Abstract
Caroli disease is a rare congenital disorder characterized by nonobstructive dilatation of intrahepatic ducts. In cases with symptomatic intrahepatic manifestations, treatment should correspond to the type with hepatic resection for localized disease and transplantation for diffuse forms. If possible, complete resection of the cysts can cure the symptoms and avoid the risk of malignancy. A 66-year-old woman presented to Wuxi Xishan People's Hospital with recurrent intermittent upper quadrant abdominal pain. Further examinations suggested the diagnosis of Caroli disease limited to the left hepatic lobe. She underwent laparoscopic hepatectomy. Pathological examination confirmed the diagnosis of Caroli disease, and no malignancy was found. There were no immediate complications and no long-term complications after one and one-half years of follow-up. Laparoscopic hepatectomy could be a feasible, safe treatment option for localized Caroli disease.
Caroli disease is a rare benign congenital disorder characterized by dilation of the intrahepatic bile ducts. It is characterized by multifocal congenital dilatations of the intrahepatic bile ducts, which may be diffuse or limited and present in a sac form that produces cystic structures that communicate with the biliary tree. It corresponds to a type V choledochal cyst, as classified by Todani [1]. The clinical symptoms of Caroli disease include right upper quadrant abdominal pain, jaundice, and recurrent cholangitis [2]. Patients with Caroli disease have also been shown to be at risk for intrahepatic cholangiocarcinoma [3]. Diagnosis is usually established by ultrasound, CT, and magnetic resonance cholangiopancreatography (MRCP) [4]. Meanwhile, the treatment of Caroli disease is still controversial. According to the type of bile duct cyst, surgical procedures include Roux-en-Y hepaticojejunostomy and variable types of hepatic resection. Liver transplantation (LT) should be considered an effective treatment modality for patients with Caroli disease [5]. Recent studies indicate higher percentages of patients with localized disease [6]. Liver resection (LR) for unilobar disease achieved excellent long-term outcomes and survival [7]. However, laparoscopic hepatectomy, which is a new option for LR [8], is still not broadly used for the treatment of Caroli disease. In this report, we present laparoscopic hepatectomy for a case of Caroli disease limited to the left lobe.
The patient's information released was permitted after discussion by the hospital ethics committee.
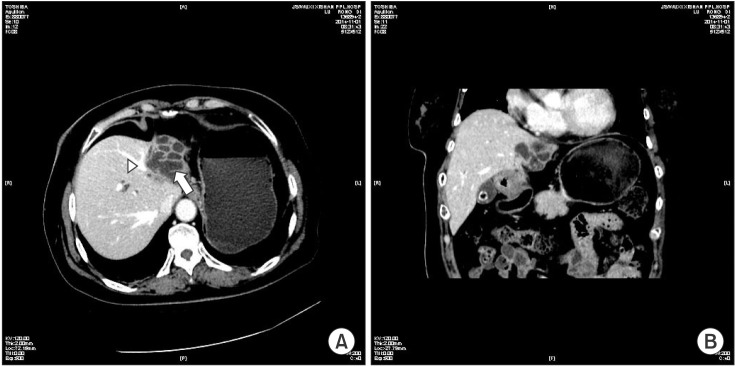
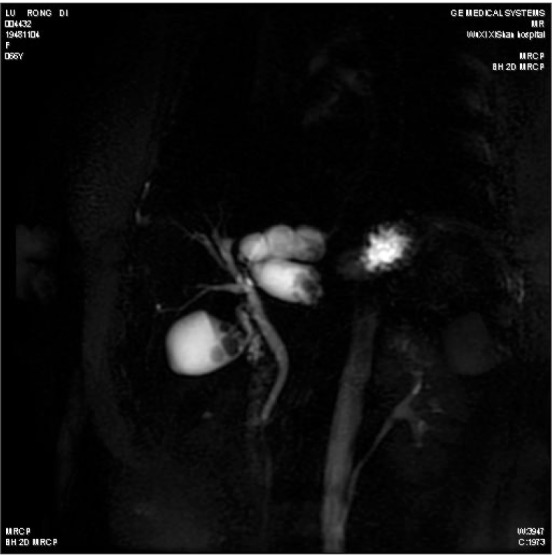
A 66-year-old woman with recurrent intermittent upper quadrant abdominal pain visited our hospital for further evaluation and treatment. Physical examination and initial vital signs were as follows: body temperature, 37.0℃; pulse rate, 66 beats/min; respiratory rate, 18 breaths/min; and blood pressure, 140/90 mmHg. Her height and body weight were 158 cm and 66 kg. She had a 10-year history of hypertension with good blood pressure control from oral Valsartan (40 mg/day). Her familial history was unremarkable. Laboratory examinations showed a low white blood cell count of 3,920/µL, a hemoglobin level of 11.8 g/L, and a platelet count of 124,000/µL. The liver function test results were as follows: serum aspartate transaminase: 14 U/L; alanine transaminase: 19 U/L; alkaline phosphatase: 88 IU/L; gamma-glutamyl transferase: 16 U/L; total bilirubin: 4.05 µmol/L; albumin, 35.7 g/L; and international normalized ratio: 0.93. CA 19-9 and α-FP were assayed for a malignancy workup, with results of 16.35 U/mL and 2.61 ng/mL, respectively. The results for viral markers including HBV surface antigen and anti-HCV were negative. Abdominal CT revealed an atrophic left lobar and dilated bile duct with the middle hepatic vein close to the cystic lesion (Fig. 1). Abdominal MRCP revealed irregular intrahepatic bile duct dilatation (IHBDD) of the left lobe with the left hepatic duct obstructed, while the common bile duct and right intrahepatic bile duct were normal (Fig. 2). However, we found that the irregular cystic dilatation of the bile duct was limited to the left liver and contained stones inside the cysts. No obvious abnormal dilated bile duct was found in the right liver. The common bile duct and the hepatic duct were normal, and no obvious dilatation was found. This patient was diagnosed with Caroli disease (type V). The surgical indication for the patient was explicit. However, the treatment prescription required consideration of the cystic wall being adjacent to the middle hepatic vein, the left hepatic atrophy and structure disorder, and the observation that the left hepatic vein was not visible. Although complete resection of the cysts may be a curative treatment for unilobar Caroli disease, this treatment was impossible for this patient due to the close adherence of the middle hepatic vein to the cystic wall. Therefore, we decided to perform laparoscopic left LR for the patient, while preserving a partial cystic wall close to the middle hepatic vein.
The standard laparoscopic equipment used to perform laparoscopic hepatectomy included a 30° 5-mm laparoscope, a hook dissector, 5-mm laparoscopic forceps, a 5-mm atraumatic grasper, a 10-mm GIA (Johnson & Johnson Medical, Shanghai, China), 5-mm harmonic (Johnson & Johnson Medical) and 10-mm locking pliers.
The conventional fully laparoscopic multiport approach was adopted. The patient was placed in a supine position, and the surgeon stood on the right side. Under general anesthesia, five 5- to 10-mm incisions were made in a “U” configuration. Division of the liver parenchyma was performed with Harmonic or Endo-GIA. Large pedicles were stapled or clipped.
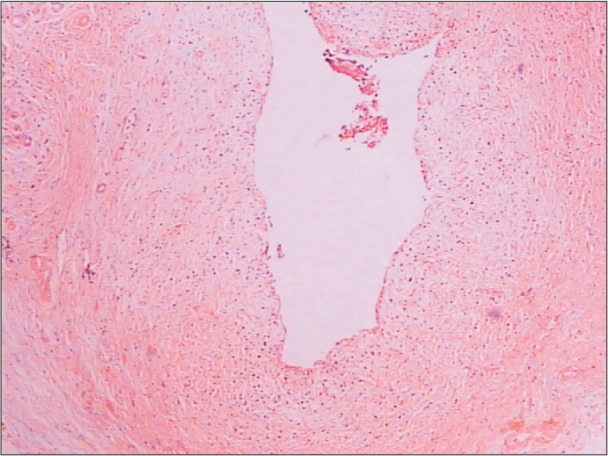
Upon surgical exploration, the left lobe of the liver was found to be atrophied, and the right liver had developed compensatory hyperplasia with a red-brown and smooth surface. However, the left liver lobe was severely adherent. We gradually dissected the adhesion using harmonic pliers and exposed the atrophic left lobe (5 cm × 6 cm × 2 cm). The gallbladder was approximately 7 cm × 4 cm × 2 cm in size and was filled with bile and gallstones. Through intraoperative exploration, we confirmed the diagnosis of Caroli disease, limited to the left lobe of the liver. We obtained a biopsy from the edge of the lesion and performed a rapid intraoperative pathological examination to exclude malignant tumor. We then decided to perform a laparoscopic left liver and gallbladder resection. The difficulty was that the lesion was close to the middle hepatic vein. We opened the cysts and resected most of the lesion while retaining part of cystic wall close to the middle hepatic vein. After laparoscopic left half-liver and gallbladder resection, the liver lesion tissue and gallbladder were removed completely from the abdominal cavity. Histopathologic findings showed congenital dilatation of the intrahepatic bile ducts, confirming the preoperative diagnosis of Caroli disease (Fig. 3). Histopathology of the resected specimen revealed large, cystic dilations of the large intrahepatic bile ducts. This patient was seen regularly every 3 months at the outpatient department. There was no recurrence of abdominal pain, and no complications were discovered after 18 months of follow-up.
Caroli disease is a rare congenital condition characterized by nonobstructive dilatation of intrahepatic ducts. In Caroli syndrome, there is associated congenital hepatic fibrosis. The early diagnosis of the disease and differentiation of types I and II are of extreme importance to patient survival. LR for unilobar and LT for diffuse bilobar congenital IHBDD complicated by cholangitis and/or portal hypertension achieved excellent long-term patient outcomes and survival. Because of the poor prognosis of cholangiocarcinoma and the sizeable morbidity-mortality after LT, timely indication for surgical treatment is of major importance.
The primary treatment of Caroli disease is surgery, such as segmentectomy, lobectomy, or hepaticojejunostomy, determined by the range of cystic formation. In patients with Caroli disease limited to one lobe of the liver without concurrent cirrhosis, hepatic resection with or without Roux-en-Y cholangiojejunostomy remains the treatment of choice.
In recent years, one study [9] assessed the clinical presentation and long-term results of surgical management of congenital IHBDD in a multicenter setting and reported a 5-year overall survival rate of 88.5% (88.7% after LT). Another study [10] reported that resection might adequately treat most individuals with Caroli disease, whereas transplantation is required for Caroli syndrome patients due to associated hepatic fibrosis.
Although reported numbers in the literature are low, there is broad consensus that hepatic resection is the therapy of choice for patients with localized forms of type V cysts. With the development of laparoscopic surgery, LH has become a feasible treatment for liver disease. However, the treatment of Caroli disease with LH has still not been reported. In our report, the patient was diagnosed with unilobar Caroli disease and underwent laparoscopic LR due to the minimal invasion. After 18 months of follow-up, no recurrent pain or cholangitis were observed in the patient.
In this case report, we described an extremely rare case of Caroli disease limited to the left hepatic lobe. Imaging findings of this case were similar to those of hepatolithiasis and cholangiocarcinoma. Liver fibrosis was not found in the right liver lobe, and the liver functional reserve was assessed as sufficient. Preoperative examination initially ruled out the possibility of malignancy. Additionally, in consideration of minimally invasive surgery, we performed laparoscopic surgery for the patient. The postoperative pathology also confirmed the diagnosis of Caroli disease. The operation also achieved the expected effect, which was improvement of the patient's symptoms. However, the residual part of the capsule may still have a certain risk of malignancy. Therefore, long-term follow-up is very important to avoid this risk.
To our knowledge, laparoscopic surgery for the treatment of Caroli disease is a new effort. As a minimally invasive technique, laparoscopic surgery could be used for the treatment of Caroli disease with several advantages, such as better intraoperative exploration, improved quality of life, and diagnostic utility.
References
1. Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977; 134:263–269. PMID: 889044.
2. Sato Y, Ren XS, Nakanuma Y. Caroli's disease: current knowledge of its biliary pathogenesis obtained from an orthologous rat model. Int J Hepatol. 2012; 2012:107945. PMID: 22007315.

3. Jang MH, Lee YJ, Kim H. Intrahepatic cholangiocarcinoma arising in Caroli's disease. Clin Mol Hepatol. 2014; 20:402–405. PMID: 25548748.

4. Wang ZX, Li YG, Wang RL, Li YW, Li ZY, Wang LF, et al. Clinical classification of Caroli's disease: an analysis of 30 patients. HPB (Oxford). 2015; 17:278–283. PMID: 25327281.

5. Harring TR, Nguyen NT, Liu H, Goss JA, O'Mahony CA. Caroli disease patients have excellent survival after liver transplant. J Surg Res. 2012; 177:365–372. PMID: 22640887.

6. Ulrich F, Pratschke J, Pascher A, Neumann UP, Lopez-Hanninen E, Jonas S, et al. Long-term outcome of liver resection and transplantation for Caroli disease and syndrome. Ann Surg. 2008; 247:357–364. PMID: 18216545.

7. Madariaga JR, Iwatsuki S, Starzl TE, Todo S, Selby R, Zetti G. Hepatic resection for cystic lesions of the liver. Ann Surg. 1993; 218:610–614. PMID: 8239774.

8. Goh BK, Chan CY, Lee SY, Lee VT, Cheow PC, Chow PK, et al. Laparoscopic liver resection for tumors in the left lateral liver section. JSLS. 2016; 20:pii: e2015.00112. DOI: 10.4293/JSLS.2015.00112.

9. Mabrut JY, Kianmanesh R, Nuzzo G, Castaing D, Boudjema K, Letoublon C, et al. Surgical management of congenital intrahepatic bile duct dilatation, Caroli's disease and syndrome: long-term results of the French Association of Surgery Multicenter Study. Ann Surg. 2013; 258:713–721. discussion 721. PMID: 24121258.
10. Moslim MA, Gunasekaran G, Vogt D, Cruise M, Morris-Stiff G. Surgical management of Caroli's disease: single center experience and review of the literature. J Gastrointest Surg. 2015; 19:2019–2027. PMID: 26302876.

Fig. 1
CT findings. (A) Enhanced transverse CT reveals grape-like dilated left intrahepatic bile ducts (arrow) with middle hepatic vein close to capsule wall (arrowhead). (B) Sagittal plane of enhanced CT shows atrophic left lobe with dilated intrahepatic bile ducts and gallbladder calculus.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download