancer [2]. Complete excision of the cyst is mandatory because of the risk of developing complications or malignancies.
With growing interest in cosmetics, laparoscopic approaches in hepatobiliary surgery have become inevitable. Laparoscopic hepaticojejunostomy anastomosis still remains one of the most sophisticated and challenging surgeries to date [15]. Since the first report of laparoscopic choledochal cyst excision in 1995 [16], studies regarding this approach have reported that laparoscopic surgery is safe and feasible in the treatment of choledochal cysts. However, complications related to hepaticojejunostomy have been reported [781011]. Therefore, robotic-assisted intracorporeal anastomosis has been investigated to overcome such issues.
Laparoscopic approaches provide magnified surgical views, allowing precise dissection and anastomosis, reduced tissue injury, and better cosmetic outcomes. However, rigid instruments with limited degrees of freedom, a fulcrum effect, and 2-dimensional vision lead to poor ergonomic positions of surgeons, thereby hindering delicate sutures during anastomosis. The robotic platform has been developed to overcome many of the limitations faced during laparoscopic surgeries, such as instruments with wrists that provide more degrees of freedom. These instruments increase range of motion and 3-dimensional high-definition vision, providing better depth perception. Such attributes have increased the dexterity and precision in complex techniques, including intracorporeal sutures, which are important maneuvers in performing hepaticojejunostomy after cyst excision [1517181920].
Although total robotic surgery can be performed, we performed the dissection under laparoscopy and anastomosis under robotic approaches for several reasons. Compared with the robotic platform, laparoscopy allows for faster surgical maneuvers with a variety of different instruments. Additionally, range of motion is wider in laparoscopy providing better surgical performance in bowel preparation for anastomosis. Furthermore, laparoscopic surgery enables a change in position during surgery, while such change is limited in robotic surgery once docking is finished. Moreover, changes in instruments are rapidly performed, thereby reducing surgical times. There are also practical issues in cases where open conversion is required and where the patient and institute experience more economic loss compared with laparoscopic surgery. In contrast, robotic surgery allows for fine movement and wristed instruments are suitable for sutures in anastomosis. Therefore, robotic-hybrid choledochal cyst excision and Roux-en-Y hepaticojejunostomy was performed to integrate the advantages of laparoscopic and robotic surgery.
Biliary tract-specific complication rates were significantly higher in patients who underwent laparoscopic surgery (P = 0.029). There were 7 cases (14.3%) of postoperative biliary leakage after laparoscopic surgery while none were observed after robotic surgery. Although postoperative biliary leakage after laparoscopic surgery were all grade A, transient biliary leakage, none were observed in the robotic approach implies that technical sophistication differs between the 2 different approaches and that robotic surgery is more advantageous when performing intracorporeal sutures. As reported in many studies and according to our early initial experience, robotic sutures are more precise and easier to handle, thereby providing secure sutures, compared with laparoscopic sutures [151719]. Compared with laparoscopic instruments, the wristed instruments of the robotic platform enable more elaborate and subtle sutures that further secure anastomosis. We believe that through this robotic approach along with the precision and delicacy seen in performing hepaticojejunostomy is the mainstay of maintaining a secure anastomosis.
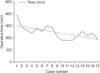
In this comparative study between laparoscopic and robotic surgery, there were no significant differences in clinicopathology, operative findings, and complications, except for operative time. This finding can be explained by the prolonged operative times when robotic platforms were first introduced. Docking times were lengthy and assistants were unfamiliar with surgical instruments that were used in this relatively new technique. However, as time progressed, the operators and robotic assistants became accustomed to instruments and procedures, and docking times have been shortened to the point where docking times rarely contribute to the overall operative time. The total operative time has decreased from 260 minutes in the early set-up of robotic surgery to 180 minutes in recent procedures. Learning curves are rapidly achieved with operative times decreasing with each surgery (Fig. 2).
In conclusion, robotic-hybrid choledochal cyst excision with Roux-en-Y hepaticojejunostomy can be considered as an emerging approach to reduce anastomosis-related complications compared to laparoscopic surgery. There are limitations to this study that are mainly a result of its retrospective nature and the small number of cases. However, we believe that while a longer operative time is needed in robotic surgery, it tends to show less biliary complications and overall surgical complications than laparoscopic surgery. We believe that with current rapid learning curves and growing expertise, the operative time will be rapidly shortened. Although there are case reports of robotic surgery in choledochal cyst excision, this is the first study to report more than 10 serial cases of robotic hepaticojejunostomy and to compare it with its laparoscopic counterpart. However, larger, prospective, randomized, controlled trials are needed for comparing laparoscopic and robotic approaches.
Figures and Tables
References
1. Wiseman K, Buczkowski AK, Chung SW, Francoeur J, Schaeffer D, Scudamore CH. Epidemiology, presentation, diagnosis, and outcomes of choledochal cysts in adults in an urban environment. Am J Surg. 2005; 189:527–531.

2. Lee SE, Jang JY, Lee YJ, Choi DW, Lee WJ, Cho BH, et al. Choledochal cyst and associated malignant tumors in adults: a multicenter survey in South Korea. Arch Surg. 2011; 146:1178–1184.
3. Sastry AV, Abbadessa B, Wayne MG, Steele JG, Cooperman AM. What is the incidence of biliary carcinoma in choledochal cysts, when do they develop, and how should it affect management. World J Surg. 2015; 39:487–492.

4. Urushihara N, Fukuzawa H, Fukumoto K, Sugiyama A, Nagae H, Watanabe K, et al. Totally laparoscopic management of choledochal cyst: Roux-en-Y Jejunojejunostomy and wide hepaticojejunostomy with hilar ductoplasty. J Laparoendosc Adv Surg Tech A. 2011; 21:361–366.

5. Jang JY, Kim SW, Han HS, Yoon YS, Han SS, Park YH. Totally laparoscopic management of choledochal cysts using a four-hole method. Surg Endosc. 2006; 20:1762–1765.

6. Tang ST, Yang Y, Wang Y, Mao YZ, Li SW, Tong QS, et al. Laparoscopic choledochal cyst excision, hepaticojejunostomy, and extracorporeal Roux-en-Y anastomosis: a technical skill and intermediate-term report in 62 cases. Surg Endosc. 2011; 25:416–422.

7. Jang JY, Yoon YS, Kang MJ, Kwon W, Park JW, Chang YR, et al. Laparoscopic excision of a choledochal cyst in 82 consecutive patients. Surg Endosc. 2013; 27:1648–1652.

8. Tanaka M, Shimizu S, Mizumoto K, Yokohata K, Chijiiwa K, Yamaguchi K, et al. Laparoscopically assisted resection of choledochal cyst and Roux-en-Y reconstruction. Surg Endosc. 2001; 15:545–552.

9. Senthilnathan P, Patel ND, Nair AS, Nalankilli VP, Vijay A, Palanivelu C. Laparoscopic management of choledochal cysttechnical modifications and outcome analysis. World J Surg. 2015; 39:2550–2556.

10. Hwang DW, Lee JH, Lee SY, Song DK, Hwang JW, Park KM, et al. Early experience of laparoscopic complete en bloc excision for choledochal cysts in adults. Surg Endosc. 2012; 26:3324–3329.

11. Palanivelu C, Rangarajan M, Parthasarathi R, Amar V, Senthilnathan P. Laparoscopic management of choledochal cysts: technique and utcomes: a retrospective study of 35 patients from a tertiary center. J Am Coll Surg. 2008; 207:839–846.
12. Margonis GA, Spolverato G, Kim Y, Marques H, Poultsides G, Maithel S, et al. Minimally invasive resection of choledochal cyst: a feasible and safe surgical option. J Gastrointest Surg. 2015; 19:858–865.

13. Akaraviputh T, Trakarnsanga A, Suksamanapun N. Robot-assisted completeexcision of choledochal cyst type I, hepaticojejunostomy and extracorporealRoux-en-y anastomosis: a case report and review literature. World J Surg Oncol. 2010; 8:87.

14. Kang CM, Chi HS, Kim JY, Choi GH, Kim KS, Choi JS, et al. A case of robot-assisted excision of choledochal cyst, hepaticojejunostomy, andextracorporeal Roux-en-y anastomosis using the da Vinci surgical system. Surg Laparosc Endosc Percutan Tech. 2007; 17:538–541.
15. Choi SB, Choi SY. Current status and future perspective of laparoscopic surgery in hepatobiliary disease. Kaohsiung J Med Sci. 2016; 32:281–291.

16. Farello GA, Cerofolini A, Rebonato M, Bergamaschi G, Ferrari C, Chiappetta A. Congenital choledochal cyst: video-guided laparoscopic treatment. Surg Laparosc Endosc. 1995; 5:354–358.
17. Stefanidis D, Wang F, Korndorffer JR Jr, Dunne JB, Scott DJ. Roboticassistance improves intracorporeal suturing performance and safety in the operating room while decreasing operator workload. Surg Endosc. 2010; 24:377–382.
18. Moorthy K, Munz Y, Dosis A, Hernandez J, Martin S, Bello F, et al. Dexterity enhancement with robotic surgery. Surg Endosc. 2004; 18:790–795.

19. Heemskerk J, van Gemert WG, de Vries J, Greve J, Bouvy ND. Learning curves of robot-assisted laparoscopic surgery compared with conventional laparoscopic surgery: an experimental study evaluating skill acquisition of robotassisted laparoscopic tasks compared with conventional laparoscopic tasks in inexperienced users. Surg Laparosc Endosc Percutan Tech. 2007; 17:171–174.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download